The COVID-19 era has seen a decline in visits to ambulatory care practices by 60 percent and an estimated financial loss for primary care of over $15 billion. Shutting down elective care is financially unsustainable for health systems and for patients, who continue to need non-pandemic-related care. While virtual medicine has emerged as a viable and mutually beneficial solution for patients and providers, the shift from in-person to virtual health is logistically and financially complicated.
Processes and workflows from in-person care don’t directly translate to the virtual setting, and a financially successful shift requires deep understanding of the factors driving patient engagement and revenue in the new normal. As such, meeting patient needs and financial goals requires robust enterprisewide analytics that drill down to the provider level.
 Download
Download

This article is based on a Healthcare Analytics Summit(HAS 20 Virtual) presentation by Patrick McGill, MD, Executive Vice President, Chief Analytics Officer, Community Health Network, titled, “Virtual Care in the COVID-19 Era: Enabled with Enterprisewide Analytics.”
Early in the spring of 2020, the CMS responded to COVID-19-related healthcare capacity strain with a call to delay all non-essential, elective procedures, heavily impacting ambulatory, including primary, care. As of April 2020, the number of visits to ambulatory care practices had declined by 60 percent nationwide. In June, Health Affairs estimated a loss for primary care of up to $15.1 billion nationally, with primary care practices losing an estimated $67,774 in gross revenue per full-time physician.
Medical practices and health systems have scrambled to avoid burning through cash while also attempting to save lives. Some organizations made cost-cutting measures, such as furloughing employees. However, these solutions were inadequate because patients still needed care, and organizations still have revenue gaps to fill.
A more sustainable, pragmatic response to the downturn in ambulatory care has been shifting to virtual care. Whether organizations were ready for the transition from in-person to remote visits, the pandemic forced them to rapidly embrace virtual models and likely maintain them for the foreseeable future. Health systems that have made smooth transitions already had robust enterprisewide analytics practices in place, which they leveraged to inform changes to best meet patient needs and financial goals.
Even though ambulatory care rebounded somewhat by May 2020, outpatient visits were still one-third lower than pre-pandemic rates. Furthermore, while outdated rules and regulations previously hindered virtual care adoption, the CMS announced in spring 2020 that it would pay for virtual visits in parity with in-person care. These events reaffirmed virtual medicine as a new key player in healthcare delivery and the ongoing need for analytics to inform and optimize virtual models.
Analytics that proved essential for organizations to transition to virtual care successfully included dashboards for COVID-19 metrics. With critical insights—such as positivity rates, ICU volumes, and more—dashboards helped team members understand the virus’s state within their health systems, respond to pandemic-driven needs, and anticipate capacity requirements (e.g., personal protective equipment, ventilators, etc.).
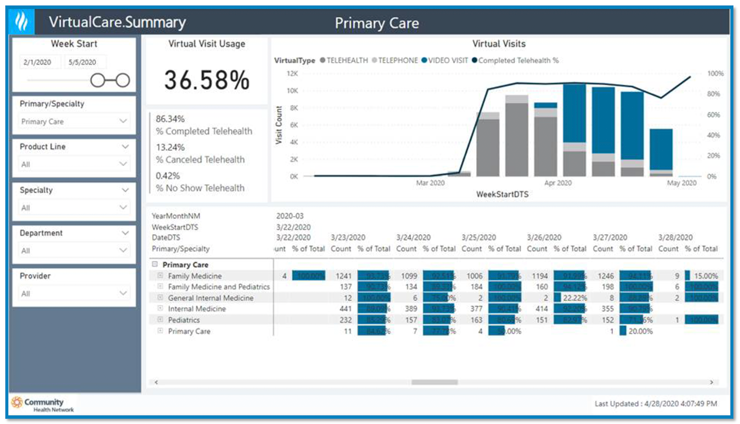
Insight into provider and patient needs will continue to be critical as organizations plan for the technology and policies to deliver virtual care cost effectively throughout the crisis. Forward-looking tasks include launching a video/telephonic platform systemwide and incorporating virtual care as part of a financially successful practice (Figure 1).

Analytic tools in the ambulatory setting that have enabled a smooth transition to virtual care measure performance down to the provider level and identify what makes each provider successful independently. This provider-level view, or analytics for practice management (Figure 2), requires a suite of tools to look at income statements, productivity, patient access, no shows, cost and overhead, and revenue cycle. Organizations with these analytics in place before a pandemic could make the most seamless shifts to virtual care, as they had positioned themselves to understand the impact of the transition per individual provider.

Reimbursement was a pre-pandemic barrier to widespread adoption of virtual care. But with reimbursement parity for a virtual visit, for the time being, healthcare can expect to see the virtual models become a delivery fixture. Consumer demand will also drive virtual care adoption, as patients increasingly want to interact with the healthcare system the same way they interact with other services (e.g., contactless grocery shopping). Meeting these expectations for healthcare involves offering e-visits and consults, asynchronous and on-demand 24/7 visits, as well as bot-scheduled video visits and follow-ups.
The following analytics-driven actions will help organizations move their and their patients’ comfort zone from in-person care and make data-informed decisions about shifting to virtual care:
Meeting patient expectations and organizational financial goals for virtual health requires health systems to change specific processes. Team members will need new training protocols from patient engagement to leveraging different EMR workflows to measure and deliver care efficiently.
With the in-person care model, competition is generally a geographically close practice or provider. In a virtual model, however, competition can be anyone across the country. Also, new technology, such as artificial-intelligence-enabled care, will become a factor as patients seek the most immediately available care. Health systems must identify competitors and proactively engage patients (e.g., with virtual outreach), who may be a risk of seeking care elsewhere.
Analytics that measure and show the impact of virtual care (Figure 3) will be critical to understanding virtual delivery performance, such as identifying barriers to patient engagement and technology needs. The ability to filter analytics by specialty, department, practice, and down to individual provider will offer the most actionable insights, as analytics show a shift from no virtual care to phone to video visits, then to increasing adoption with the reimbursement shift.
Scenario analysis helps the organization understand the revenue impact of changes under virtual care by evaluating outcomes by visit type. For example, users can explore questions such as: how would a certain percentage of virtual visits impact revenue?
Virtual care may disproportionately affect certain populations (e.g., vulnerable communities) who don’t have reliable internet or smartphones. By breaking down patient populations by county, race, and ethnicity, organizations can identify groups that may need added support to shift to virtual care.
Provider productivity analysis shows the impact on organizational income of different workflows. For example, if a clinician adds another visit to her schedule, what’s the effect on work relative value units, patient experience, productivity, and income? Heatmaps can inform provider productivity by showing the high-demand time of day, guiding how to add visits and fill in gaps to drive virtual adoption.
Managing an entire patient panel per care team allows team members to identify people not coming into the office and target outreach, such as virtual care, to engage these patients outside of the office setting. Such interventions are essential tools to avoid losing a patient to other organizations and networks.
To optimize revenue and patient outcomes and experience in the transition to virtual care, organizations must make significant adjustments, including adoption of new tools, behaviors, and workflows. Having enterprisewide analytics that are drillable down to the provider level will help health systems understand how to shift resources to optimize virtual delivery models across the continuum of care and understand the care experience beyond the four walls of a hospital or practice, including how patients interact with the healthcare system and what the growth of virtual models means for competition in a post-COVID-19 setting.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.
Click Here to Download the Slides
https://www.slideshare.net/healthcatalyst1/shifting-to-virtual-care-in-the-covid19-era-analytics-for-financial-success-and-an-optimized-patient-experience