Despite pandemic-driven limitations, health systems can still find ways to optimize revenue cycle and generate income. When health systems improve and prioritize patient access through a patient-centered access center, they can improve the revenue cycle performance through decreased referral leakage, better patient trust, and optimum communication across hospital departments.
Rather than relying on traditional revenue cycle improvement tactics, health systems should consider three ways a patient-centered access center can positively impact revenue cycle performance:
1. Advance access.
2. Optimize resources.
3. Engage stakeholders.
 Download
Download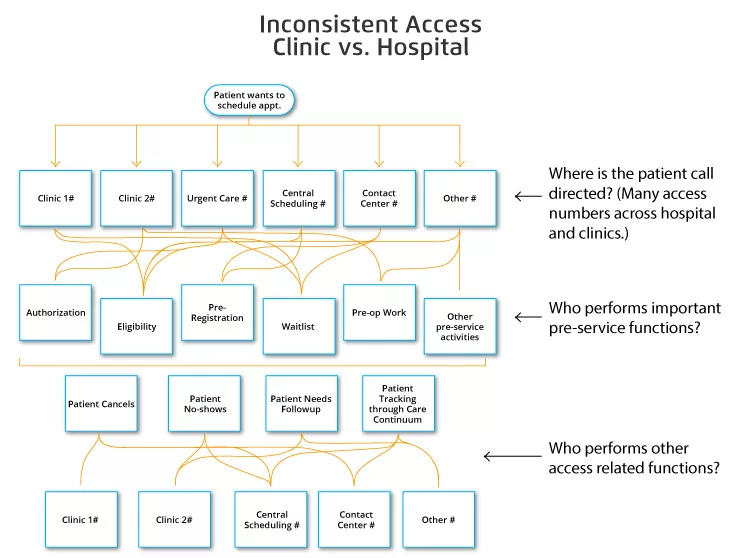
This report is based on a 2020 Healthcare Analytics Summit (HAS 20 Virtual) presentation by Jennifer Livermore, MSIHM, Director of Access Operations, ProHealth Care, titled, “Improving Revenue Cycle Performance with a Patient-Centered Access Center.”
In a fraught healthcare landscape, health system leaders learn to operate on thin margins with limited resources. However, some leaders overlook the value that better patient access can have for an organization’s financial well-being, especially when unprecedented changes, such as COVID-19, compromise access in new ways.
Patient access is the foundation for optimal revenue cycle performance because providing care is the primary income source for health systems. Therefore, if patients can’t easily access care, hospitals can’t deliver that care, nor generate income because patients will seek care elsewhere. Establishing a patient-centered access center, one place (or source of truth) for all patient inquiries, requests, and referrals, can help health systems optimize patient access and, thus, improve the healthcare revenue cycle.
Too often, health systems only focus on healthcare revenue cycle management (e.g., processing the insurance coverage verification correctly to conduct a procedure and then collect the revenue) and fail to realize the revenue cycle opportunities that come with improving patient access. To improve the revenue cycle through patient access, health systems must first understand the relationship between revenue and access.
If patients can’t access care at a health system, the organization cannot generate income from their care or procedure. No part of the revenue cycle—including billing and insurance, payment, and financial clearance to determine which patients are likely to pay (also a safeguard to prevent bad debt)—can occur unless a health system cares for patients.
Effective patient access also helps health systems respond more rapidly to COVID-19. For example, with virtual access in place, health systems can seamlessly convert in-person visits to video and telephonic visits, reserving limited hospital beds for patients with COVID-19 without forgoing patient visits.
Health systems have always faced barriers to patient access but connecting patients with care is even more challenging in a global pandemic. To improve patient access and positively impact the revenue cycle, health systems should consider the benefits of a patient-centered access center—a navigation infrastructure that creates new access points, deepens patient trust, and supports patients throughout the care journey.
Three core methods behind a patient-centered access center enhance patient access and improve the healthcare revenue cycle:
Advancing patient access is complex, but there are many ways organizations can achieve better access. Centralizing ownership of referrals and orders through a patient-centered access center and training access center staff to provide patients with a consistent experience, no matter where they receive care throughout the system (e.g., cardiovascular, pulmonary, orthopedics) have a positive impact on access. A decentralized approach often fails to hold team members accountable for sending referrals and orders to the right place.
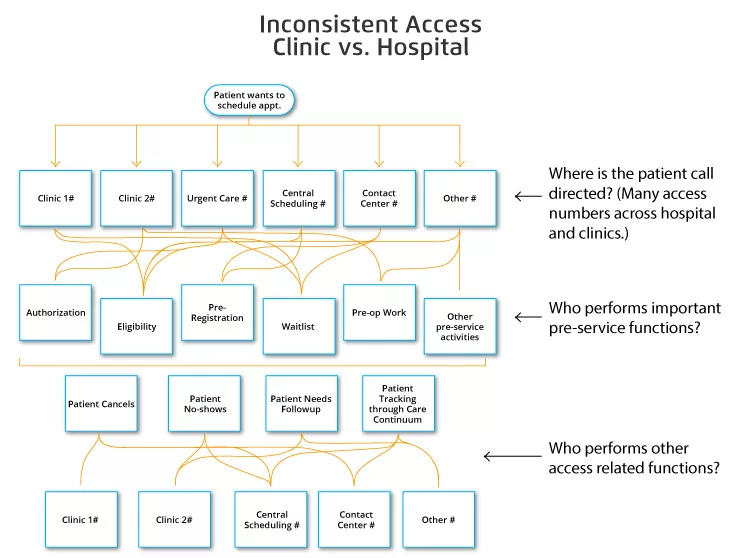
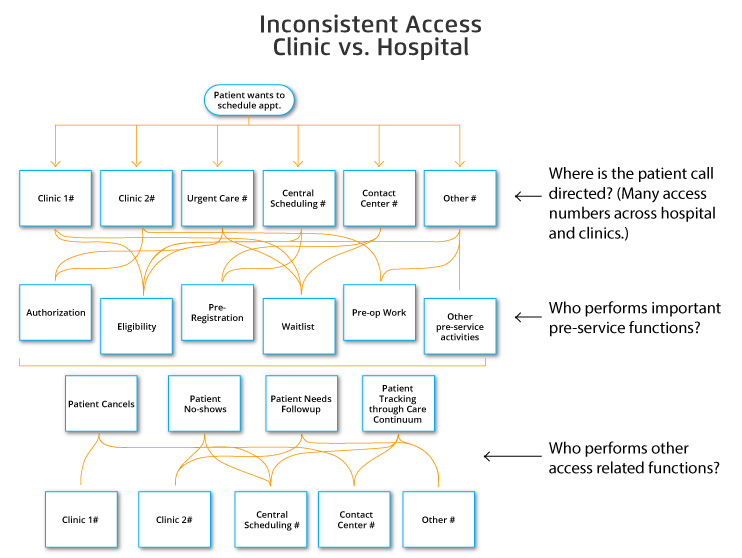
Historically, health systems have taken a decentralized patient access approach (Figure 1). This scattered approach makes it difficult for team members to follow referrals, ensure the referral makes it to the correct destination, and identify the process gap that sends a referral to the wrong place. Inconsistent responsiveness (e.g., in a decentralized call center) leads to patient confusion and dissatisfaction, increasing the likelihood that a patient will seek care elsewhere.
Centralizing referrals in one place (e.g., a patient-centered access center) ensures responsiveness to service requests and matches patients to the optimal service, provider, and location, leading to better access and satisfaction. These small changes result in higher efficiency (because team members refer patients to the right place the first time), more procedures, and, therefore, more revenue.
Common patient access resource challenges include differing schedule management practices by department and a lack of clarity around patient cancellations and no-shows. To tackle scheduling management differences, health systems can better optimize resources by creating and distributing standard templates and protocol guidelines.
When every team member at the patient access center follows the same (or similar) workflow, different access center teams don’t have to waste energy recreating workflows, allowing health systems to optimize the limited resources they have. Another way to optimize limited, and sometimes overworked, staff is to define schedule management best-practices and unify them across departments by training template owners on applying scheduling standards.
Health systems can also optimize resources by cross-training staff so that all team members at the access center can handle every type of patient access request, rather than transferring patients to other teams. For example, to overcome cancellations and no-shows, leaders can train all access center team members about the correct workflow to fill empty patient slots, giving patients every opportunity to schedule and keep an appointment. When a patient-centered access center provides every opportunity for a patient to receive care, the health system has the chance to generate revenue from those appointments instead of losing revenue from canceled or missed appointments.
Effecting change in any organization is challenging, especially in a health system—where disparate departments spearhead initiatives, and leadership support is already spread thin. However, stakeholder engagement (or leadership support) is critical in improving patient access.
Health systems can increase stakeholder engagement around a patient-centered access center by creating collaborative governance structures that drive design, goals, and performance evaluation and issue resolution tactics. With a clinical and administrative leadership perspective, health systems can also help evaluate referral and demand processes and patterns and ways to improve them.
Regularly engaging leadership in the details of a patient-centered access center and how to improve it will increase buy-in and dedicated resources around the access center and other access-focused initiatives. In addition, when leaders and providers are committed to advancing access, they will find ways to improve access within their respective disciplines.
In a challenging time with limitations from COVID-19, organizations can still generate income and improve revenue cycle performance through a patient-centered access center. Advancing access through responsiveness and consistency, optimizing resources to reflect availability accurately, and engaging stakeholders in problem-solving access issues leads to an effective patient-centered access center where a health system can review, understand, and track all patient access entry points. When health systems prioritize patient access, they can improve the healthcare revenue cycle through decreased referral leakage, improved communication across different departments, and getting patients to the right place the first time.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.
Click Here to Download the Slides
https://www.slideshare.net/slideshow/embed_code/key/DseKQqemNfd6BJ