Acuitas Health improved access to data for its partner clinicians by using its data platform and closed-loop analytics to integrate data from more than ten disparate systems. Clinicians receive patient-specific details before the patient visit, allowing them to identify opportunities for health maintenance, improve quality, support data-driven medical decision making, increase adoption of best practices, and improve hierarchical condition category (HCC) coding.
Acuitas Health is a population health services organization that supports multiple provider practices to deliver high-value healthcare while preserving the independent practice of medicine.
Clinicians can treat their patients better when they have more information. However, huge-scale data dumps without an approach to meaningful synthesized information make patient care more difficult and inefficient.
Physicians, nurses, and other members of the care team often lack the data they need to understand their performance and improve care outcomes, even though they frequently spend substantial time and resources on data-related administrative tasks.1,2 It is estimated that $15.4 billion is spent each year just to report healthcare quality measures.2
Pre-visit planning is a process for making the necessary information available to the clinician and shifting administrative tasks out of a patient’s appointment time. The process allows clinicians to focus on the patient while increasing efficiency and decreasing costs.3
Clinicians supported by Acuitas Health were committed to ensuring patients received the best possible care, including providing patients primary and preventive care and needed medical care in the right setting, at the right cost. Despite this commitment, clinicians struggled to identify opportunities to improve health maintenance and quality and use data to drive their medical decision making.
Critical information needed by clinicians for the most effective decision making resided in disparate systems. To have all the data they wanted and needed, clinicians would have to access each system, often documenting information on paper before the patient visit, which was frustrating, time-consuming, and costly.
Acuitas Health needed a solution for its partner clinicians that would make the best use of their time, ensuring they had access to critical data, while decreasing the administrative burden and reducing costs.
The solution for Acuitas Health and the clinicians it serves was to leverage the Health Catalyst® Data Operating System (DOS™) platform and interoperability, including closed-loop technologies, to integrate data from more than ten disparate systems. The integration provides patient-specific details and synthesized insights to clinicians at the point of care in the most efficient way, before the patient visit.
Acuitas Health used the data platform to develop a pre-visit planning “EMR alert” to give clinicians access to clinical insights. The pre-visit planning form includes information from EMRs, the practice management system, health information exchange alerts, and claims data, enabling clinicians to identify opportunities for health maintenance, as well as to improve quality and data-driven medical decision making (see Figure 1).
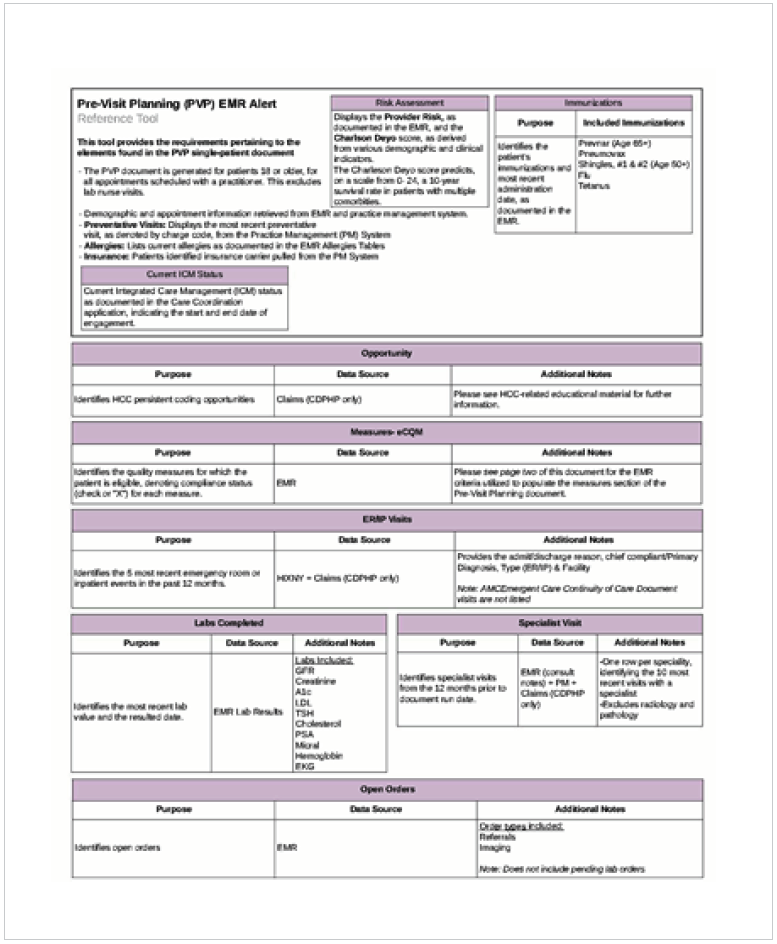
The pre-visit planning form includes high-level information about the patient, including appointments, allergies, and insurance provider. The document also includes more detailed patient information, including the following:
The pre-visit planning form also includes opportunities to improve HCC coding and electronic clinical quality measure insights. The form identifies each clinically relevant quality measure domain for which the patient is eligible, denoting the required task for each measure domain.
The data platform aggregates the necessary data, generates the patient-specific pre-visit planning form, and then uses closed-loop analytics to place a copy of the document in the patient’s EMR, updating it daily until the patient’s visit occurs. Consolidated, value-based information is now synthesized and available in a single location at the point of care with little access barriers, supporting improved pre-visit planning.
The pre-visit planning EMR alert has given clinicians access to clinical insights at the point of care for the first time, enabling users to achieve the following:
In just five months, there have been more than 24,000 patients that have received pre-visit planning, with 200 patient-level data points updated daily (new information for patients with a scheduled appointment).
“The purpose of this solution was to save time and harmonize chaos for clinicians by leveraging automation. We want to reduce burnout, free up more time for patient care, and improve patient outcomes.”
– Keegan Bailey, MS, Strategy and Technology Leader
Acuitas Health plans to continue to expand its use of the data platform and technology to support its growing practice of delivering high-quality healthcare.




