With the healthcare industry move towards value-based payment (VBP), financial executives must navigate a shift away from volume and embrace quality care as a key driver of financial health—particularly as accountable care, quality measures, shared savings, and bundled payments gain traction. To meet this ongoing quality-cost challenge, health systems must understand their progress in clinical quality measures and costs of delivering care, as clinical quality is an increasingly significant predictor of financial outcomes. While the traditional fee-for-service environment emphasized volume, today’s VBP paradigm puts quality ahead of older metrics.
 Download
Download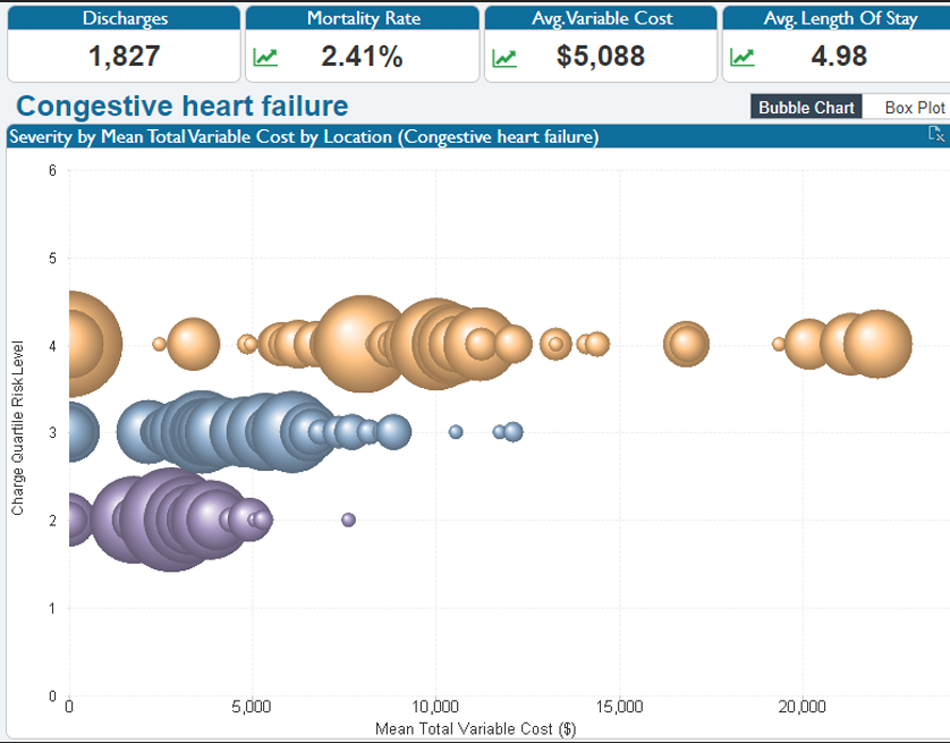
At first glance, creating a healthcare system that focuses on lowering costs seems counterintuitive in an environment that rewards quality improvements. But lowering costs while improving quality and combining the two to ensure a thriving bottom line is precisely the challenge today’s healthcare finance executives face in the shift towards value-based purchasing (VBP).
This two-pronged goal of lower cost and higher quality is, however, a winnable challenge, provided health systems have a thorough understanding of where they stand relative to clinical quality measures and the costs associated with delivering care. For finance executives, this understanding means factoring in clinical quality to predict the organization’s financial health, which is a significant paradigm shift from the traditional fee-for-service (FFS) reimbursement environment.
Under FFS, measuring volume was front and center for the finance team, and it’s still a key part of the equation today. Generally, healthcare has adapted to per-case payment methodology. But with payments also hinging on quality, focusing solely on old metrics (e.g., volume) won’t bring financial success, particularly in a world of accountable care, quality measures, shared savings, and bundled payments. Today’s focus must shift to lowering the costs while providing the highest quality care.
With the shift to VBP, the U.S. healthcare system faces its most significant transformation since the advent of managed care in the 1980s. Health system financial executives are in the thick of navigating the complexities of this change, tasked with helping their organizations determine exactly how to strategically approach the new reimbursement environment.
Questions financial executives must address as organizations move towards VBP include the following:
While each individual quality measure is a small item to track, the combination of quality measures coupled with an influx of new regulations heavily impacts the bottom line. Add to this complexity the fact that quality measures can and likely will change over time and each payer has the right to associate different penalties and incentives with them, and tracking develops into a very complicated proposition.
