Improving health equity is gaining traction as a healthcare delivery imperative. Yet, while equity is indivisible from healthcare quality, many initiatives targeting disparities fall short. Organizations too often rely solely on leader and stakeholder passion and perseverance without sufficiently leveraging data and analytics to understand, measure, and support equity improvement efforts. It’s time for the industry to pursue equitable care with the same resources it uses in other key dimensions, such as safety and efficacy—by leveraging data. A data-driven approach to equity opens health system’s most advanced predictive resources to equity efforts, thereby driving massive, measurable, data-informed improvement that benefits all.

Beginning in 2020, the dramatically higher COVID-19 infection and morbidity rates for communities of color compared to white communities heightened awareness about the human and financial costs of inequitable healthcare. In response, more healthcare organizations are prioritizing advancing health equity and investing in diversity, equity, and inclusion programs and leadership—all of which require data to showcase the most significant gaps and healthcare disparities.
Equity is one of six quality dimensions in healthcare and has been since the National Academy of Medicine (NAM) published “Crossing the Quality Chasm” in 2001. Since 2018, the Center for Medicare and Medicaid Services (CMS) has presented Health Equity Awards to recognize organizations committed to overcoming disparities through a strategic approach to identifying, prioritizing, and addressing improvement areas. Effective quality assessments include equity as a requisite.
According to NAM, quality healthcare must be safe, effective, patient centered, timely, efficient, and equitable. NAM defines equitable as “Providing care that does not vary in quality because of personal characteristics including gender, ethnicity, geographic location, and socioeconomic status.”
Yet, healthcare organizations often rely solely on passion and perseverance to address equity. There is a gap in reliance on analytics and augmented intelligence (AI) to identify and address inequitable care. As an industry, would not pursue improvement in the other dimensions, such as safety and effectiveness, without relying on data, and we must close the equity gaps by leveraging data.
NAM’s statement on quality care provides a hint as to how to close the gap. If the industry changes “care that does not vary…” to “care that cannot be predicted by…,” we open the possibility of using an AI toolset. Health equity becomes the predictive model we hope we would not need to build. We feel “good” about being able to predict a patient’s readmission based on their medication complexity (we might intervene with medication simplification, support, or education). However, we do not feel good about higher readmission risk due to personal characteristics, to include primary spoken language or zip code.
All healthcare organizations benefit from data to improve health equity and formalize and operationalize equal access to and delivery of healthcare for all patients.
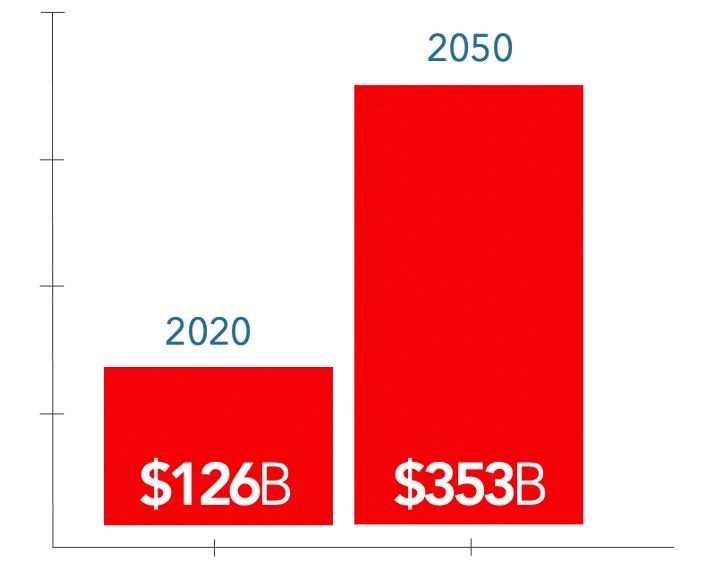
Along with improving clinical outcomes, bolstering health equity improves health systems’ operational and financial performance. A 2016 IHI white paper projects that, left unchecked, health disparities could reach an economic burden in the United States of $353 billion by 2050 (Figure 1).
COVID-19 demonstrated that U.S. health systems are falling short in health equity. Vulnerable communities have borne the pandemic’s brunt from infection rates and risk of death to access to treatment, testing, and vaccination.
