Mass General Brigham (formerly Partners HealthCare) developed a strategic framework for population health management, focusing on high-quality, cost-effective care for half a million risk-contracted lives. This framework enables collaboration among providers, uses unified performance targets, and integrates robust analytics to meet diverse contract requirements while enhancing patient care.
Reengineering care delivery to provide higher quality of care at a lower price is a top priority for provider organizations throughout the United States. Spurred by federal legislation, accountable care organizations (ACOs) are fast becoming one of the most common approaches to tackling federal incentive and penalty programs such as value-based purchasing (VBP). In fact, the past few years have witnessed rapid growth in the number of federal and commercial ACOs. The number of ACOs in the U.S. is now 626 (329 with federal contracts, 210 with commercial contracts, and 74 with both), while the total number of ACO-covered lives has reached approximately 20.5 million.1
One provider organization that has embraced the ACO approach to care delivery is Mass General Brigham (formerly Partners HealthCare) in Massachusetts. The integrated delivery system consists of two large academic medical centers (Massachusetts General Hospital and Brigham and Women’s Hospital), six community hospitals, five community health centers, five major multispecialty ambulatory sites, inpatient and outpatient psychiatric and rehabilitation specialty services, homecare, and more than 6000 physicians.
Located in a state that passed legislation in 2006 designed to provide health coverage and control healthcare cost growth, Mass General Brigham was well primed for the passage of the Affordable Care Act in 2010. Mass General Brigham founded a large ACO to manage risk-based reimbursement models and, in 2011, signed accountable care contracts within all major payer categories. These contracts placed a significant percentage of the organization’s revenue at risk, encouraging Mass General Brigham to hold increases in total medical expenses (TMEs) below the state average and below the growth in state domestic product.
Successfully managing these contracts required Mass General Brigham to define new organizational structures and processes for delivering care under a new paradigm. It also required a sophisticated analytic environment to enable the ACO to manage risk and optimize value.2 As an integrated health care delivery system, Mass General Brigham also needed to think strategically about growing their referral business in and out of state to meet the needs of their academic medical centers, and therefore needed trended information about volumes and other market forces. Being able to differentiate among referral sources and identify those patients referred by their at-risk population (ACO business) and that referred by other systems/ACOs is a critical analytical cut needed to understand the impact of the provider market consolidation, payer strategies and internal strategies focusing on the overall hospital business. Equally important to managing the health of a population, is the ability to be able to look at data about patients from all sources.
Because Mass General Brigham began the transformation to a new care-delivery model quite early, the ACO has now advanced to take on significant risk for its populations. In fact, the organization must agree to an annual TME target for all patient populations for which it is at risk. With its multiple contracts, Mass General Brigham is currently at risk for costs for nearly 500,000 lives—making medical expense management critically important for the organization, especially for high-risk, high-utilization populations of patients.
A robust analytics system that could operate across the ACO was essential to managing these populations.
As Mass General Brigham’s leadership assessed the organization’s IT needs, they saw significant gaps between what they had and what they needed. They did not have the ability to efficiently integrate and analyze multiple data sources from across the ACO—including clinical data, claims data and financial data—to effectively manage costs and risk. Their existing analytics environment was fragmented into three separate data warehouses (for clinical, financial, and claims data respectively) and numerous other smaller repositories, making it extremely difficult to obtain the integrated views required for effective risk and cost management.
Integrating data from these disparate warehouses was done either manually or not at all. This approach was time intensive, error prone, and frustrating. As Mass General Brigham moved further into at-risk population health management, leaders recognized that this system was neither scalable nor sustainable. They needed more effective analytics capabilities to measure performance and drive clinical transformation.
To address the challenge of transforming care delivery, Mass General Brigham embarked on a systemwide initiative to reengineer business processes and align the organization’s operations with value-based principles. This initiative—guided by strong leadership and meticulous change management—has resulted in the development and successful implementation of a strategic framework for managing at-risk populations across their integrated care delivery system.
The foundational components of this framework include the following structures, processes, and tools for delivering care under a value-based paradigm:
Mass General Brigham created a new division to coordinate the systemwide work required by risk-contracting arrangements. The Division of Population Health Management (PHM) works closely with organizational leadership at member institutions to collaboratively design and execute Mass General Brigham’s systemwide accountable care strategy. The PHM team developed capacity, infrastructure, and expertise to implement and manage a clinical strategy for the entire integrated delivery system. This included:
The health system spearheaded a multi-disciplinary governance and sponsorship approach that resulted in a high level of user adoption of and engagement with new processes and technologies. This strategy involved clinical, business, and executive stakeholders and closely engaged with the Division of PHM to ensure the information needs of the operational leaders and decision-makers were being met. As part of this process, the Mass General Brigham’s team conducted more than 100 executive communication sessions. These interviews not only increased awareness and engagement but also generated valuable feedback for ongoing design and development.
Mass General Brigham’s PHM team implemented new care models (dubbed the iCMP) to increase the organization’s capacity to manage the health of populations while also reducing growth in healthcare costs. This multi-disciplinary care model seeks to manage high-risk patients, keeping them out of the hospital in lower-cost care settings and away from expensive diagnostic and therapeutic interventions.
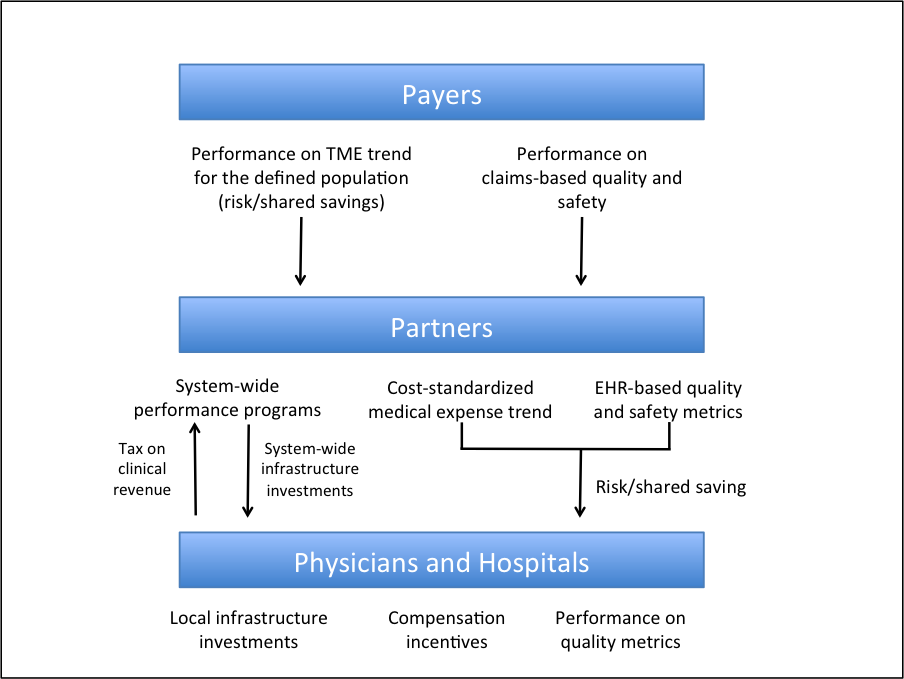
Mass General Brigham established an elegant framework to promote collaboration and align incentives among providers across the care continuum. The IPF also organized metrics to promote the best possible care for all patients while at the same time meeting the demands of multiple external contract requirements.
The IPF uses a single set of performance targets for all Mass General Brigham contracts. It rewards member institutions for (1) adopting systemwide initiatives (2) meeting external quality measure targets, and (3) limiting the growth of cost-standardized medical expenses (CSME) (Figure 1).
The approach incentivizes primary care physicians to refer patients within the Mass General Brigham delivery system where costs can be controlled more efficiently. The IPF unites Mass General Brigham specialty and primary care physicians with a common goal—to provide optimally efficient care.
To enable analysis of current performance and drive clinical transformation, Mass General Brigham implemented an analytics platform for the traditional hospital business and drivers of trends in volumes, (driven mostly by referrals at the acute medical centers), as well as for ACO, shared-risk, and population health management. This platform consisted of an enterprise data warehouse (EDW) and advanced analytics applications. Mass General Brigham implemented a late-binding EDW from Health Catalyst. The EDW aggregates clinical, financial, operational, claims, and other data to create consistent views of the data and inform decisions. It also employs common patient and provider identifiers to facilitate linkage of information about patients and providers and to easily identify high-risk patient cohorts.
On top of the EDW platform, the Mass General Brigham team deployed three advanced analytics applications that, in combination, help them understand their overall business trajectory, assess performance, manage utilization, and control costs. These applications focused on:
The strategic value of the advanced analytics applications is derived from the ability to easily explore data in a way that provides:
To deploy the applications quickly and effectively, Mass General Brigham used iterative development and incremental implementation consistent with the Agile methodology.3 This rapid prototyping of models allowed for sequential releases in short 6-8 week cycles.
The combination of an EDW and ACO/shared-risk and population health analytics applications gave the Mass General Brigham team easy access to the key strategic information they needed to inform the organization’s strategy and to support data-driven clinical, financial, and operational decision-making.
From previous experience, the Mass General Brigham team knew that access to aggregated data alone would not drive success. They also needed to build a strong base of end-user engagement and support to ensure that the information was used effectively. Therefore, they implemented a series of support services designed to help the end-user community understand what data and analytic tools were available; how to access, use and navigate them; and who could provide subject area expertise.
“Our advanced analytics applications for population health help us understand our business trajectory and effectively manage costs in the emerging at-risk environment. With costs for so many lives at risk, this insight is essential.”
- Sree Chaguturu, MD, Vice President, Population Health Management
Mass General Brigham has developed and implemented a strategic framework for managing at-risk populations and growing referral business regionally, nationally and internationally, that can serve as a model for health systems throughout the United States. With this solid framework in place, the organization is focused on continuously enhancing the functionality of its ACO/shared-risk and population health analytics applications. The team also continues to develop its analytics roadmap. They will soon conduct an assessment of the existing EDW environment to identify opportunities for data-management efficiency and cost reduction, beginning with impacts of the organization’s current EHR implementation.
Furthermore, in support of developing a culture of data-driven decision-making, Mass General Brigham is taking steps to strengthen the analytic user community. The team wants to ensure that end users are both getting the data they need and understanding it.


