Since accountable care took the healthcare industry by a storm in 2010, health systems have had to move from their predictable revenue streams based on volume to a model that includes quality measures.
While the switch will ultimately improve both quality and cost outcomes, health systems now need the capability of tracking and analyzing the data from both clinical and financial systems.
A late-binding enterprise data warehouse provides the flexible architecture that makes it possible to liberate both kinds of data to link it together to provide a full picture of trends and opportunities.
I have a book on my desk that tends to scare people, but its thesis is a great way to introduce the importance of linking clinical and financial data to improve healthcare. The book is called Show Me the Money by Jack and Patricia Phillips.
The book isn’t there to scare people, of course. It’s there because I’m a finance person, and I love the book’s discussion about achieving high-value results because it’s applicable to today’s new healthcare environment.
Health systems didn’t need to concern themselves with achieving high-value care until accountable care took the healthcare industry by a storm in 2010. That’s because health systems had a predictable revenue stream from the fee-for-service payment model, and to account for their revenue, they were primarily interested in the financial data they acquired from patient volumes.
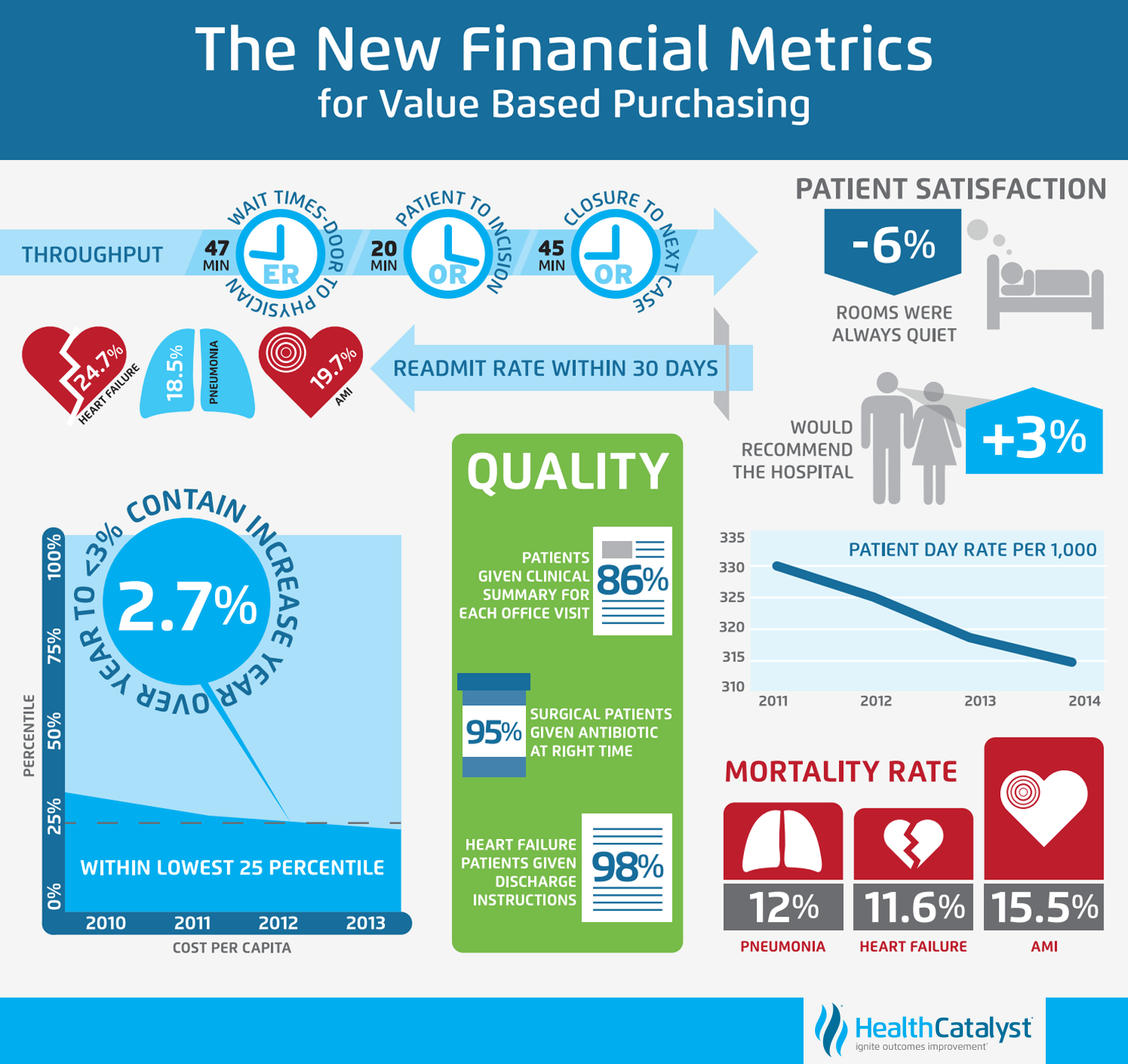
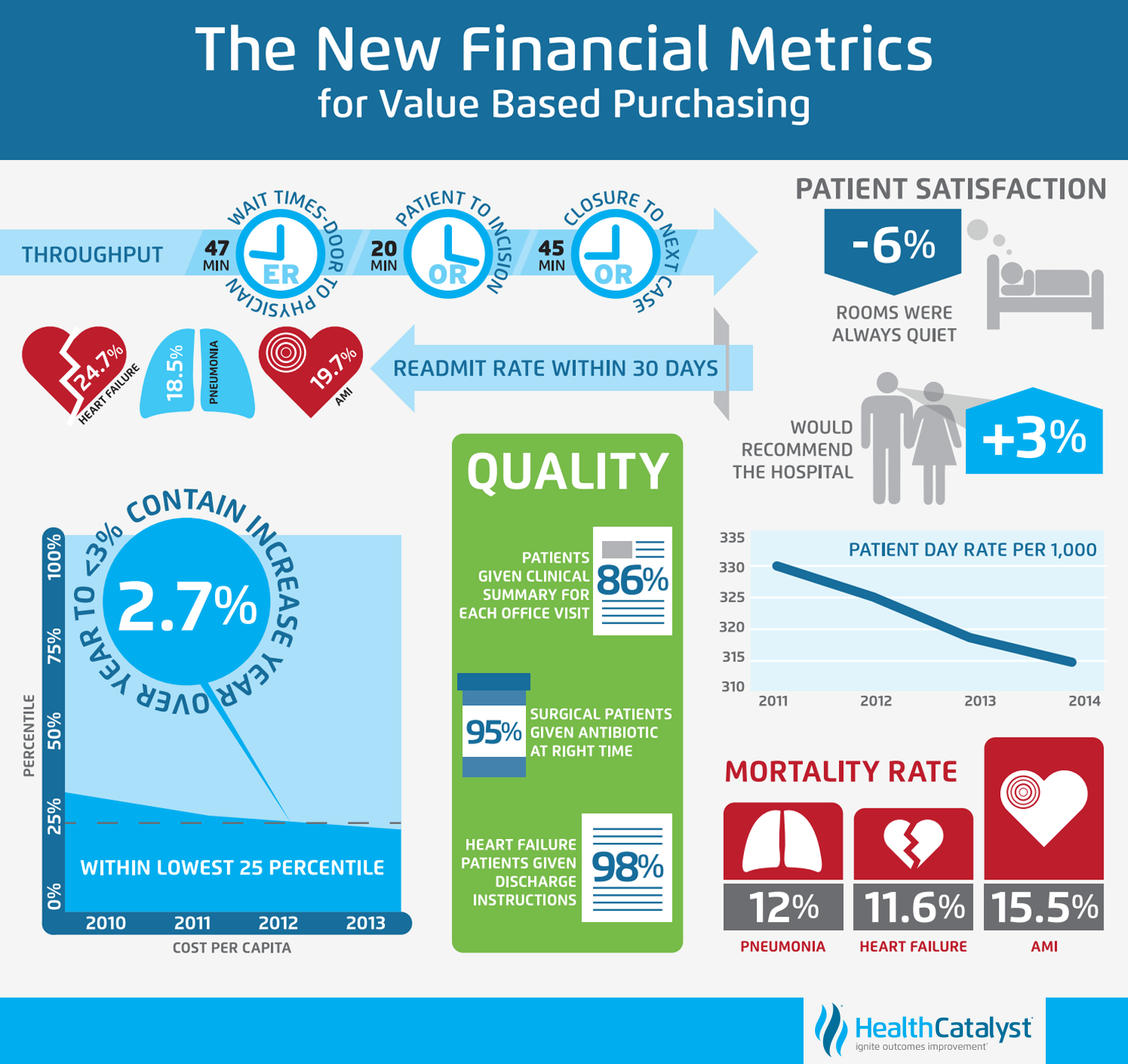
The days of only tracking volume with the fee-for-service model, however, are now long gone. Nowadays health systems are tasked with providing high-value or value-based care along with a new focus on improving the quality of care based on clinical data.

