While much of the healthcare industry was eager to put 2020 behind it, the new year brings its own challenges, concerns, and promises. Trends in the three main categories of new Biden administration policy, care delivery, and healthcare technology will shape 2021, with key issues including the long-term effects of COVID-19, future emergency preparedness, and the outlook for the Affordable Care Act (ACA). Healthcare leaders can prepare for this pivotal year by understanding critical areas to watch within these categories and how events, activities, and political appointments will affect the healthcare ecosystem.
After a turbulent, COVID-19 dominated 2020, healthcare leaders, policymakers, and the U.S. public are eager to know what 2021 holds. Pressing concerns include persisting and emerging pandemic challenges, the long-term effects of COVID-19, future emergency preparedness, and how the Biden administration will impact healthcare—notably, the future of the Affordable Care Act (ACA).
2021 healthcare trends fall into three main categories: healthcare policy, care delivery, and technology. The industry can prepare for the future by understanding critical areas to watch within these categories and which events and activities may affect the healthcare ecosystem.
With President Joe Biden’s inauguration on January 20, the healthcare industry will be watching for the new administration’s priorities around the ACA and its COVID-19 plan, as well as who will be on the administration’s healthcare team and on which policies it focuses.
While ACA repeal was a constant threat under the last administration, the Act looks more secure following recent developments. The ACA’s future likely hinges on the constitutionality of the individual mandate and potential severability under the California versus Texas case, which the U.S. Supreme Court is currently considering.
The California versus Texas case came to the Supreme Court from a federal appeals court. If the Supreme Court affirms the appeals court ruling, the case will go back to the federal district court to decide on the issue of severability of the individual mandate from the rest of the ACA. At the November 2020 oral argument, it looked like the Supreme Court, including one or more of the new justices, was inclined to honor the doctrine of severability, making it less likely the ACA will face complete repeal. Additionally, the new slim Democratic majority in the Senate (thanks to the Georgia runoff) makes it likely that Congress would fix the constitutional problem by reinstating the mandate with a nominal penalty.
The ACA also includes many popular, patient-focused programs, making it less likely to face repeal. These include the protection for individuals with pre-existing conditions, parental healthcare coverage for children up to age 26, and greater access to health insurance through the exchanges. Popular on the healthcare-industry side are value-based care (VBC) and the Medicare Shared Savings Program. These programs and are likely to continue, regardless of the ACA’s future, because they enjoy bipartisan support.
The Biden administration may also take steps to strengthen aspects of the ACA, such as making more resources available for demonstration projects, and raising tax credits and subsidies to purchase insurance on the exchanges. These actions may be attainable within the framework of the existing law and wouldn’t require new legislation.
The Biden administration has made a number of appointments and nominations to fill healthcare positions, with notable roles including the following:
These appointments and nominations point to a strong emphasis on COVID-19 recovery and vaccine distribution and coordination. For example, Fauci remains as the Director of the National Institute of Allergies and Infectious Diseases, and there’s now a COVID-19 data director (Shahpar), indicating this administration will emphasize data and reporting. Also evident in these appointments is a Biden administration focus on health equity and healthcare disparities—particularly with Nunez-Smith as the first Equity Task Force Chair for COVID-19.
Democratic control in the Senate will also impact healthcare. For example, Washington state Senator Patty Murray will chair the Senate Committee on Health, Education, Labor, and Pensions. She has advocated for a more robust federal response on COVID-19. And Senator Ron Wyden, Oregon, leads the Finance Committee and has pushed for drug pricing reform and drug price negotiation.
COVID-19 tops the Biden administration’s priorities and will likely do so for the foreseeable future. Vaccine distribution will dominate the first six months of 2021, with federal effort focused on the expansion of testing, contact tracing, and better public health reporting from states and localities up to the CDC and other federal agencies
Data collection and expanded use of data will be critical to the Biden administration’s ongoing COVID-19 response. The administration proposes funding to states and localities for their public health response infrastructure (including registries, reporting, surveillance, and dashboards). The administration also plans to expand the availability of platforms that ensure patient data security and to expand data use rights to enable use and disclosure for research and surveillance. These actions will accelerate research on effective clinical interventions and treatment pathways, expand patient monitoring, and help public health reporting and tracking vaccine distribution.
The new administration will also likely push to expand healthcare program funding, including ACA programs and value-based care, and expansion of coverage. The Senate may use the budget reconciliation process to push through a COVID-19 relief package and some healthcare-related policies. Budget reconciliation requires only a majority vote, as contrasted to a supermajority vote for regular legislation. However, budget reconciliation can only happen a couple of times per year, generally speaking, when the budget is up for approval, and is limited to budget-related items.