Quality measurement is just one of the complexities that VBP introduces to the process of organizational cost management. Understanding how clinical quality and other factors affect the bottom line requires financial executives to master the new lexicon, which pays and rewards providers based on outcome quality and patient satisfaction. Volume metrics alone can’t provide the insight organizations need to succeed under healthcare reform. Finance teams need to work with quality teams to develop dollar impact and prioritize which metrics to track.
To make sound decisions, finance executives need to track key metrics within VBP beyond volume for a full picture of a health system’s quality. These metrics include the following:
The CMS VBP program is self-funded via hospital eligibility for a penalty or a bonus for its scores in the four categories above with a cap of 2 percent.
Organizations should prepare to answer key metrics and determine who is accountable for results—including mortality rates for specific conditions, patient receipt of discharge instructions, and complication rates for hip/knee arthroplasty cases. Additional notable metrics should include the facility’s patient engagement score and rate of hospital-acquired infections.
The following measures also impact VBP:
Each of the above metrics carries potential penalties and/or incentives under the various CMS-sponsored payment innovation programs. Commercial payers have implemented similar programs to track quality metrics that impact the health of their insured members. These programs increase the number of measures organizations must monitor and improve.
Commercial payers rely on Healthcare Effectives Data and Information Set (HEDIS) measures set, a set of standardized performance metrics. Organizations that thrive in a value-based environment will routinely track these measures as part of their reporting and monitoring structure, rather than sponsor occasional studies of their performance in these areas.
Beginning in 2020, the COVID-19 public health emergency has impacted quality measures. In response, CMS has finalized a measures suppression policy to ensure providers are not penalized based on pandemic-affected data. CMS has revised baseline periods, excluded COVID-19 patients, and suspended measures temporarily.
For 2022, CMS will not make payment adjustments to hospitals in the VBP program. CMS will display the measures for public consumption. In 2023, CMS will suppress the measure for PSI 90 and pneumonia mortality. Also in 2023, CMS will eliminate the pneumonia readmission score and remove all COVID-19 patients from the remaining readmission measures. The agency will adjust the performance periods in the HAC program by truncating the periods for reporting in 2022 and 2023.
As clinical quality metrics have a growing impact on organizations’ bottom lines, healthcare financial executives face with new challenges: how to track, measure, and analyze these metrics and translate them into financial terms? The answer begins with data collection. However, using data isn’t as straightforward as it sounds. Significant barriers, such as the following, exist to leveraging data effectively to drive value-based decision making:
Traditionally, separate systems have housed financial and clinical data, making relevant data available only to the teams that needed it (e.g., the billing and clinical care teams). As such, financial data is often far removed from clinical data, making it difficult to understand the relationship between the two. In addition, many hospitals and health systems have a variety of transactional system siloes throughout the care continuum.
While numerous health systems have made headway in aggregating their clinical data to create longitudinal health records, the unstructured nature of clinical documentation (e.g., manually reviewing charts) often hampered efforts to track metric. Plus, clinical data aggregation alone does not incorporate the financial, operational, and patient-experience data an organization needs to fully visualize its quality/cost equation.
Healthcare data gathering and reporting processes are often outdated and insufficient for the complexities of the value-based environment. For example, the quality team may provide metrics on readmissions, HACs, and core measures for clinical processes, while finance is responsible for cost and payment data. Getting data from both parties may become a manual collection process.
The following are two significant drawbacks of outdated data gathering and reporting processes:
A typical scenario for gathering data for analysis may comprise the following five steps:
While digitized dashboards are convenient for executives, they require significant amount of manual work to pull the information together, which slows the process and leaves reports further from real time. Furthermore, analytics teams must update these reports on a regular basis.
Some health systems have adopted dashboard programs for point solutions that remove some of the manual effort. While these dashboards may provide insight about a targeted issue, they don’t link clinical, financial, operational, and patient experience data in the way that value-based decisions require. Because the solutions aren’t linked, individual users still must determine how to fit these reports together and make collective sense of them—in other words, dashboards lack the ability to drill into data and ask questions.
