MultiCare Health System launched an initiative to improve care, costs, and patient experience for patients with pneumonia. Key actions included developing evidence-based order sets and assigning social workers as "personal health partners" to improve follow-up and communication. The organization also implemented an analytics application for real-time feedback on compliance and performance while offering a single view of patient-specific data across multiple visits and care settings, such as medication and readmission histories. These efforts have resulted in significant outcome improvements.
MultiCare Health System, an integrated delivery system (IDS) serving communities throughout Washington State, recently undertook an initiative to improve the care of, cost of, and experience for pneumonia patients.
This initiative included the building of evidenced-based order sets (and driving their adoption), assigning a team of social workers called “personal health partners” to research and improve patient follow-up and communication, and deploying an analytics application to provide near real-time feedback on compliance and performance while offering a single view of patient-specific data across multiple visits and care settings, such as medication and readmission histories.
Pneumonia accounts for nearly 1.1 million patient hospitalizations utilizing more than 5.7 million inpatient days each year in the United States.1 In 2008, as part of a sweeping initiative to improve clinical outcomes for pneumonia patients, the Centers for Medicare & Medicaid Services (CMS) and Hospital Quality Alliance (HQA) began publicly reporting 30-day pneumonia mortality measures. CMS has since expanded the publicly reported outcome measures to include 30-day readmission for pneumonia, as well as implement penalty programs applied to Medicare reimbursement rates for hospitals performing poorly on these metrics.2
Senior leadership at MultiCare Health System, an integrated delivery system (IDS) serving communities throughout Pierce, South King, Thurston, and Kitsap counties in Washington State also identified pneumonia patients as a high opportunity for quality and process improvements. This was no simple undertaking for a health system with multiple hospitals and clinics and a combination of employed and community providers. MultiCare had a strong performance improvement structure in place led by physician and operational leaders, and composed of Clinical Collaboratives and Workgroups—that is, teams focused on improving patient outcomes and reducing cost in each one’s assigned clinical focus area. In February 2014, MultiCare launched a Pneumonia Workgroup under the guidance of the Medicine Collaborative to improve the care and outcomes for their patients with pneumonia.
A wide range of providers and service venues are inevitably involved in the care of pneumonia—which meant that the Pneumonia Workgroup’s membership likewise needed to be diverse and varied. Disciplines and care locations represented in the Workgroup included the emergency department, inpatient and outpatient units, transitional care and nursing home providers, physicians, nursing, respiratory, pharmacy, operations, information technology, organizational effectiveness, and physical therapy. Assuring that all players had a voice, all workflows were understood, and that patient needs were met would in turn require creative and innovative approaches to process improvement, communication, and deployment. That said, Workgroup members shared a common purpose to improve the care of their patients, and a common set of overarching goals:
To achieve these goals, Workgroup members would need to work collectively to overcome a number of challenges that stood in the way—some related to being part of a large health system; others associated with the difficulty of treating the condition itself; and all underscored by limited access to quality data.
Aggregating data for root cause analysis. The first challenge facing the Workgroup was to gather information to understand the root causes of the issues members were trying to address. To fully understand the problems and root causes, members needed to have a deep and data-supported understanding of patient flow, workflows, disease process, care routines, and patient outcomes associated with pneumonia. To monitor the sustainability of any improvements, the Workgroup would also need meaningful, easily accessible, trended metrics to provide feedback on the impact of all pneumonia treatment interventions.
Building an enterprise-wide order set for pneumonia. Based on experiences with other Collaboratives, the Workgroup determined that a standardized electronic order set was the easiest and most effective way to define best practices, while leveraging informatics to help clinicians “do the right thing.” This would require bringing clinicians to consensus on the best way to treat pneumonia across the system.
Providing faster access to data. Almost immediately, these challenges shone a light on the need for faster access to data. The existing process for obtaining information to support improvement efforts required a request to the Information Intelligence department for a custom report that would need to be checked, adjusted, and vetted before the information could be used. For each request, resources had to be prioritized and allocated, and the data validated. It could take anywhere from a couple of days to a month to get the information needed to support improvement efforts such as the Pneumonia Workgroup’s.
On the treatment side, primary care providers, too, wanted efficiency of data access. Preparing for a clinic visit required them to review multiple sources of data to gather the information needed to appropriately treat a patient with pneumonia.
To successfully address the care needs of a widespread and complex clinical condition such as pneumonia, the Pneumonia Workgroup represented a diverse range of disciplines and care locations. While having so many different stakeholders might pose a challenge in itself, the Pneumonia Workgroup exceeded all expectations. It modeled what has turned out to be a highly effective, patient-centered and outcomes-focused approach to making quality improvements for pneumonia patients.