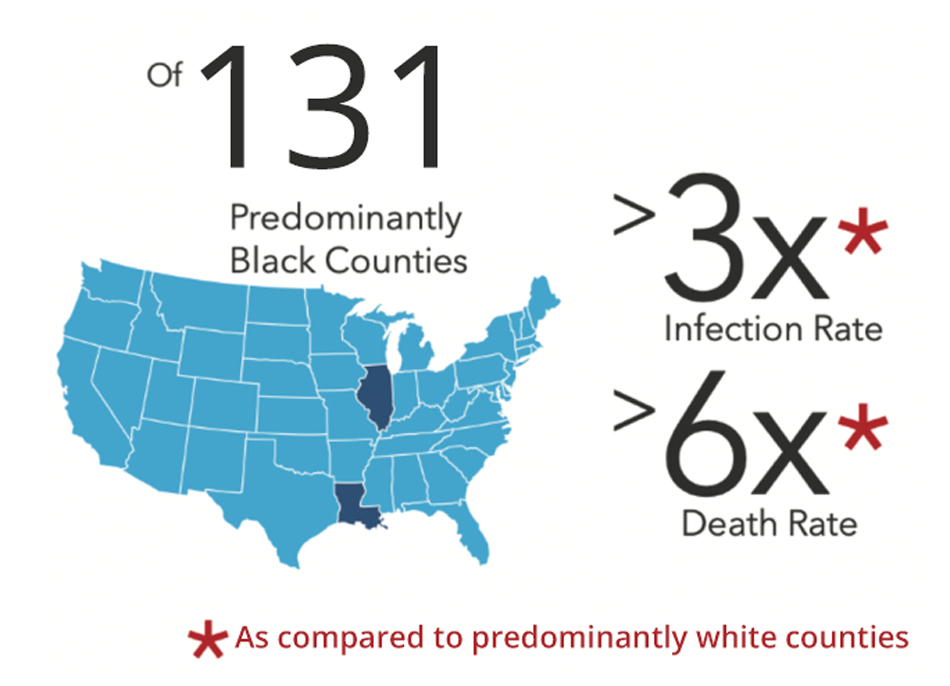
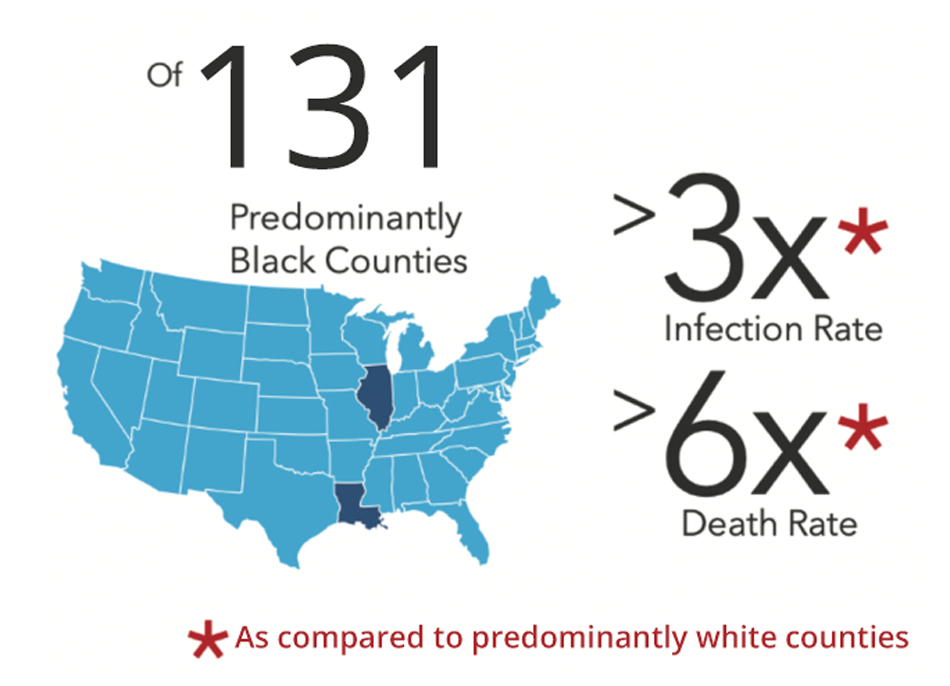
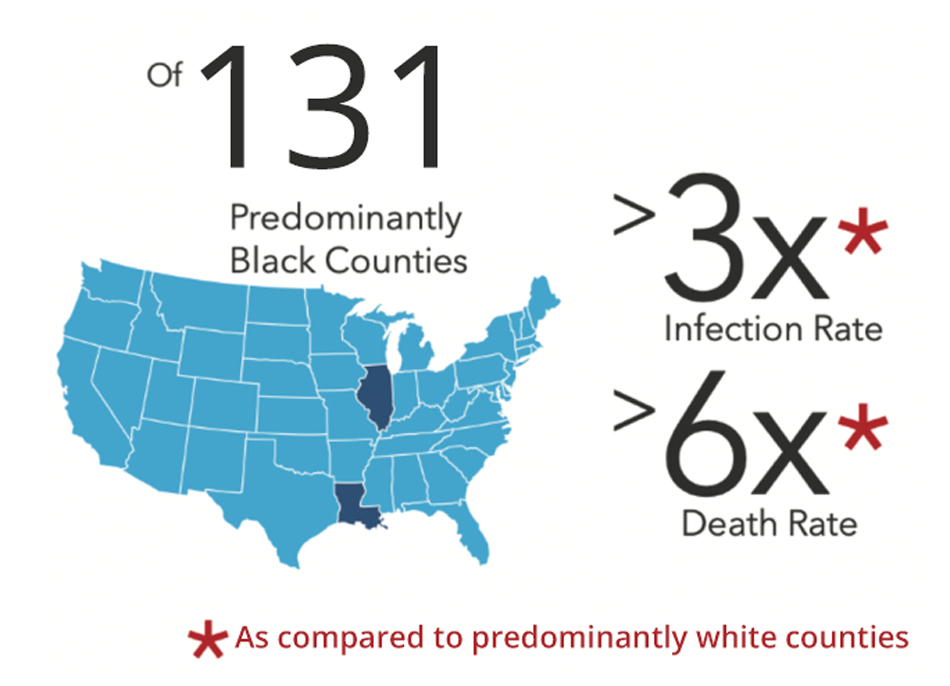
For example, based on early pandemic data reported in JAMA, residents in predominantly Black counties in the United States experienced three times the COVID-19 infection rate and six times the death rate of chiefly white counties (Figure 2).
Not surprisingly, the disparity in COVID-19 impact among Black populations reflects decades of documented disparities in healthcare. A report from the Kaiser Family Foundation states that the Black and American Indian or Alaska Native (AIAN) individuals continue to fare worse across most examined health status measures, including physical and mental health status (Figure 3). Meanwhile, Black and AIAN individuals’ infant mortality rate is roughly two times higher than for white individuals. Black teens and adults have a more than eight times higher HIV diagnosis rate, and Hispanic teens and adults have a more than three times higher HIV and AIDS diagnosis rate.

Healthcare disparities, including those related to COVID-19, are part of broader underlying social and economic inequities, making it more critical than ever for organizations to have data and analytics to understand the personal characteristics, goals, preferences, and circumstances of those they serve. Primary drivers for increased insights include the social determinants of health (SDOH), the conditions in which people are born, grow, live, work, and age—all areas healthcare data hasn’t traditionally captured. As COVID-19 further underscores health inequities between U.S. racial and ethnic groups, the industry can't ignore the demand for comprehensive patient data and open analytics.
