Over one-third of women in the U.S. have undergone a hysterectomy by age 60. Recognizing this, healthcare systems are enhancing women’s health services for better care and cost efficiency. UPMC established a comprehensive Women’s Health service line supported by strong leadership, an enterprise data warehouse, and an activity-based cost management system.
By the age of 60, more than one-third of women in the United States have had a hysterectomy. Healthcare systems across the country are recognizing that organizing Women’s Health as a service line offers a pathway to improving care and decreasing cost for these patients. Having accurate activity-based costing information is necessary to uncover opportunities for clinical practice improvement and cost reduction.
The University of Pittsburgh Medical Center (UPMC) made the decision to organize Women’s Health as a service line across the entire health system. UPMC fortified this approach with strong and collaborative leadership, an enterprise data warehouse, and an activity-based cost management system.
As health systems all over the country seek to decrease costs while improving care, more and more are turning to service line management as a solution. Organizing along service lines in healthcare naturally leads to the use of evidence-based medicine to create metrics, protocols, and care pathways that reduce unwanted variations in care and improve patients’ experiences and outcomes.1 To be effective in achieving cost reduction, service line managers must have an ongoing understanding of cost and revenue drivers—which spurs the need for accurate activity-based costing information.
The University of Pittsburgh Medical Center (UPMC), a large health system with over 20 hospitals and 500 clinics in Pennsylvania and additional sites in other states and countries, has embarked on a journey to implement the service line management approach in conjunction with activity-based costing. One of the health system’s first and most successful service lines was Women’s Health—an area with considerable clinical complexity and potential variation of care across the clinics and hospitals. For instance, hysterectomy is the second most frequently performed surgical procedure, after cesarean section, for women of reproductive age in the United States. Approximately 600,000 hysterectomies are performed annually in the United States, and approximately 20 million U.S. women have had a hysterectomy.2 Put another way, by the age of 60, more than one third of women in the United States have had a hysterectomy.
Changing from traditional hospital and unit-based management to service line management requires a new concept of physician leadership. In the service line paradigm, physicians shift focus from their practice groups to a more systemwide view of their specialty area and the full continuum of care for their patients. Here, a wide base of physician engagement is essential to assure adoption of care pathways and protocols. This in turn requires accurate, actionable information that clinicians trust to inform decisions and support changes in practice. To be truly useful, this data must be viewable by service line, subservice line, hospital and physician services, and be available at the patient level.
This access to data and analytics is essential in identifying opportunities for improvement. Equally important is the development and adoption of best practices in operations and clinical care—through policies, procedures, protocols, and care pathways. This is especially important in a Women’s Health service line, which, with its focus on obstetrics and gynecological services, is inherently complex and includes practitioners across multiple specialty areas and care across many venues. Further, for obstetric patients, the service line must account for the care and outcomes of the neonate, as well as the mother.
After the decision was made to organize Women’s Health as a service line, UPMC fortified the new approach with strong and collaborative leadership—aided by analytics—to make cost and care improvements.
UPMC incorporated experts from all areas of the organization including clinical care, operations, and finance to guide the Women’s Health service line. Specifically, this leadership structure includes three operational leaders (physician leader, executive administrator, and the chief nursing officer) and a financial lead.
The clinical and operational leads of the service line are responsible for developing new models of care using evidence-based clinical pathways. Their goals are to move from a volume to a value mentality and approach, improve clinical outcomes and quality of patient care, and assure that initiatives are driven by physician leadership. They also drive the move to more efficient use of resources and effective cost containment, accomplished by reducing unnecessary variation in physician and operational practice. To that end, operational leadership is responsible for making physicians aware of cost while improving quality, standardizing protocols, policies, and clinical pathways, and increasing physician engagement and subsequent adoption of practice changes.
The role of the service line financial lead is a key component of the transition from hospital-based management to service line management. This role serves as the primary contact for all financial matters for Women’s Health and collaborates with other financial areas such as supply chain. Additionally, the service line financial lead supports clinical leaders, provides the financial overview, develops and monitors goals, and supports cost management development.
The financial lead also aligns clinical, financial, and operational service line goals through a service line reporting framework that:
In order to support the financial lead and provide the service line leadership team with the detailed information and financial reports that they needed, UPMC developed its own unique activity-based costing methodology. This methodology associates different costs with patients based on the way they move through their various care locations, thus enabling UPMC to identify operational nuances that would otherwise go undetected. Service line leaders bring their individual expertise to the table to figure out the implications of the information that the activity-based cost management system uncovers.