This began with strategic background and planning work to assure the right problems were addressed. Here Workgroup members manually reviewed and analyzed charts to pinpoint the processes, interventions, and outcomes that pneumonia patients were experiencing. Concurrently, members reviewed the literature for best practice recommendations, articles, and case studies to leverage the experience and knowledge of other organizations and experts.
What became evident through intensive research and chart audits was that not all pneumonia is the same. The orders and care routines built into the order set needed to accommodate the legitimate variation and different care needs among four sets of pneumonia patients:
Once this background, data analysis, and problem identification work was complete, the Workgroup identified several key process improvement efforts:
Building a single and effective order set for use across the system. Constructing an order set that allowed variation for four subsets of pneumonia patients involved intensive work from numerous disciplines, especially pharmacy and nursing.
To identify the appropriate antibiotic for each subset, for instance, pharmacists evaluated antibiograms for specific pneumonia patient populations by facility. (An antibiogram is tool based on information from microbiology laboratory tests that provides information of how likely a certain antibiotic is to effectively treat a particular pathogen).
The pharmacists combined their findings with best practice recommendations from the literature and developed a list of appropriate antibiotics for each of their four subsets of pneumonia patients. They also determined that, in addition to selecting the right antibiotic, the right dosage and duration were equally important. As such, these recommendations were also built into the order set.
Meanwhile, Nursing and Respiratory concluded that developing a bronchodilator protocol that gave the registered nurse and the respiratory therapist the ability to modify the frequency of treatments based on symptoms would provide for more effective care. This protocol was developed and incorporated into the standard pneumonia order set.
Improving interventions while lowering the cost. A number of interventions were identified and implemented to rein in the cost of treating pneumonia while improving clinical outcomes. Among the most notable was the concerted effort to eliminate unnecessary radiology procedures. Here, too, specialists in the discipline played key roles. Radiologists researched appropriate use of radiology procedures in diagnosing and monitoring pneumonia, and then built guidance and the correct orders for each of the four subsets of pneumonia into the order set.
Engagement and adoption. As indicated in the prior examples, the order set was carefully designed to respect the workflow of individual departments. Any department whose workflow was impacted was directly involved in either designing or reviewing the final order set. Once the new order set was created, the Workgroup removed all the other pneumonia order sets that were in use, and implemented the new one simultaneously across the entire MultiCare organization. From there, analytics was used to provide feedback that indicated the level of order set adoption.
Workgroup members overcame resistance of providers to using the order set by showing them the data on their clinical outcomes and performance metrics compared to those of their peers, or systemwide results, when the order set was used.
Post-discharge follow-up and communication. Research also indicated that contacting pneumonia patients post-discharge to answer questions about their medications and confirm that they had scheduled their follow-up appointments decreased the likelihood of readmission. This patient engagement activity was undertaken by social workers, recently retitled as “personal health partners,” on the care management team.
Analytics assisted with providing the background information needed to focus efforts effectively to improve follow-up appointments and phone calls. It was originally assumed, for example, that high-risk patients would require extra care management and attention to avoid readmissions. Yet the data showed that it was the medium risk group that was most often readmitted. By focusing efforts on the medium-risk patients, the Workgroup was able to improve the overall readmission rate for pneumonia patients.
Analytics delivered new capability to correlate processes with outcomes. Being able to provide near real-time feedback on compliance and performance was key to supporting and sustaining meaningful process improvement. Publicly reported metrics were inadequate in fulfilling this purpose, due to their delay in reporting and the limited patient population included in the metrics. MultiCare recognized that it needed an analytics application that could mine the data about pneumonia patients and provide near real-time, interactive data that showed the impact of interventions on the high-level outcome metrics: mortality, readmissions, length of stay, and cost.
To this end, MultiCare partnered with Health Catalyst and deployed a pneumonia analytics application. MultiCare defined the patient cohort and the corresponding metrics to include all patients with pneumonia over the age of 18, expanding the population beyond that of the publically reported CMS metrics. The resulting application was designed to quickly and easily display data and trends to show improvement related to specific interventions—for instance, an increased order set could be correlated to a reduction in readmissions.
