Thibodaux Regional Medical Center addressed the high costs associated with total hip and knee arthroplasties by forming a care transformation orthopedic team. The organization implemented standardized processes, educational programs, and a joint replacement analytics tool, successfully reducing cost variability while maintaining high patient satisfaction and enhancing care quality for Medicare patients.
Total Hip (THA) and Total Knee (TKA) Arthroplasty are the most prevalent surgeries for Medicare patients, numbering over 400,000 cases in 2014, costing more than seven billion dollars annually for the hospitalization alone. Today, more than seven million Americans have hip or knee implants, and the number is rising. Furthermore, substantial variation in the cost per case has raised questions about the quality of care. At Thibodaux Regional Medical Center, total joint replacement for hips and knees emerged as one of the top two cost-driving clinical areas with variation in care processes.
To address this, Thibodaux Regional maintained its focus on the IHI Triple Aim while developing organizational and clinical strategies to transform the care of patients undergoing THA and TKA. It commissioned a Care Transformation Orthopedic Team that set multiple outcome goals. Among its many efforts, the team established standard care processes, created an educational program, redesigned order sets and workflows, and deployed a joint replacement analytics application.
Thibodaux Regional reduced variability and decreased costs significantly while maintaining high levels of patient satisfaction.
Hip and knee replacement are among the most common inpatient surgeries for Medicare beneficiaries. In 2014, there were more than 400,000 surgeries, costing several billions of dollars annually for the hospitalization. The number of THA and TKA operations performed each year have been on the rise, a trend that is expected to continue. It is estimated that more than seven million Americans now live with an artificial hip or knee.1
There is also substantial variation in the cost of total joint replacement, with the average Medicare expenditure ranging from $16,500 to $33,000.2 As such, expenditures and associated quality outcomes are often under scrutiny.
Thibodaux Regional, a community hospital, experienced these same variation issues at a local level. As a recipient of the Healthgrades Patient Safety Excellence Award and the J.D. Power and Associates Distinguished Hospital Award, Thibodaux Regional has been committed to providing high-quality care, including its comprehensive orthopedic services.
Thibodaux Regional has diligently focused on the IHI Triple Aim: improving the quality of care, reducing the cost of providing care, and creating a great patient experience. To help achieve this, it had previously implemented the Health Catalyst® Analytics Platform, including the Late-Binding™ Data Warehouse and a broad suite of analytics applications, including the Key Process Analysis (KPA) application.
Using the analytics platform and KPA application, Thibodaux Regional examined all of its hospital care processes and determined where the greatest resource consumption and variation existed. Total joint replacement for hips and knees emerged as one of the top two cost-driving clinical areas with variation in care processes.
Upon further analysis, Thibodaux Regional identified sizeable variation in LOS, cost of care, and complication rates.
Thibodaux Regional needed a plan that would transform orthopedic care for its patients undergoing THA and TKA. It needed to establish consistent care processes, drive out variability, and decrease costs while improving the quality of care and patient satisfaction.
From previous improvement efforts, Thibodaux Regional has experience with the effectiveness of dedicated improvement teams, which showed that when it focused on the Triple Aim, used data-driven approaches to improvement, and provided physicians with the necessary tools to lead change by engaging cross-functional teams, it could truly transform care.
Thibodaux Regional’s Care Transformation Steering Team commissioned a Care Transformation Orthopedic Team to focus on the care of THA and TKA patients. The cross-functional team included orthopedic surgeons, an anesthesiologist, an internal medicine physician, registered nurses, clinical directors, physical therapists, a pharmacist, a data architect, and an outcomes analyst.
The Care Transformation Orthopedic Team understood that clear goals provide focus, increase motivation, improve group cohesion, and are an essential requirement to guide work and facilitate measurement of success. The team first established outcome goals, including:
With the goals in place, the Care Transformation Orthopedic Team researched evidence-based practices across multiple disciplines and evaluated various strategies to improve patient safety, reduce complication rates, and improve patient education. The team planned how to change perioperative care, established standard processes, and discussed various strategies to ensure all patients received appropriate medical clearance prior to each procedure. The transformation included multiple, far-reaching, ongoing efforts:
The Care Transformation Orthopedic Team used the Health Catalyst Joint Replacement – Hip and Knee improvement application to monitor performance and the outcomes associated with its improvement work (see Figure 1).
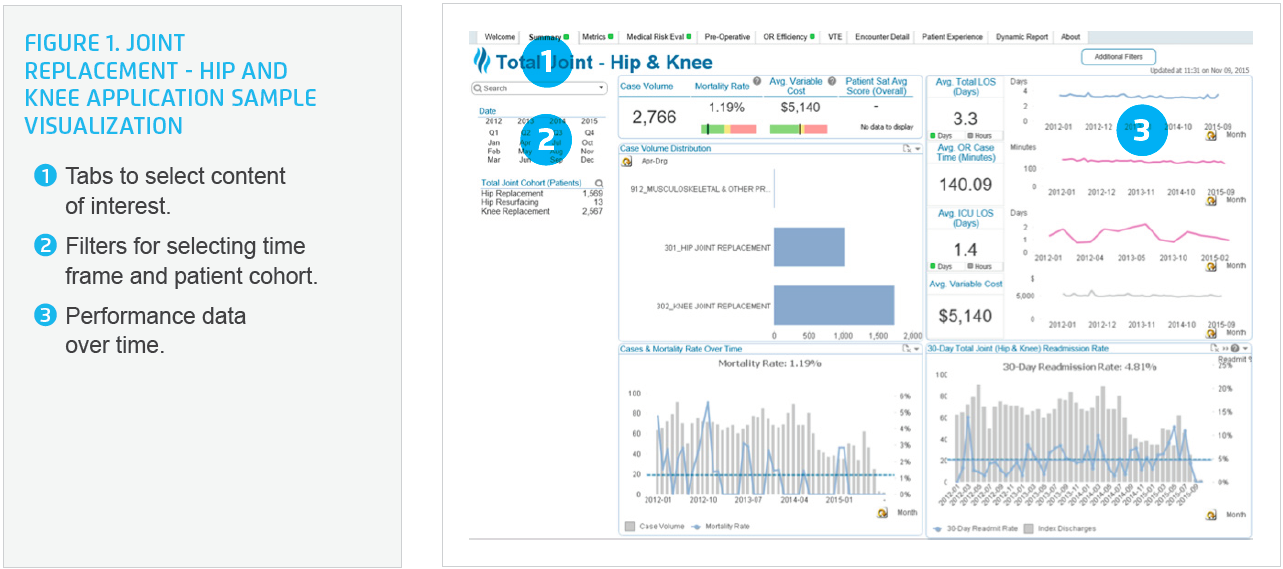
The analytics application provided near real-time data, giving the team valuable insight into complication rates, average variable cost, length of stay, compliance with the newly defined pre- and postoperative processes, and patient satisfaction. The team could immediately see the impact of their work on outcomes, which increased stakeholder commitment and willingness to change.
Thibodaux Regional successfully transformed the care processes and outcomes for patients undergoing hip and/or knee joint replacement. Results include:
“Data transparency helped make the case for change with the physicians. When we were able to see our individual performance in comparison to our peers, it motivated us to want to do better.”
– Dr. David Elias, MD, Orthopaedic Surgery
Thibodaux Regional plans to continue its focus on the Triple Aim, using data-driven approaches to transform care. The Care Transformation Orthopedic Team is exploring opportunities to further decrease the costs within the operating room.