Finance has played a key role in supporting service line reporting and analysis using activity-based costing information. Clinicians provide the insight needed to interpret the costing information, derive cause and effect relationships, and identify actions that need to be taken. Because of the complexity of Women’s Health, UPMC needed to identify and report on multiple sub-service lines in order to get to actionable data. Here the expertise of the operational leaders was essential in identifying meaningful sub-service lines. For example, they needed data not only at the level of “hysterectomy” but also by the type of procedure used in the hysterectomy: open, robotic, vaginal, or laparoscopic (Figure 1).
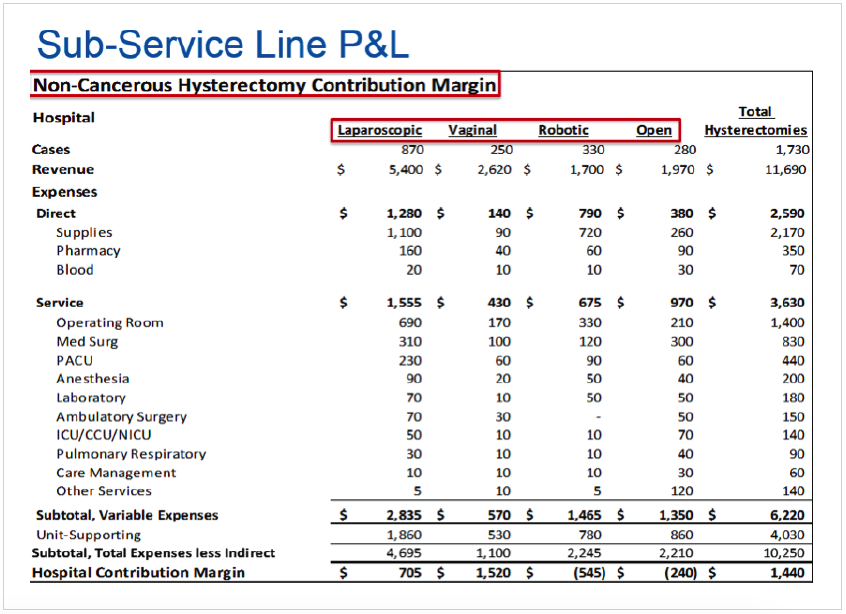
By designing their sub-service lines in ways that are meaningful to clinicians and operations, and being able to view standard reports based on those levels at consistent intervals, operational leads gained a deeper understanding of the services they provide.
Standing reports for the Women’s Health service line are enabled in part by an enterprise data warehouse and activity-based costing data mart. These reports include a quarterly service line financial packet that compares service line trends to actual, projected, and, in FY17, the budget; service line and sub-service line margin reports to help understand the cost of various procedures; physician cost and quality dashboards to identify variation; and other financial analysis and metrics to help uncover areas of potential opportunity.
UPMC has taken care to build the leadership team’s skills in analyzing these reports to identify practices and procedures that indicate potential savings. Using this approach, the Women’s Health service line quickly zeroed in on two opportunities that became its first improvement initiatives— the use of open surgical techniques for hysterectomies, and length of stay (LOS) variation for noncancerous hysterectomies.
The initial focus for service line leaders was the use of open procedures for non-cancerous hysterectomies. There was a general feeling among clinicians that this procedure was being overused, but they needed more information to guide a recommendation for practice changes that would improve outcomes, decrease cost, and best serve their patients.