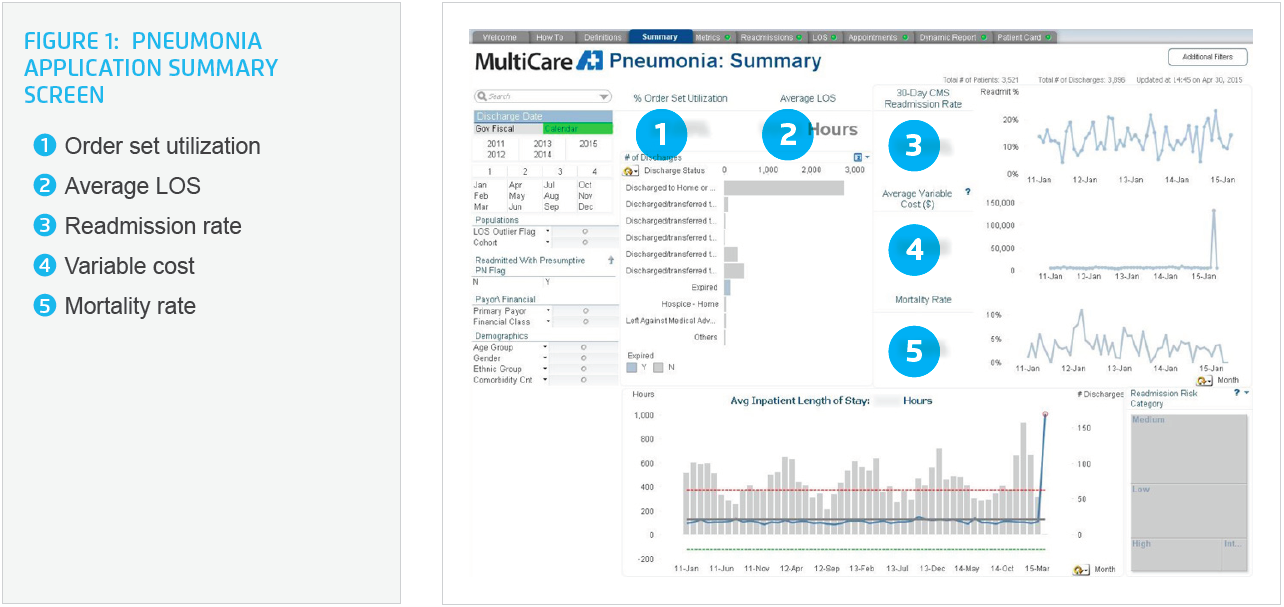
The pneumonia analytics application is used by the Pneumonia Workgroup to monitor high-level outcome measures, as well as to monitor process metrics by each team every month. In this way, the Workgroup is able to identify patterns and problem areas quickly and take corrective action almost immediately. With the pneumonia application, Collaboratives and Workgroups can interact directly with the data, which is now at their fingertips instead of two days or even a month away from accessing (see Figure 1).
A single view across medication and readmission histories. Another benefit that the analytics application provided was the ability to show information from multiple sources and care locations on one screen. The Patient Card screen in the application (see Figure 2) provides improved visibility into patient’s medication and readmission histories. What normally would have taken multiple chart reviews is now visible in one place. Importantly, providers have access to a tool that gives them the information needed to avoid prescribing the same antibiotic that was prescribed at the original admission.

To monitor the cost impact of interventions, the Pneumonia Workgroup used a charge ratio as a proxy for variable costs and included this information and length of stay on the Pneumonia Summary screen in the pneumonia application. These metrics are now easily monitored and correlated to new interventions and improvements.
The success of this Workgroup was not only what was done, but how. The Pneumonia Workgroup set a precedent for doing the work differently and used innovative methods of communication to assure a high level of participation, engagement, adoption, and collaboration across the organization and the communities that it serves. The Pneumonia Workgroup delivered the following results within one year of reaching the deployment and implementation phase of the improvement effort:
High-level outcome measures:
“As a result of the work of this team, the level of confidence that the providers have in the pharmacists has increased tremendously, and the confidence of the pharmacist with the physician as well.”
– Tasheba West, Pharmacist
The members of the Pneumonia Workgroup are determined to continue to improve the care for pneumonia patients. Among the next areas of focus are to implement the use of the CURB-65 Severity Score3 in the emergency department to identify patient risk of mortality and help determine whether inpatient or outpatient treatment is needed. To hold and advance their gains, the Pneumonia Workgroup will be doing process validation, performance monitoring, and ongoing improvement.
MultiCare is also applying lessons learned from pneumonia to Chronic Obstructive Pulmonary Disease (COPD). The health system has been able to construct a COPD order set in half the time it took to create one for pneumonia.
Additionally, MultiCare would like to expand its analytics application to include a Physician Card screen approach similar to the Patient Card screen, which would include performance and adoption metrics by provider. Leadership in Primary Care is interested in expanding the use of Patient Card by primary care physicians to assist with pre-encounter patient reviews. This could save 30-60 minutes per patient in preparation time, and increase the likelihood that correct antibiotics are ordered and appropriate care delivered. Meanwhile, pharmacy would like to continue to increase their engagement with patients to ensure smoother transitions of care for these patients.
While this list of next steps is lengthy and ambitious, the Pneumonia Workgroup has shown what it can accomplish in a short period of time and the lengths it will go to in order to improve the care and clinical outcomes for MultiCare patients. There is little doubt that this approach will continue to assure ongoing success.