Budget reconciliation pushed through some provisions of the ACA in 2010. While some of the ACA expansions, increased subsidies, and tax credits could occur through budget reconciliation, this process would not be available for bigger picture health policy issues that are unrelated to the federal budget. These bigger picture items include issues such as a public option, Medicare for all, and lowering the Medicare eligibility age to 60.
The following policy priorities, if the administration adopts them, would also help the nation better prepare for future emergencies at the health system, local, state, and national levels:
The Biden administration has released its National Strategy for the COVID-19 Response and Pandemic Preparedness, a $1.9 trillion-dollar plan, which Congress was debating as of early February 2021. Although Congress will likely approve a reduced COVID-19 relief package, some notable features of the proposal include the following:
Like healthcare policy, COVID-19 will continue to drive care delivery in 2021. The pandemic will shape healthcare moving forward, with the impact and toll of the virus factoring in care delivery for a long time. Critical areas of concern include how COVID-19 continues to impact health systems, clinicians, providers, patients, and VBC programs and healthcare delivery changes to prepare for future pandemics.
As of early February 2021, the Washington Post reported that COVID-19 deaths had reached over 2 million worldwide. This number included more than 444,00 deaths in the United States and more than 100 million cases worldwide.
In Figure 1, below, from Center for Disease Control (CDC), the bottom line shows the expected deaths in the United States for any given year. As of January 23, 2021, the actual observed numbers of deaths were well above the threshold for excess deaths.

The above numbers represent a tremendous burden on COVID-19 victims and their loved ones and the U.S. healthcare workforce—with both physical and mental impacts. Those working in high-risk departments (e.g., emergency departments (EDs) and ICUs) with infected patients, sometimes with suboptimal PPE access, have felt the most significant impact and experienced the highest mortality. This loss will impact the industry indefinitely. To fill in frontline gaps, many organization team members who usually focus on process improvements in care settings are doing frontline work. This matter reflects the financial impact and the shortage of staff due to COVID-19.
The CDC has responded to the pandemic’s toll with Project Firstline, an initiative for communities and health frontline workers to promote infection prevention and infection control. The Health Research and Education Trust, American Medical Association, and the American Nurses Association co-sponsor the initiative, which provides practical tools and resources to implement infection control protocols in every patient interaction.
The influx of COVID-19 patients has driven massive change in the healthcare delivery system. According to the Kaufmann Hall National Hospital Flash Report, many individuals are avoiding routine and elective interactions with healthcare, with consequences including a drop in weekly screening for breast cancer, colon cancer, and cervical cancer of between 86 and 94 percent, according to the Kaufmann Hall National Hospital Flash Report: December 2020. Foregoing screenings and other preventive care will have a long-term impact on healthcare, as early detection and intervention will decrease.
Kaufmann Hall’s findings also showed discharges volumes were down in terms of elective discharges, as were operating room minutes, elective procedures and ED visits in general, and revenues were dramatically down at 14 percent per adjusted discharge. Outpatient revenue (a source of loss for elective work) was down 6 percent compared to an inpatient revenue drop of 1 percent.
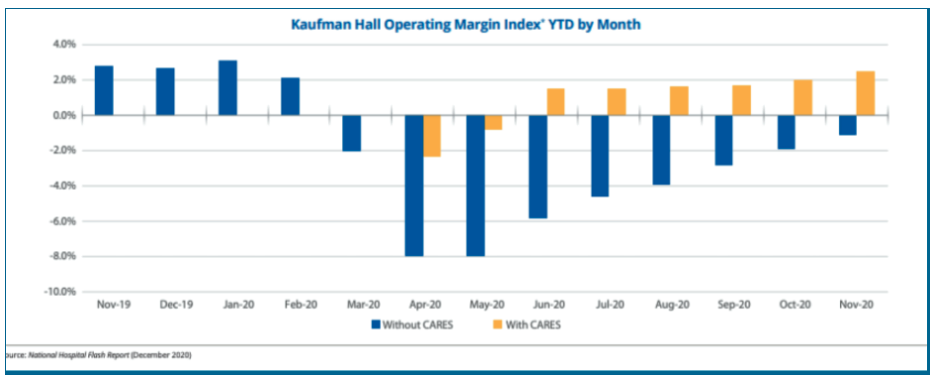
As healthcare consumers have made fewer routine and elective visits, organizations have felt a financial impact, hitting ambulatory and hospital settings. Operating margins have fallen dramatically, with a 5 percent drop in margins nationwide by the end of 2020. The CARES Act provider relief has given some support to the healthcare delivery system, but 2020 margins still declined nearly 2% compared to 2019. (Figure 2, Kaufman Hall National Flash Report: December 2020).
In 2021, on the other side of COVID-19’s tolls, is a light at the end of the tunnel: the COVID-19 vaccine. By the last week of January, the United States averaged around 1.5 million vaccinations a day.
