The Centers for Medicare & Medicaid (CMS) intend to sunset the traditional Merit-based Incentive Payment System (MIPS) under the Quality Payment Program (QPP), so providers and healthcare groups must know how to confidently navigate its replacement -- the MIPS Value Pathways (MVP) -- using a comprehensive approach to data collection and reporting.
 Download
Download

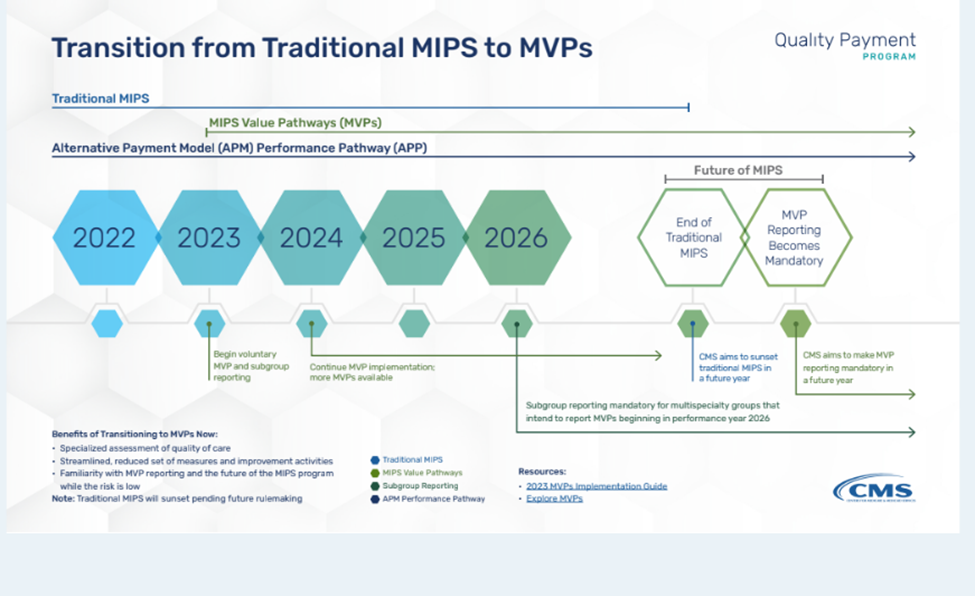
The Merit-based Incentive Payment System (MIPS) is undergoing a significant transformation with the introduction of MIPS Value Pathways (MVPs). Finalized in the November 2, 2023 Physician Fee Schedule (PFS) Final rule for Performance Year 2024, MVPs are poised to become the primary reporting structure for MIPS participants in the future. Until then, healthcare organizations can benefit from the early adoption of MVPs, gaining familiarity before they become mandatory.
The introduction of MVPs is part of an ongoing effort by the Centers for Medicare & Medicaid Services (CMS) to enhance MIPS. MVPs are designed to make reporting and participation in MIPS more relevant and meaningful for specific specialties or medical conditions while also keeping patients at the center of informed decision-making in clinical settings. Just like traditional MIPS, healthcare teams can use MVPs to gain analytic insights, identify care gaps for each measure, and work to address these gaps to improve quality.
It is beneficial for providers to submit measure data using both MVPs and traditional MIPS, as CMS will apply the higher score achieved. Meanwhile, providers can improve their efficiency in navigating MVP reporting, maintenance, and measure requirements by gaining a clear understanding of the pathways, especially considering the policy changes that will take effect in 2024.
CMS has actively revamped MIPS reporting options through initiatives outlined in the CY 2023 Physician Fee Schedule (PFS) Final Rule and subsequent CY 2024 updates to the Medicare Shared Savings Program (MSSP). These improvements culminated in the development of MIPS Value Pathways (MVPs), a streamlined reporting framework designed to ease participation and promote value-based care.
Clinicians in 2023 had three MIPS reporting options: MVPs, traditional MIPS, and APM Performance Pathway (APP). However, CMS plans to phase out traditional MIPS in the future, making MVP reporting mandatory unless clinicians opt for APP.
To report an MVP, advance registration is required, and each MVP consists of a subset of measures and activities tailored to specific medical specialties or conditions.
Quality: CMS will select the top 4 performing quality measures (similar to MIPS).
Improvement activities: CMS will award 20/40 points for medium/high-weighted activities (differs from MIPS).
Cost & Promoting Interoperability: CMS will collect Cost data using Medicare Part B claims while the Promoting Interoperability requirements are identical to traditional MIPS.
Final score: Aligns with traditional MIPS performance category weights.
Focus: Priority is given to health equity and performance-enhancing activities.
The MVPs were expanded from the 12 available in the 2023 performance year to 16 available in the 2024 performance period.
Two MVPs from 2023 (“Optimizing Chronic Disease Management” and “Promoting Wellness”) were combined to create the newly adopted “Value in Primary Care” MVP in addition to four other new MVPs covering new medical conditions and specialties.
The five new MVPs for PY 2024 are as follows:
Below is the list of all finalized MVPs for the 2024 performance year:
G0057 Adopting Best Practices and Promoting Patient Safety within Emergency Medicine
M0001 Advancing Cancer Care
G0055 Advancing Care for Heart Disease
G0053 Advancing Rheumatology Patient Care
G0054 Coordinating Stroke Care to Promote Prevention and Cultivate Positive Outcomes
G0058 Improving Care for Lower Extremity Joint Repair
M0002 Optimal Care for Kidney Health
M0003 Optimal Care for Patients with Episodic Neurological Conditions
G0059 Patient Safety and Support of Positive Experiences with Anesthesia
M0004 Supportive Care for Neurodegenerative Conditions
M1366 Focusing on Women’s Health
M1367 Quality Care for the Treatment of Ear, Nose, and Throat Disorders
M1368 Prevention and Treatment of Infectious Disorders Including Hepatitis C and HIV
M1369 Quality Care in Mental Health and Substance Use Disorders
M1370 Rehabilitative Support for Musculoskeletal Care
M0005 Value in Primary Care
As mentioned earlier, CMS is expected to sunset traditional MIPS in future legislation, at which point MVPs will become mandatory unless the clinician qualifies to report the APP. In the meantime, CMS has publicized important milestone dates to facilitate a smoother transition to MVPs, including the following:
Such regulatory changes may introduce data quality and management challenges for ACOs, clinicians, and practices as they migrate to reporting MVPs, making it crucial to stay updated on the most recent policy changes and emerging best practices.
Fortunately, the Health Catalyst ambulatory measures solution offers a comprehensive approach by integrating an organization's data from various sources, compiling measures from multiple programs, and providing detailed performance visualizations. This streamlines the process of monitoring, improving, and submitting performance to CMS, creating a more efficient workflow for users and enabling providers to more easily identify and address gaps in care.
Would you like to learn more about this topic? Here are three articles we suggest:
A Complete Guide to MIPS Quality Measures
Data-Informed MIPS Improvement Efforts Drive Improved Quality Scores and Increased Revenue