Learn how Allina Health leveraged its analytics platform and Health Catalyst professional services to perform an analysis demonstrating the impact of pharmacist-led medication therapy management (MTM).
Nearly half of all Americans use at least one prescription drug, and 11.9 percent take five or more prescription drugs, demonstrating that prescription medication use is widespread and increasingly complex.
With high prescription usage comes prevalent medication-related problems. More than 1.5 million preventable medication-related adverse events occur each year, costing more than $177 billion in medication-related morbidity and mortality.
To reduce medication-related adverse events, Allina Health, a non-profit health system, was considering expanding the involvement of pharmacists performing medication therapy management (MTM) to a group of Medicaid patients covered by a shared-risk contract. Prior to being able to make this decision and develop a comprehensive business plan, the health system wanted to better demonstrate the unique impact pharmacists were making on patient outcomes.
Among ACO NextGen Medicare cost insured patients, prescription medication use is commonplace and increasingly complex. Nearly half of all Americans use at least one prescription drug with 11.9 percent using five or more prescription drugs.1 Also prevalent are medication-related problems. There are approximately 1.3 million emergency department (ED) visits each year due to adverse drug events, with about 350,000 patients requiring hospitalization for treatment.2
A not-for-profit health system, Allina Health cares for patients from beginning to end of life through its 12 hospitals, 65 clinics, 52 rehabilitation locations, 23 hospital-based clinics, 15 retail pharmacies, and two ambulatory care centers. It continually looks for ways to minimize medication-related adverse events and improve care outcomes.
Allina Health’s advanced care team, an integrated group of healthcare disciplines including social workers, registered nurses, care guides, and pharmacists, is focused on the coordination and care of patients with complex healthcare needs. The advanced care team pharmacists focus their efforts on patients who have recently been discharged from the hospital who are at high-risk for readmission, and patients with high ED utilization.
Pharmacists meet with patients and complete a comprehensive medication review. The intent of the pharmacists’ review is to optimize drug therapy to improve the clinical outcomes in collaboration with the patient’s provider. The pharmacists provide in-depth education to patients and their families and caregivers, helping to increase patient understanding and adherence.
While Allina Health had completed a comprehensive analysis on the impact of the advanced care team, demonstrating reductions in the total cost of care, reduced hospital admissions, and reduced ED visits, it had not yet isolated the role of the pharmacist and evaluated their contribution to outcomes.
Allina Health was considering expanding the involvement of pharmacists performing MTM to a group of Medicaid patients covered by a shared-risk contract. Prior to making this decision and developing a comprehensive business plan, pharmacy leaders at Allina Health wanted to better understand the impact pharmacists were having on patient outcomes.
