Rising denials, outdated tools, and siloed workflows put margins at risk. Today’s revenue cycle must be transparent, data-driven, and connected across teams. Health Catalyst equips revenue leaders with integrated data, real-time insights, and embedded workflows. From audit readiness to denial prevention, we help turn operations into a strategic advantage.
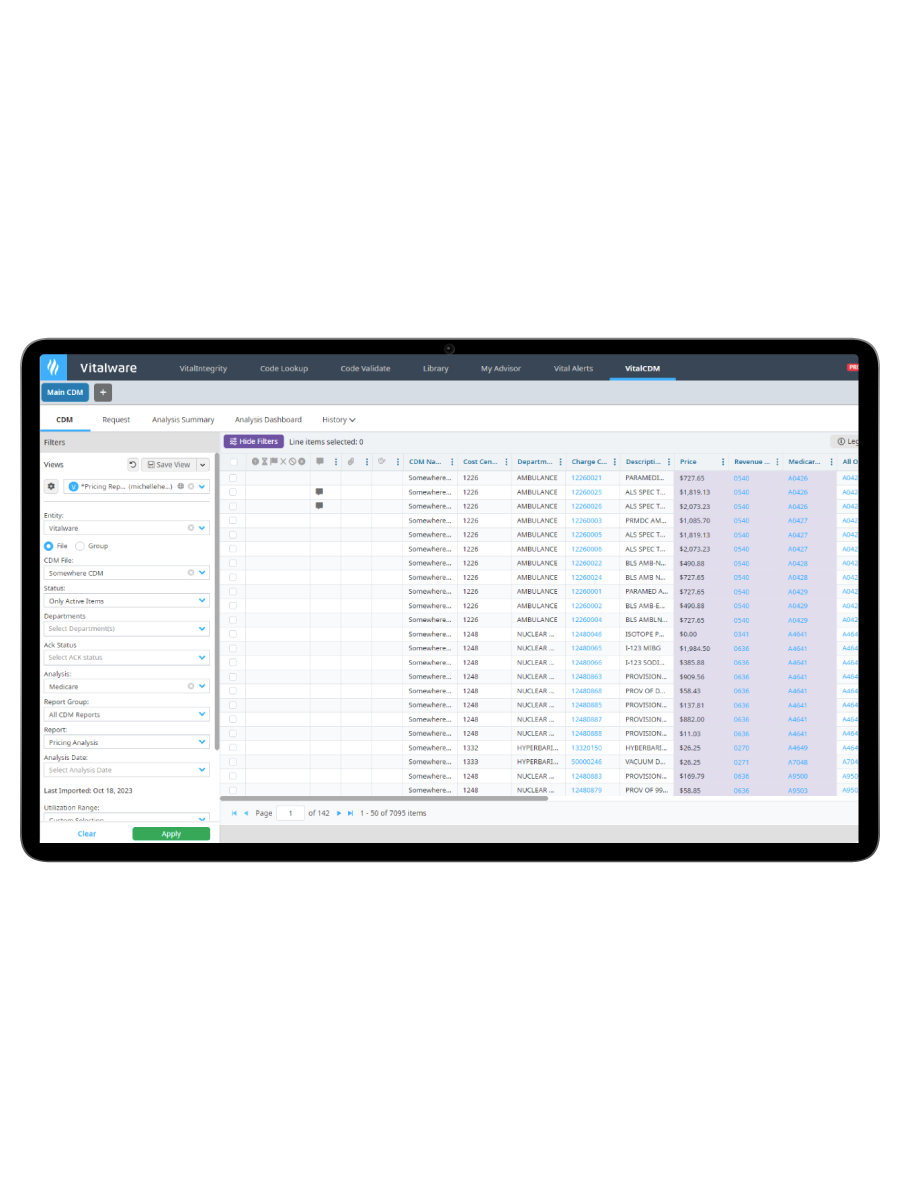
Bridge the disconnect that causes missed charges, inefficiencies, and downstream revenue risk.
Result: Fewer missed charges and tighter clinical-financial alignment.

Keep up with evolving payer and coding requirements without burning out your team.
Result: More confident decisions, fewer errors, and stronger compliance.

By combining powerful analytics with trusted reference data, Health Catalyst empowers teams across the revenue cycle to make smarter decisions, faster. From finance to compliance to clinical operations, everyone gets the visibility and tools they need to drive integrity and protect reimbursement.
Surface hidden revenue leakage with advanced analytics and root-cause insights.
Result: More revenue retained and fewer audit surprises.
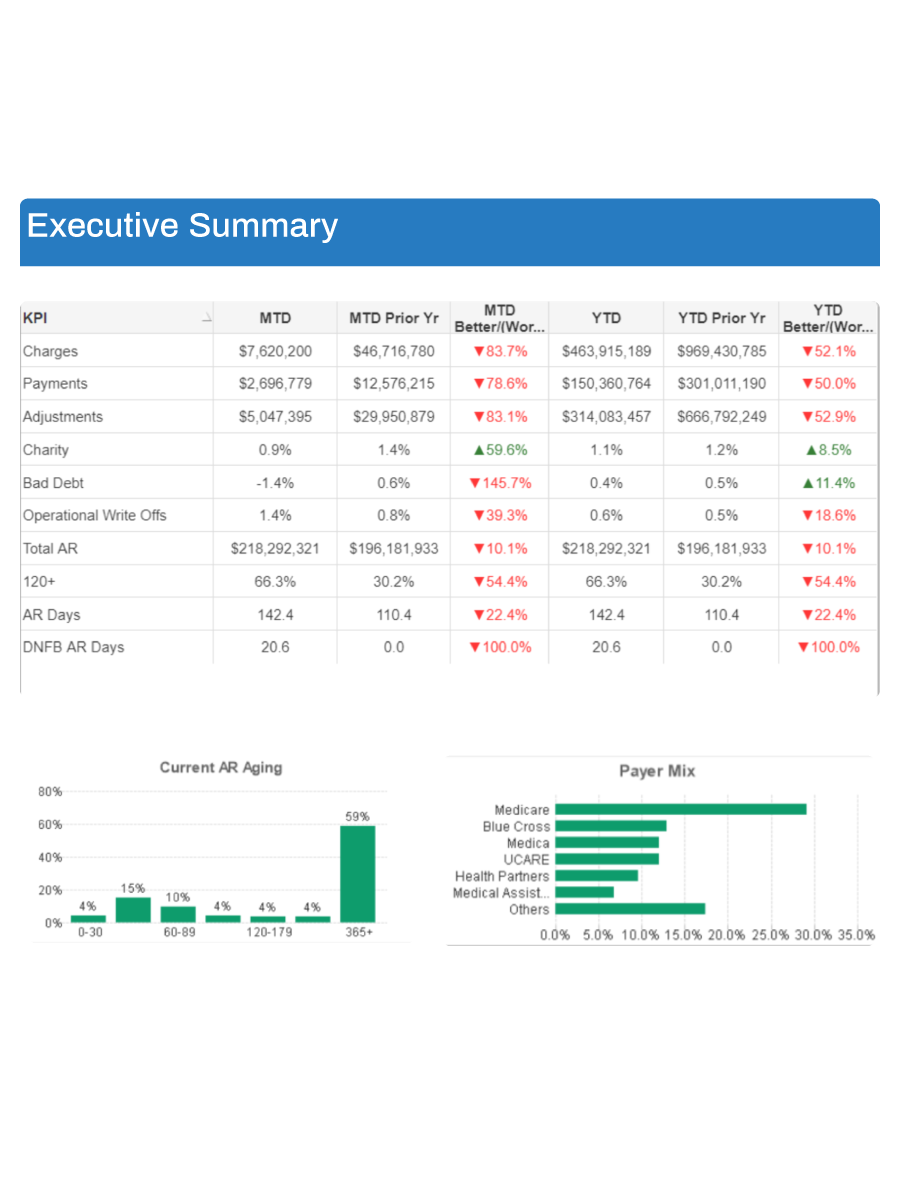
Break the cycle of rework and delay with the insights needed to stop denials at the source.
Result: Fewer denials, faster payments, and stronger revenue resilience.