By using the new reports and analytics capabilities to look at the data for FY12, Women’s Health was able to see that 28 percent of non-cancerous hysterectomies were performed as open procedures, even though open procedures had a higher cost (approximately $2,000 more than minimally invasive hysterectomies) and less favorable outcomes. (Complications, transfusions, infection rates, and readmissions were higher for open hysterectomies. Additionally, LOS for open hysterectomies was about three days, while other surgical techniques done minimally invasively were less than one and a half days. It also took open hysterectomy patients up to two and a half weeks longer to return to work. (Figure 2)
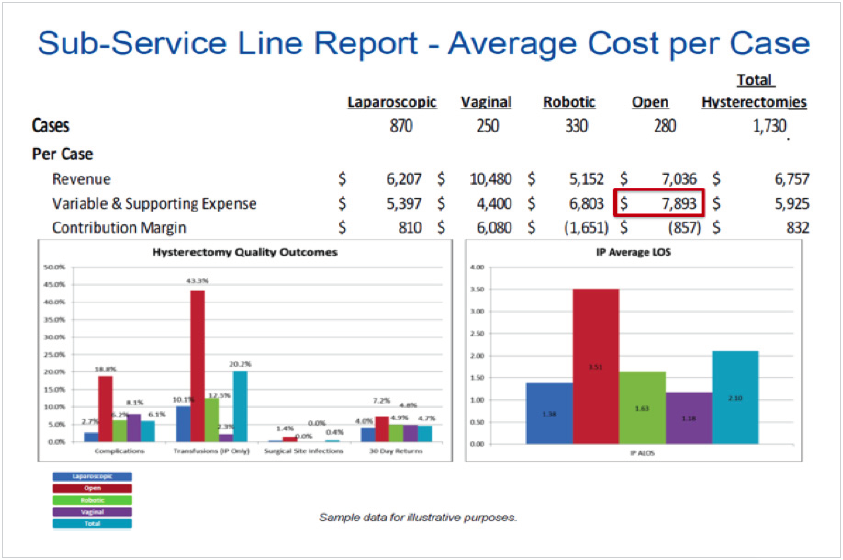
Service line leaders next turned their attention to identify opportunities to reduce time spent in the hospital post-surgery. They were able to do this by combining information about financial performance, quality outcomes, and LOS for minimally invasive, and non-cancerous hysterectomies.
Service line leaders discovered that while outcomes were the same whether patients had same day surgery or stayed overnight, the cost for the latter was much higher. This insight allowed the service line leaders to evaluate the practice of routinely keeping all patients overnight for minimally invasive, non-cancerous hysterectomies. Clinical criteria was developed to determine which patients were candidates, as well as protocols that would facilitate same day discharge.
Prior to having activity-based costing and service line reports, the need for this change was hidden by incomplete and fragmented information, as well as a lack of transparency which made it almost impossible to view information across the organization or the patient care continuum. With the information now at hand to leverage and make the case for changing both LOS and open hysterectomies, the service line took the steps outlined below. (Figure 3)

Supported by analytics, UPMC was able to provide to the practitioners a correlation between clinical and operational practice, patient outcomes, and cost. During this time, the clinical service saw a 25 percent improvement in their contribution margin. By leveraging a combination of service line management and activity-based costing, Women’s Health achieved the following results:
20 percent reduction in inpatient LOS for hysterectomies from F12 to FY15.
34 percent reduction in open surgeries for hysterectomies from FY12 to FY15, which includes a 9.3percent reduction between 2014 and 2015.
28.3 percent reduction in 30-day readmissions for open hysterectomies from 2014 to 2015.
A 200 percent increase in same-day hysterectomies as a result of a pilot program, led to an estimated cost savings of $250,000. Voluntary adoption of the program’s protocol has resulted in 67 percent of the prior year’s same day surgery volume being achieved by Q2 FY16.
“Instead of Finance coming up with ideas and putting them out there, we work with a group of physicians as a sounding board to go through the data, understand it, and identify areas of opportunity. Then they go back and sell those ideas to the other physicians.“
– Paula Lounder, Director, UPMC Payer Provider Programs
UPMC’s work with improving hysterectomies is not yet done. The health system plans to decrease overall hysterectomy utilization and reduce physician variability in supply usage. UPMC also intends to expand focus on the obstetric population to reduce variability in prenatal care, develop protocols for inpatient management, reduce Cesarean sections not medically necessary, reduce NICU costs, and enhance education. With a winning combination of service line management and activity-based costing, UPMC will continue to improve patient care and set an example for other healthcare systems to follow.
In January 2016, UPMC and Health Catalyst announced an agreement in which Health Catalyst licensed for commercial use an activity-based cost management system developed by UPMC as part of its effort to advance patient care while lowering costs. On February 29, 2016, Health Catalyst announced the close of a Series E capital raise that was co-led by UPMC, which is also a Health Catalyst customer.


These results were obtained during a time when this clinical service saw a 25 percent improvement in their contribution margin.