When team members throughout the organization access data in different ways and from multiple sources, inconsistency and variability among the data are common. For example, for two executives may present conflicting data about emergency department admissions or length-of-stay trends simply because they relied on different data collection methods. Inconsistencies like these can lead users to distrust the data. And of decision-makers don’t trust the data, they can’t be sure they’re making the best decisions for the organization.
To overcome data trust challenges and successfully manage costs in a value-based environment, health systems can leverage their two most important assets for effecting cost and quality change: data and clinical teams. Finance executives provide leadership to actively assist in this effort.
The keys to successfully navigating the quality and cost demands of value-based care are as follows:
A cloud-based data platform, such as the Health Catalyst Data Operating System (DOS™) is the key to liberating clinical and financial data and linking it together for a full picture of trends and opportunities.
An effective platform in the value-based environment aggregates data from a wide variety of sources. It must accommodate all clinical and financial data tables involved with the programs the organization is trying to impact. The data platform also needs to include information from costing systems, including supply chain and labor productivity to calculate the true cost of an episode of care
With the data in hand, health systems must then determine how to use that information to meet cost and quality goals. Most organizations employ a top-down approach for driving change that relies on executive dashboards. However, multidisciplinary, permanent teams operating on the front lines of clinical care and using clinical and financial data to drive improvements support a more effective bottom-up approach.
The top-down approach that health systems commonly deploy consists of using executive dashboards to rank facilities, departments, and individuals based on their performance relative to defined benchmarks. This approach operates on the assumption that pressure from the top will drive change. However, a top-down strategy has several key drawbacks:
Organizations can drive sustainable improvement by forming multidisciplinary, permanent, frontline teams that leverage aggregated clinical and financial data. These frontline teams consist of clinicians, quality personnel, analysts, and technologists and receive support from a financial representative. This approach engages frontline personnel to drive quality improvement.
The frontline team is at the helm of the quality initiative. And to be truly effective, the team needs to report to a guidance team comprised of members of management who can eliminate roadblocks, prioritize work efforts, and set clear goals for the entire organization. The frontline team—those who are closest to the processes that need refinement—have the following responsibilities:
Just as finance needs to understand the impact clinical processes have on the bottom line, clinicians need to also understand the financial implications of their clinical decisions. Organizations involve clinicians in looking at both clinical and financial data by creating a learning culture in which clinical and financial personnel listen to each other and educate each other.
Integrated data informs this level of collaboration, enabling a health system to effect sustainable improvement in a value-based environment. Finance personnel present data to the clinical team to educate them on what the financial data means. Then, the clinical team can help define how to best adapt care to improve outcomes and lower costs.
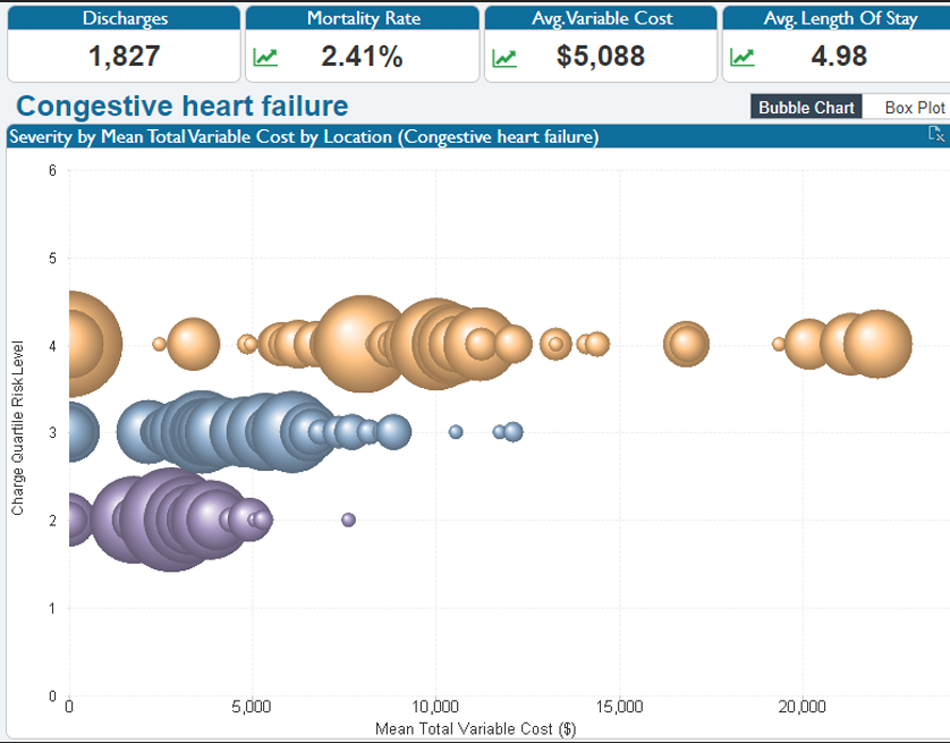
For example, financial analysts can use data to show clinicians the variation in how they are delivering care at different locations using tools like the bubble chart in Figure 1.