While the switch to value-based purchasing will ultimately improve both quality and cost outcomes, health systems now need the capability of tracking and analyzing many other metrics before they can comply with the government’s new mandates. These metrics include the following:
As though health systems weren’t already dealing with enough concerns with all of the new metrics they need to capture and analyze, there’s one more challenge they’re dealing with — accessing linked clinical and financial data from within their systems to provide the right metrics in this new world of value-based reimbursement.
Traditionally, health systems housed their financial and clinical data in separate systems. The original systems were designed this way because financial data needed to be available to certain teams tasked with specific functions such as cost and payments. Clinical data was housed in systems that would allow clinical teams to focus specifically on readmissions, hospital acquired conditions, and core measures for clinical processes. But the two data systems were not integrated because there wasn’t a need.
There is now, however, a need to access the data from both clinical and financial systems because the data can be leveraged to drive concrete, timely quality improvements. The kind of quality improvements necessary to survive in this new world of accountable care, quality measures, shared savings, and bundled payments while also lowering costs.
Achieving high value results for health systems is a winnable challenge, provided the organization approaches the task with a thorough understanding of where it stands relative to clinical quality measures and the financial costs associated with delivering care. But the right tools and teams are necessary to liberate clinical and financial data to link it together to provide a full picture of trends and opportunities.
Enterprise data warehouse and Data Operating System
An enterprise data warehouse (EDW) provides the ability to aggregate data from a wide variety of sources, such as clinical, financial, supply-chain, and HR source systems, in such a way that a sophisticated analytics system can then leverage the data to drive concrete, timely quality improvements.
However, traditional data warehousing, which solved some of these problems, is no longer good enough. As Gartner recently reported, traditional data warehousing will be outdated and replaced by new architectures by the end of 2018. And current applications are no longer sufficient to manage these burgeoning healthcare issues. The technology is now available to change the digital trajectory of healthcare.
The Health Catalyst® Data Operating System (DOS™) is a breakthrough engineering approach that combines the features of data warehousing, clinical data repositories, and health information exchanges in a single, common-sense technology platform.
Multi-disciplinary teams
In addition to the EDW and DOS, permanent multi-disciplinary teams of frontline staff (for example, clinicians, quality personnel, analysts, a financial representative, and technologists) can help drive sustainable improvement initiatives by analyzing the data to determine what to target and how best to realize improvement.
The team then sets goals that they constantly monitor to ensure they’re focused on sustaining quality and financial improvements as well as clinical and operational outcomes. Once they discover an improvement based on the data and best practices, then they work to gain buy-in from the clinicians to adopt the improvement.
The “Aha!” Moment
It’s important to educate clinicians so they buy in to the improvement and understand the financial implications. In working with health systems for many years, I’ve discovered that if education and financial results are tied to real, demonstrable clinical improvements, clinical teams will become excited about the change. By using easy-to-use dashboards along with DOS, clinicians can visualize their own progress. The “Aha!” moment comes when they can see how the clinical decision they made two days ago affected the bottom line today.
A Health System Example of Linking Clinical and Financial Data to Improve Costs
Here’s a quick example of how a client I worked with benefitted by gaining buy-in from their frontline teams. One of our client hospitals targeted length of stay following an appendectomy as a key opportunity for quality and financial improvement. The frontline team looked at the data in their EDW and discovered that clinicians were prescribing a wide range of antibiotics after an appendectomy.
Based on the outcomes data for each antibiotic, the team decided on a protocol for the entire facility and started encouraging clinicians to prescribe one particular antibiotic following surgery. The antibiotic turned out to be expensive, so any clinician who knew that the hospital was trying to cut costs might simply suggest using a lower-cost medication. But because we had linked the clinical and financial data in the data warehouse and made it available via dashboards, clinicians could see that while pharmacy costs rose, a parallel drop in length of stay (LOS) more than made up the difference. Once clinicians saw these results and caught the vision, they began requesting further refinements to the system. They began asking the team questions like, “Are we giving patients the antibiotic at the correct time after surgery?” Clearly, these clinicians became willing and proactive participants in the process. This is what data-driven quality improvement is all about.
In short, quality and cost improvements require intelligent use of linked financial and clinical data coupled with education for multi-disciplinary teams who are driving process improvements. DOS offers the ideal type of analytics platform for healthcare because of its flexibility. DOS is a vendor-agnostic digital backbone for healthcare. Using DOS, teams will be able to populate workflow information systems with critical point-of-decision insights and give the organization access to the most recent clinical and financial data. This, in turn, provides the organization with the best way to identify quality and cost improvements and ultimately to achieve high-value results.
Would you like to use or share these concepts? Download this presentation highlighting the key main points.