Despite encouraging vaccination numbers, distribution is meeting challenges. According to the Kaiser Family Foundation, some Americans are hesitant to receive the vaccine, a preference that appears to correspond to political orientation, ethnicity, age, and urban or rural setting (Figure 3, Kaiser Family Foundation).
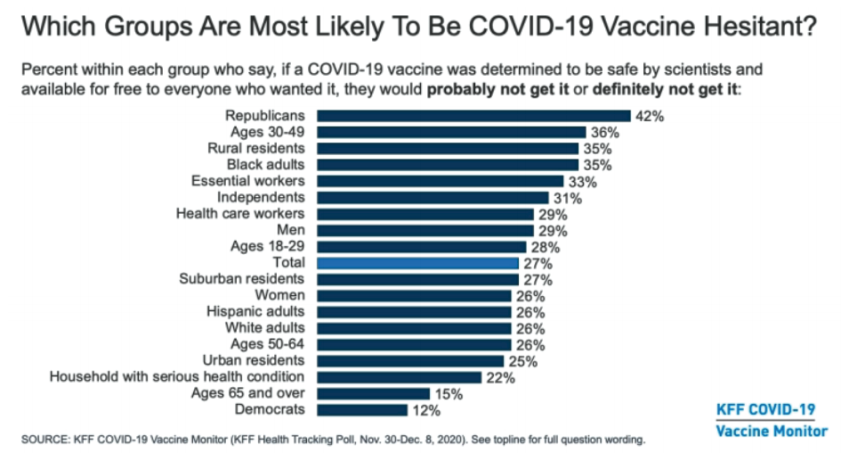
As of December 2020, people in their 50s and older, urban residents, those with a household member with a health condition, Democrats, and Hispanic adults appeared more likely to get the vaccine, and women were more likely than men. Interestingly, healthcare workers were a little cautious, with 29 percent hesitancy.
One of the best chances for more comprehensive COVID-19 vaccination among U.S. populations is for primary care physicians to become a recognized information source about the vaccine. According to a Kaiser Family Foundation poll, 85 percent of patients regard their healthcare provider as the most trusted source of information about the vaccine.
As an extension of COVID-19’s far-reaching impact across healthcare, the pandemic has also affected healthcare technology, accelerating some changes and dramatically demonstrating how nimble the industry can be. Healthcare data analytics, artificial intelligence, and telemedicine capabilities have massively expanded to support the pandemic response and recovery, a trend that will likely continue to propel healthcare technology.
COVID-19 made the need to leverage data and advanced analytics central to many health systems. Expansion of those capabilities to meet the demand for real-time data or close to real-time data has been dramatic.
For example, hospital administrators are looking at their COVID-19 dashboards hourly and using data to update their business intelligence reporting tools. Previously, the most useful artificial intelligence applications (AI) and machine learning (ML) were likely predicting revenue cycle trends, with attempts for more sophisticated use, such as reading imaging with AI stalled. Now, COVID-19 has compelled innovation to bring advanced analytics to the forefront of disease response, using predictive models to track the virus and estimate the risk of COVID-19 to patients with severe symptoms, enabling more effective treatment.
Health systems are rapidly expanding their support for a digital workforce, including the chief information officer (CIO) role. The CIO is playing a larger role in an organization’s strategy, risk management, and cybersecurity. The EHR has expanded and will likely continue to evolve with digital and voice assistance and natural language processing. With such clinical IT developments, including augmented reliable and wearable technology so that patients can make decisions in real-time with real data, the digital workforce and CIO roles stand to continue to grow.
COVID-19 created an urgent need for telehealth to care for patients outside of the clinic or office setting and offset financial losses due to reduced ambulatory visits. According to a McKinsey study, the number of patients using telehealth increased from 11 to 46 percent in 2020, with growth likely to continue. McKinsey predicts telehealth could account for 20 percent, or $250 billion, of U.S. healthcare spending in the near future.
Though the transition towards expanded telehealth is in motion (including policy changes around accessibility and reimbursement), healthcare technology will still need to adapt to accommodate the continuing shift. Health systems need greater integration with existing technology platforms and strategies to address cybersecurity and privacy concerns. In this way, telehealth is another area that will increase demands on the digital workforce and healthcare CIOs.
The healthcare industry begins 2021 forever-changed by COVID-19 and still trying to recover and find its direction. While healthcare leaders and professionals are recuperating from the significant losses of 2020, they will continue to face challenges as the pandemic continues and the recovery begins. A new federal administration will look to lessons learned so far during the pandemic, available data, and industry experts, to accelerate vaccine distribution and get the nation back on its feet. Changes in care delivery models and technology have accelerated, and will continue to, as a result of the pandemic response and recovery. Perhaps a silver lining is that the healthcare industry, patients, and providers, would continue to benefit from these positive developments in care delivery and technology.
Would you like to learn more about this topic? Here are some articles we suggest: