To succeed in today’s rapidly evolving business environment, healthcare organizations must have accurate financial data. Approximately 50 percent of CMS payments are now tied to a value component; hospital operating margins are at an all-time low; and consumer demands are rising with their costs.
In order to meet these new challenges, health systems must shift their strategy or risk being left behind. This article details the operational, organizational, and financial strategies that drive financial transformation, as well as examples of how to obtain and utilize financial data, find waste reduction opportunities, and much more.
This report is based on a webinar presented by Steve Vance, MBA, FHFMA, on October 30, 2019, entitled, “Why Accurate Financial Data Is Critical for Successful Value Transformation.”
The shift towards value and consumerism in healthcare is pushing providers to adopt new financial mindsets and strategies. Approximately 50 percent of CMS payments are now tied to a value component. The CMS Innovation Center has allocated nearly $5.4 billion to implement 37 value-based payment models, with 55 percent of those funds marked for development and implementation of additional value-based models. In order to succeed in today’s rapidly evolving business environment, healthcare organizations must have—and leverage—accurate financial data.
Since 2013, Medicare dollars at risk has increased steadily in the areas of hospital-acquired conditions, readmissions, value-based purchasing, and meaningful use. While some may argue that health systems aren’t yet realizing the benefits, in reality many organizations aren’t employing the necessary strategies and tools to be successful in this value proposition. The shift from volume to value varies across the country and by institution, but experts estimate that approximately 15 percent of payments nationwide are based on value rather than fee-for-service (FFS). Organizations that are unprepared for this shift will be left behind once they reach a tipping point of roughly 26 percent of total payments tied to value-based care (VBC).
The shift from volume to value necessitates a corresponding shift in incentives. In a FFS world, providers’ financial incentives are tied to higher volumes. In contrast, VBC shifts providers’ incentives to keeping people healthy and maintaining healthcare utilization at appropriately low levels. Living in both a FFS and a VBC world creates conflicting incentives, placing payment models at odds with one another, but providers can thrive if their organizations have the right tools and data to manage these competing incentives.
Providers and healthcare organizations aren’t alone in taking on more financial risk. Consumer healthcare costs have increased by more than 25 percent since 2014, largely due to an increase in high deductible health plans, and consumers are also paying more for health insurance as plan premiums continue to rise. As a result, healthcare users are increasingly demanding cost transparency and convenience. In order to meet these rising demands, health systems must shift their mindset and strategy, or risk being left behind.
As healthcare organizations embrace new payment methodologies, they must have accurate financial data. According to the Healthcare Financial Management Association (HFMA), not-for-profit hospital average operating margins are at an all-time low of 1.6 percent, and approximately 30 percent of those hospitals are operating at a loss. While many healthcare organizations focus on increasing topline revenue, eliminating waste can be more impactful, providing as much as a 50 to 100 percent contribution per dollar saved.
The first step to reducing healthcare costs is understanding the current costs. Knowing profitability, operating margins, and the various components that drive these margins is key. Healthcare organizations should understand cost drivers at all levels of the organization, down to a department or even procedural level. Having accurate data is crucial in gaining providers’ trust. When reviewing and comparing data such as cost-per-case between clinicians, healthcare leaders must be able to trust and easily understand the data presented. Additionally, organizations seeking to reduce waste need to trust the accuracy of data that shows those opportunities exist.
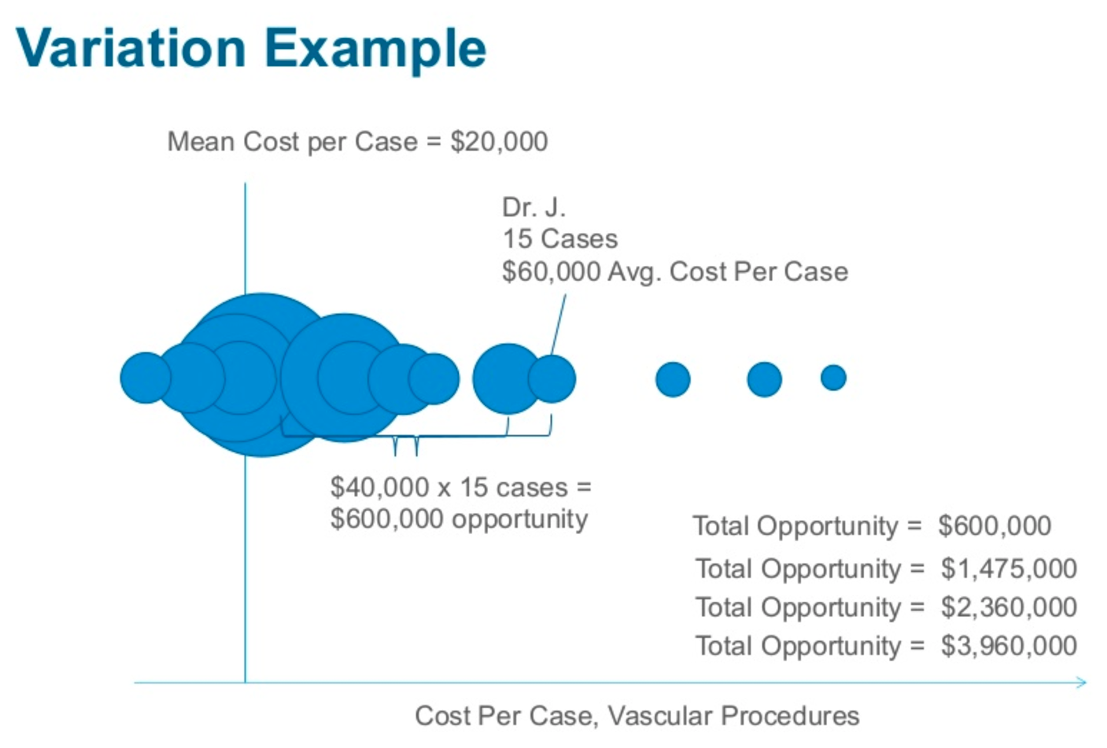
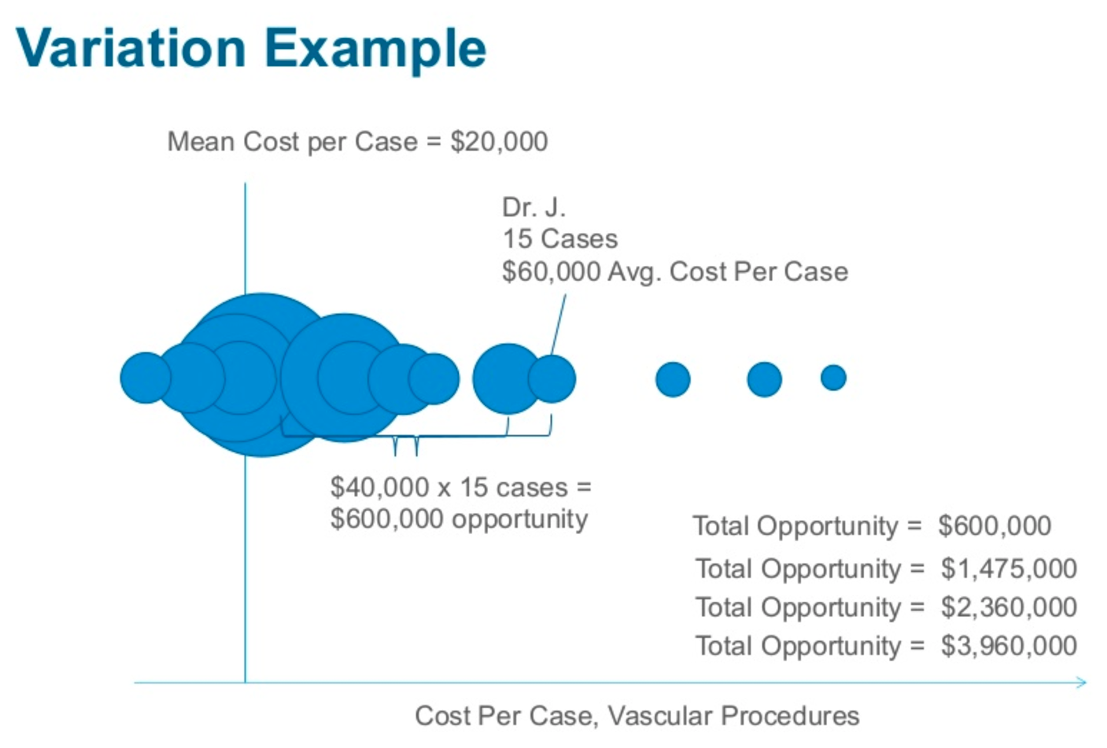
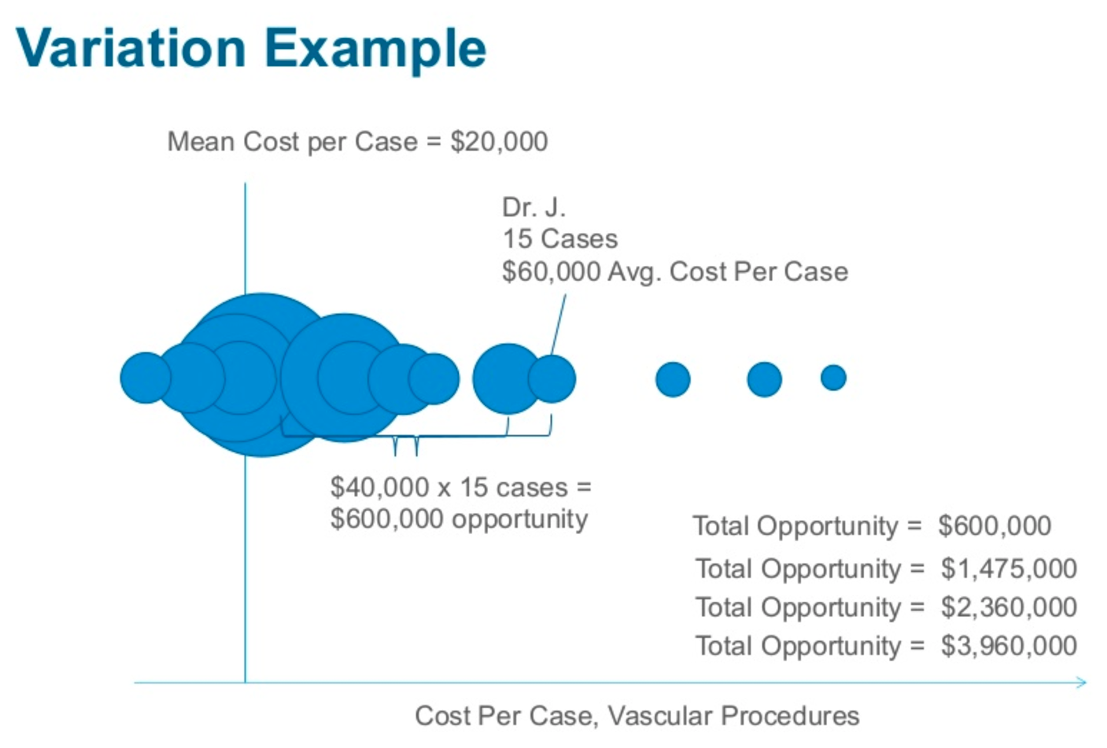
After addressing some of the low-hanging efficiency improvement opportunities, healthcare organizations can dig deeper into the data to uncover more significant areas for waste reduction. This might include identifying variation in provider expenses and patterns such as operating room minutes, implant costs, and many others. Figure 1 illustrates one such example. In this vascular procedures cost-per-case example, the user (Dr. J.) has 15 cases with a $60,000 average cost-per-case. The mean cost-per-case is $20,000. That difference of $40,000 times 15 cases represents a $600,000 opportunity.
Healthcare organizations can employ certain tactics for successful value transformation, including operational, organizational, and financial strategies. Accurate financial data is crucial to the success of each one.
Healthcare financial transformation can’t happen without constant measurement and evaluation. The following operational strategies can help organizations cut costs and improve care:
Individual efforts alone won’t result in sustained improvements. Successful initiatives require systemwide support and the backing of senior leadership, which the following organizational strategies illustrate:
Quality and cost improvements require informed use of both financial and clinical data in the following financial strategies:
The above operational, organizational, and financial strategies will help healthcare organizations begin their transformational journey, but to succeed, they’ll need tools to improve quality and efficiency. The following Health Catalyst tools and resources support organizations on the data-driven journey to massive clinical, financial, and operational improvements.
First, the cloud-based Data Operating System (DOS™️) is a healthcare-specific, open, flexible, and scalable data platform that provides customers a single comprehensive environment to integrate and organize healthcare data. Then, a suite of analytics applications built on top of DOS allows customers to make measurable clinical, financial, and operational improvements.
The CORUS® Suite is especially important to obtaining accurate financial data. This activity-based costing application accurately calculates cost based on activities, whereas other costing tools base cost on work relative value units (RVUs) or a percentage of code charges. CORUS uses more granular data to provide an accurate, comprehensive view of all the organizations’ costs, enabling users to identify actionable insights into the real drivers of cost variation. Figure 2 shows a sample report from CORUS that combines both clinical and financial data about hysterectomies.
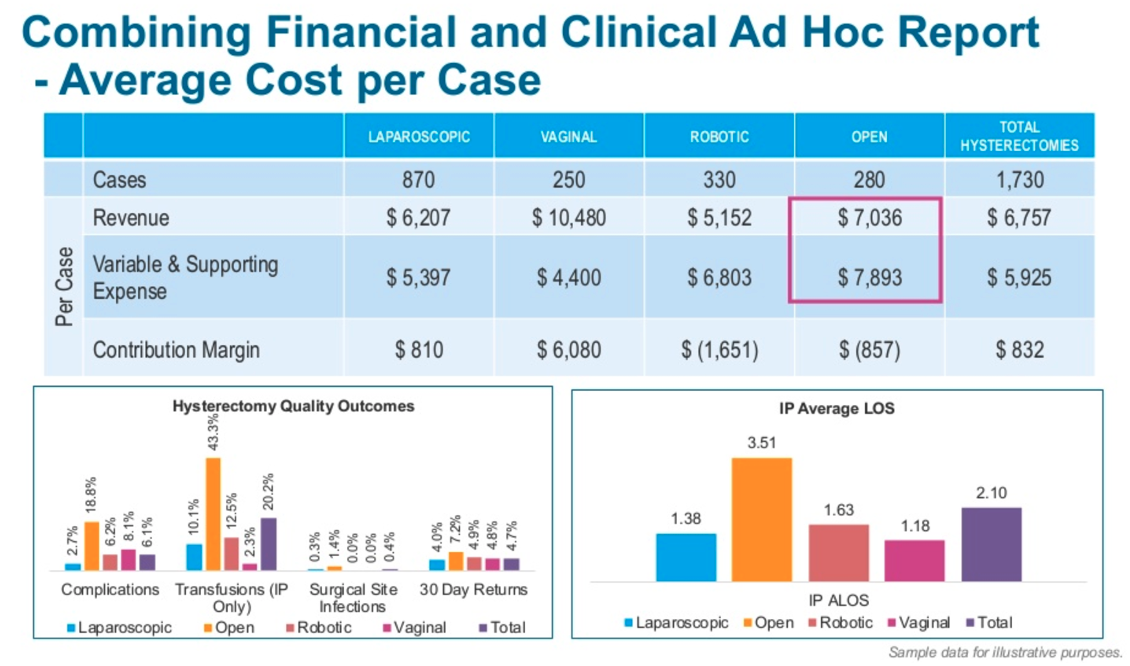
In this sample report, hysterectomies overall contributed a positive $800. Drilling down, however, the user can see that, depending on technique, there are significant differences in cost, contribution margin, and outcomes—showing why combining profitability with accurate financial and clinical data is so important in seeing a holistic picture of the total cost of care.
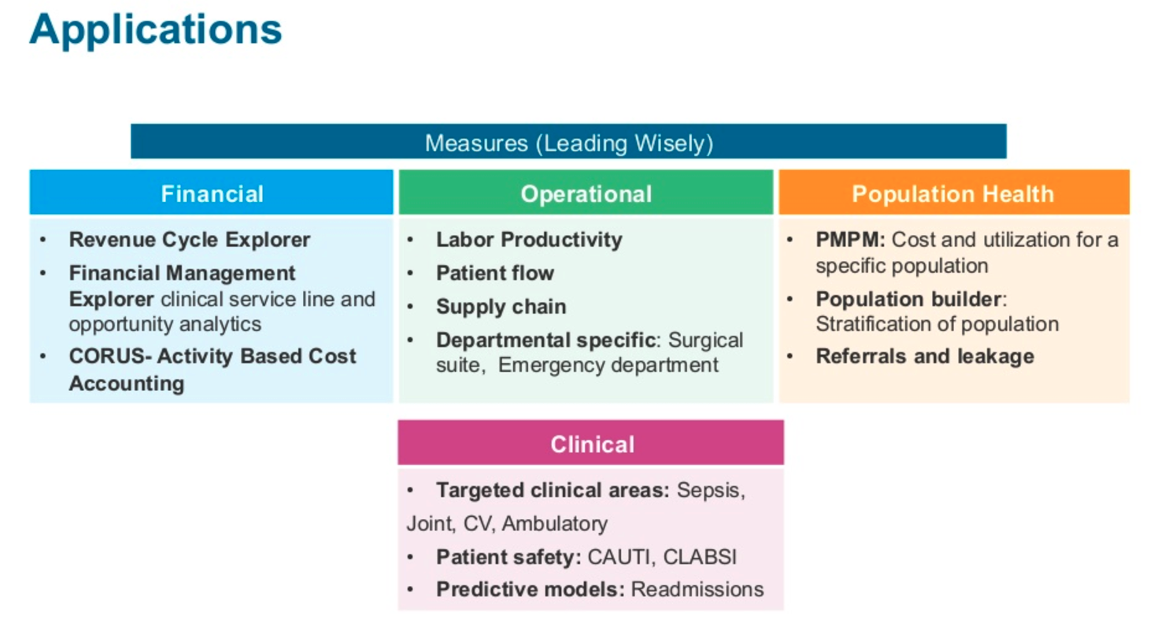
Health Catalyst offers a comprehensive suite of financial applications, such as Revenue Cycle Explorer and Financial Management Explorer, as well as powerful operational and clinical applications, giving health systems the tools they need for healthcare financial transformation. Figure 3 shows a sample of the applications that work together to provide accurate financial data and insights needed for value transformation.
As the healthcare industry moves further into pay for value, organizations need to shift their strategy and mindset to deliver the best care at the lowest costs. Accurate financial data is critical for any successful value transformation and enables strategic decision making and goal alignment across the organization. Health systems must invest the time and resources to obtain and leverage the data needed for sustained transformation. Organizations must also have a clear long-term vision for financial viability that includes a path to providing high-quality, affordable healthcare. A robust analytics platform combined with operational, organizational, and financial strategies translates to sustained success in the world of VBC.