Making better data-informed decisions is one of the first steps toward achieving greater equity—not just during a crisis like a pandemic but in everyday healthcare. A data-informed approach to health equity directs focus and rational accountability targets to secure resources and provides tools to optimize impact.
For example, Health Catalyst’s data-driven health equity solution, currently being piloted, combines an analytics framework with the services expertise to accomplish the following:
There is justified concern about AI exacerbating disparities if algorithms rely on biased assumptions or data that can reinforce inequities. At Health Catalyst, we share this concern. We also have found ways of using AI to reduce disparities. We do this by ensuring AI empowers organizations to identify where to focus their attention and resources.
Healthcare is accustomed to using predictive models, for example, to anticipate readmission or cardiovascular disease risk, based on clinical factors, such as comorbid burden, medication complexity, or genetics. Someone will likely heal more quickly from a splinter than a car accident.
We have identified a disparity if we can predict care or outcomes based on personal characteristics. When we fail to predict care or outcomes based on personal characteristics, including race, ethnicity, age, gender, sexual orientation, zip code and more, we have demonstrated health equity.
Approaching health equity as a prediction problem opens the entire predictive modeling toolbox to organizations wishing to reduce disparities but lacking quantitative support to pinpoint areas of improvement. This is an unexpected example of how high-quality data analytics replaces anecdotes and assumptions to drive massive, measurable, data-informed improvement.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download this presentation highlighting the key main points.