To better understand the impact of the pharmacist on patient outcomes, Allina Health leveraged the Health Catalyst® Analytics Platform and Health Catalyst professional services to perform a comprehensive analysis.
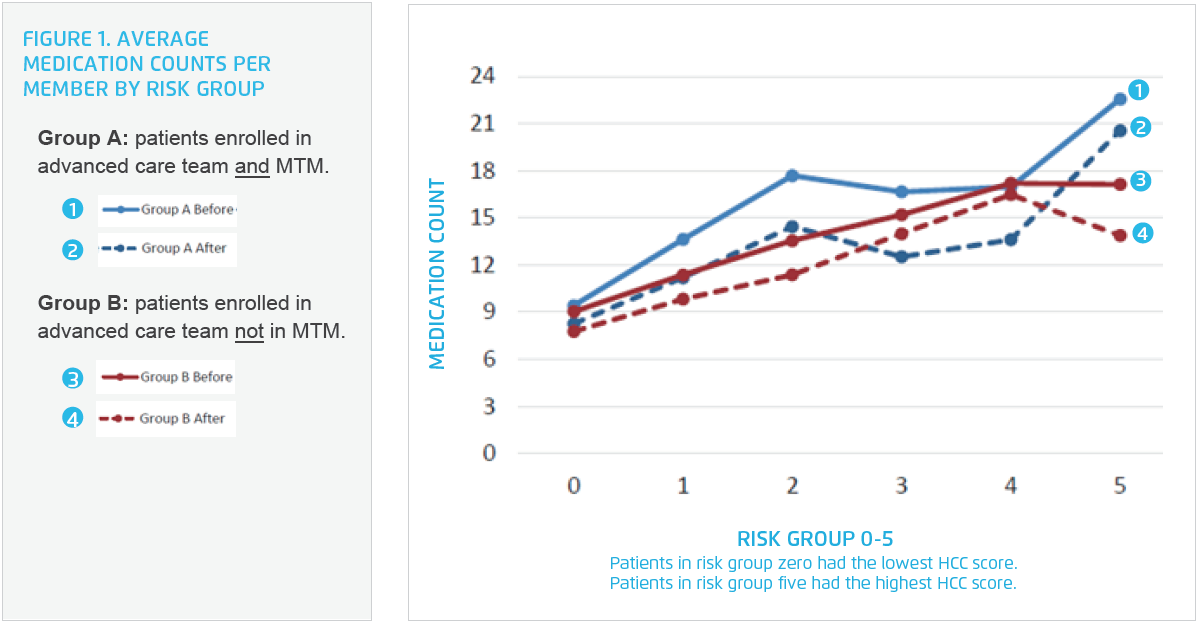
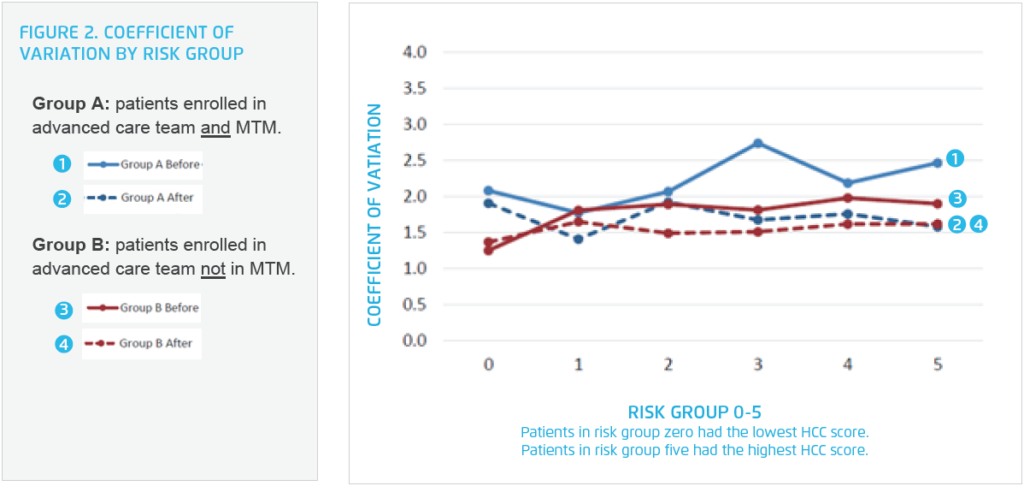
Using claims and clinical data from the analytics platform, analysts compared outcomes for two groups. Both groups consisted of patients receiving advanced care team services with Group A patients also obtaining MTM, while patients in Group B did not get MTM. Using these criteria, the analysis observed 283 patients in Group A and 566 patients in Group B.
Each group has an index date: Group A is the first MTM encounter date and Group B is the advanced care team enrollment date. This enables analysts to evaluate, by patient, the total cost of care in the six-month period prior to the index date against the total cost of care in the six-month period after that date.
Analysts used the Centers for Medicare and Medicaid (CMS) rolling 12-month hierarchical condition category (HCC) score at the time of the index date to group the patients into six risk different groups (zero-five). The risk score distribution helped demonstrate that the patient populations for Group A and Group B were comparable enough to be evaluated against each other. The risk groups included:
Analysts then evaluated the pharmacist MTM impact on all MTM and advanced care team patients. The analysis included:
The analysis, using Allina Health’s specific data and patient population, demonstrated the unique, positive impact pharmacist MTM is making on patient outcomes in the six-month period following the pharmacist MTM. This program is effectively reducing the total cost of care.
Results include:
MTM pharmacists have also decreased the pill burden for patients. In one case, a pharmacist recently worked with a patient who had been struggling to take their medications correctly. The pharmacist identified that it worked best for this patient to take his medications when his wife was present.
Without someone else present when he took his medications, he would sometimes forget if he had taken the medication or not and would then either take too much or too little, of the prescribed medication. The pharmacist was able to change the patient from an immediate release medication prescribed three times per day to an extended-release medication taken once daily. While this did not reduce the drug count, it reduced the pill burden for the patient and improved his adherence.
Pharmacy leaders integrated the data demonstrating the unique, positive impact of pharmacists on patient outcomes at Allina Health into the business plan for pharmacist MTM services, gaining organizational commitment to extend pharmacist MTM services to a new patient population.
“The data derived from Allina Health showed the value, in a very strong way, of the pharmacist participating in the care team.”
– Ann Byre, PharmD, Vice President, Pharmacy Services, Allina Health
Allina Health will continue to use data and analytics to evaluate the impact of pharmacist MTM on patient outcomes. Next, it plans to evaluate the impact of pharmacist MTM on clinical conditions affected by drug therapy, such as pharmacist driven changes to blood pressure drug therapy and the long-term impact on blood pressure control.