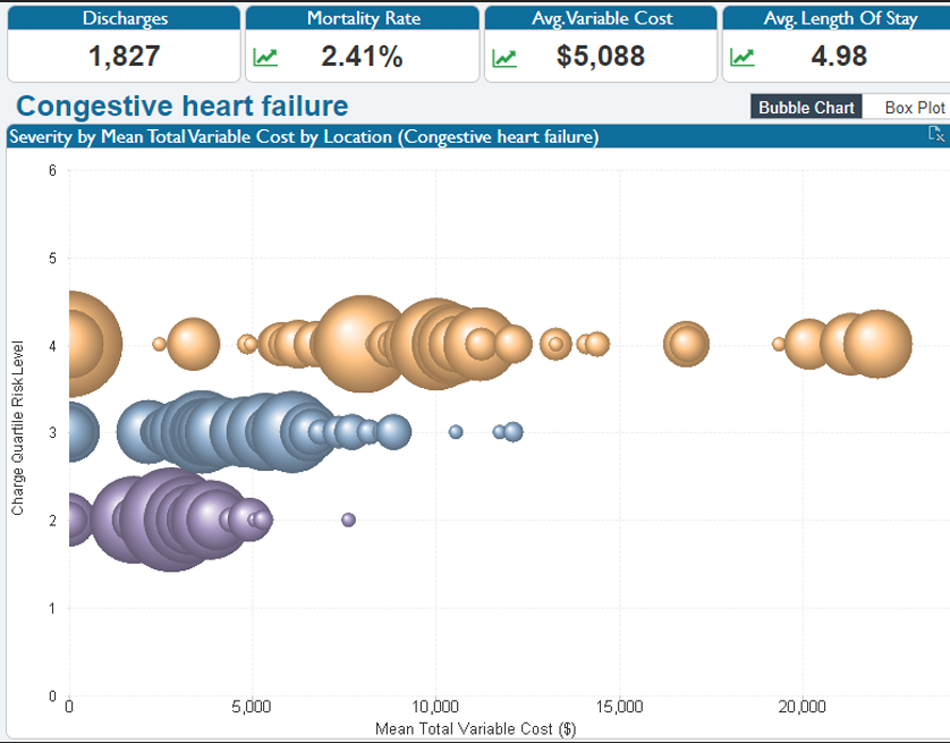
Each bubble in Figure 1 represents a location, and the size of the bubble reflects the number of cases that provider handles across a specific patient population. Variation in cost per case is displayed for the severity level of the cases treated. Noting the variation in cost per case, the data indicates an opportunity to study the clinical performance and apply lessons learned to improve quality and costs.
Presenting visually accessible data to clinicians can prompt productive discussions about which treatment protocols offer the best outcomes for patients and whether the care delivered was truly indicated. Together, clinical personnel can then determine what care they can standardize, and which costs they can reduce. Finance can model the change and share the expected results with the larger team.
In addition to effective data sharing, frontline teams must be longstanding and not dissolve once they achieve their goals. The organization needs to continuously incorporate teams into its structure to watch measures on an ongoing basis. Teams must have the power and accountability to make changes as needed to constantly improve care. Without consistent, ongoing surveillance of quality and cost measures, gains may begin to fall away.
With the industry moving towards VBP, financial executives must embrace a paradigm shift away from volume and embrace quality care as a key resource to ensure organizations’ financial health. The combination of effective collaboration between financial and clinical personnel and an agile data platform creates a clear pathway for financial success under the new value-based paradigm.
Would you like to learn more about this topic? Here are some articles we suggest: