Heart failure treatment is complex and requires ongoing attention. To ensure organizations are delivering optimal treatment to prevent disease, slow progression, and improve outcomes there are seven key strategies across the continuum of care to deliver guideline-directed medical therapy and engage patients in their care.
 Download
Download
Heart failure (HF) impacts 6.2 million adults in the United States and has negative physical and emotional consequences, resulting in poorer quality of life and increased morbidity and mortality. Treating HF is complicated and dependent upon severity of disease and comorbid conditions. It requires different treatment protocols, ongoing titration, optimization of therapy, perpetual assessments, remote patient monitoring, and lifestyle changes. Without all these interventions, mortality and morbidity increase, hospital stays are lengthened, and unnecessary hospital readmissions occur.
The recently published 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure provides treatment recommendations for each of the four stages of HF — from patients who are at risk for HF to those who already have advanced disease. To deliver effective care, healthcare organizations need a comprehensive approach. Through optimal care, organizations can prevent HF, slow disease progression, improve the quality of life for patients, and prevent hospitalization and readmissions.
Here are seven strategies to improve HF care and impact outcomes and the patient experience.
HF disease progression can be slowed and patient outcomes can be improved when guideline-directed medical therapy (GDMT) is closely followed, yet the data shows this often doesn't happen. That may be due to a variety of reasons:
Leveraging technology and more rigorous processes across the continuum can bridge these gaps in HF care delivery and ensure compliance with GDMT.
Data analysis is an essential population health initiative to identify patients who may be at risk for developing HF, including those with high blood pressure, high low-density lipoprotein (LDL) cholesterol, diabetes, smoking and secondhand smoke exposure, obesity, unhealthy diet, and physical inactivity. Armed with these data, organizations can develop programs designed to modify lifestyle behaviors that may include primary care initiatives, community and school programs, individual wellness coaching, and direct consumer engagement.
For those with an existing diagnosis of HF, cohort stratification into stages (Class I through IV) based on left ventricular ejection fraction (LVEF) enables analysis of compliance with GDMT, including pharmacological and non-pharmacological therapies. An enterprise view of deviation from guideline-based patient management enables the identification of patterns that may form the basis for action, such as training, distribution of monthly performance dashboards, creation of remote physiologic monitoring programs, evolution of nurse navigator protocols, and more.
A HF hospital admission, as noted in the AHA/ACC/HFSA report, represents a critical opportunity to continue, initiate, and further optimize GDMT. However, the CHAMP-HF (Change the Management of Patients with Heart Failure) registry identified many eligible patients with a reduced LVEF who were not prescribed guideline-informed therapies.
Standardization of inpatient care protocols across an organization, IDN, or network represents a crucial improvement activity and includes:
Alerts and notifications can serve as reminders to frontline staff when there is a deviation from GDMT. They can ensure that the appropriate tests are being ordered and medications are being paused, delivered, or titrated.
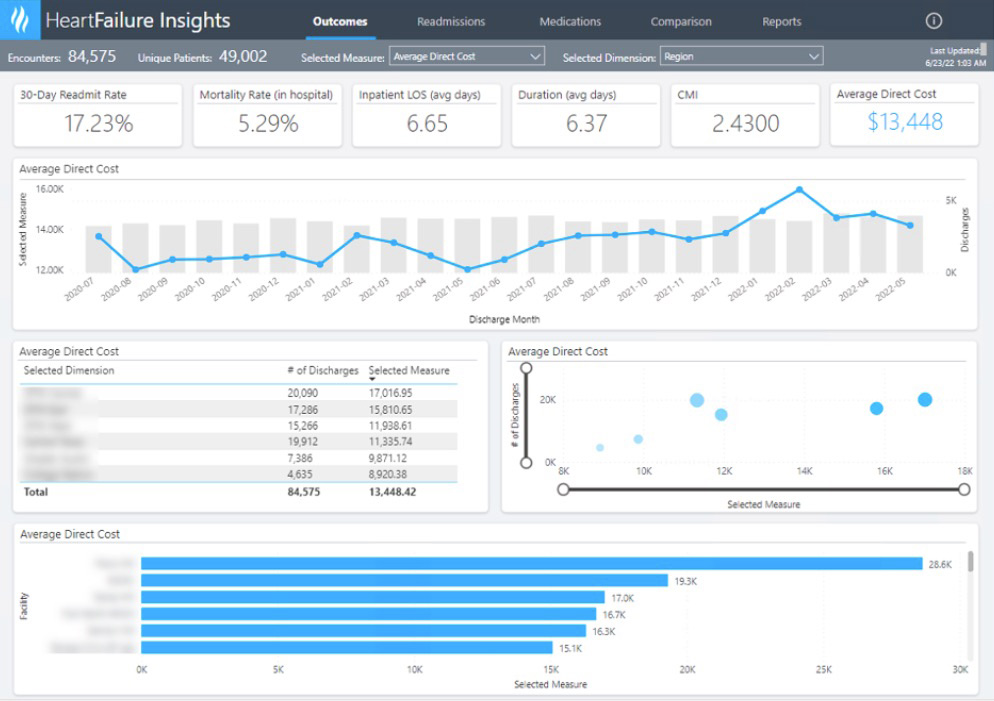
Enterprise-wide dashboards driven by robust data and analytics can support clinical leaders in identifying unwarranted care variation by location, provider, and patient cohort. Filters and drill-down capabilities are useful in analyzing the root cause of variation, therefore pinpointing improvements that will likely have the largest impact on clinical outcomes, operational efficiencies, and revenue.
HF patients are most at risk during transitions from one care setting to another. The hospital-to-home transition is particularly problematic, with very high rehospitalization and mortality rates occurring after HF discharge. Implementing structured telephone support after discharge, multidisciplinary HF clinics in the community, and care transition interventions such as home visit programs involving pharmacists and nurses can reduce readmissions and mortality.
Transitional care plans initiated prior to discharge define patient-centered instructions with a clear plan for transitional care. It’s also an opportunity to address high-risk characteristics associated with poor post-discharge clinical outcomes and plan for medications, follow-up, and at-home monitoring. Leveraging a technology solution can help automate these tasks through checklists and care team alerts.
Medication adherence and care plan compliance are also common post-discharge concerns. Many organizations are realizing success with automated digital patient communication and engagement pathways that aim to overcome challenges:
Real-time, automated care team notifications based on patient engagement parameters also support intervention to prevent further exacerbation that leads to ED visits and hospital admissions.
It’s important to monitor patient health and titrate GDMT medication dose every 1–2 weeks to achieve treatment goals and prevent readmission. However, the continual compression of inpatient length of stay complicates medication monitoring. To initiate and optimize treatment after hospitalization, an ambulatory clinical communication pathway can assist with ensuring the completion of medication reconciliation, follow-up phone calls from the care team, scheduled clinic appointments, and identification of barriers at home.
Initiating care management and navigation services can serve as added support for patients who face significant barriers or are living with severe illness. Care teams can better ensure patients receive timely care and avoid rehospitalization or death.
Remote cardiac monitoring encourages patients to be proactive in their care. Noting changes in daily readings supports smarter decision-making about their activity levels, diet, and lifestyle choices. RPM is also a simple and effective way for healthcare providers to keep track of disease progression and provide early intervention.
There are a variety of ways to deploy RPM. For patients identified in the at-risk group, a simple blood pressure monitoring pathway can be automatically deployed via patient engagement technology. It can support the patient in obtaining a blood pressure monitor, remind them to submit their BP readings on a regular basis, and deliver information like dietary tips and encouragement to make lifestyle changes.
It's also very important for HF patients to monitor their weight, blood pressure, and symptoms. Automated text messages can prompt patients to report barriers such as lack of access to a weight scale or difficulty obtaining prescribed medications.
This real-time feedback enables optimization of treatments, early intervention when needed, slowed disease progression, and improved outcomes.
HF patients with low activation can experience negative outcomes, including higher 30-day mortality, and patients at the lowest activation level had a more than sixfold increased risk of death within 30 days of hospital discharge compared with patients in the highest two activation levels. Furthermore, most patients hospitalized with HF have low activation, and therefore lack the skills, confidence, and motivation to manage their own health. They also tend to be less satisfied with their care and more often require skilled care at hospital discharge.
Maintaining a connection outside of a clinical or hospital setting is essential for patients who are at risk for HF – whether it’s to monitor physiologic data, provide education and encouragement, or connect patients with resources. For patients who are at risk for HF or are already living with this progressive disease, organizations must find creative ways to engage patients between visits to ensure compliance with GDMT, conduct serial assessments, monitor patient-reported outcome measures, and dynamically adjust medications and therapies based on evolving patient conditions.
Empowering patients can also ease the ongoing healthcare staffing challenges. Nurse navigator activities can be supplemented with patient engagement strategies. The automated delivery of simple text messages makes patients feel more cared for, and based on patient responses, care teams can be alerted about potential deterioration and provide early intervention.
A comprehensive approach to HF is essential to meaningfully prevent the disease, slow progression, improve the quality of life for patients, and prevent hospitalization and readmissions. Compliance with national guidelines for management of patients with HF is challenging for many providers given their complex and evolving nature. The opportunity to optimize care delivery spans the continuum:
Technology is a powerful ally in the quest to improve HF outcomes. Providers face mounting pressure to deliver GDMT amidst a staffing crisis, while also lacking actionable data to drive decision-making. Effective strategies to optimize patient outcomes, decrease mortality and morbidity, reduce hospital length of stay, and prevent unnecessary hospital readmissions include:
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download this presentation highlighting the key main points.