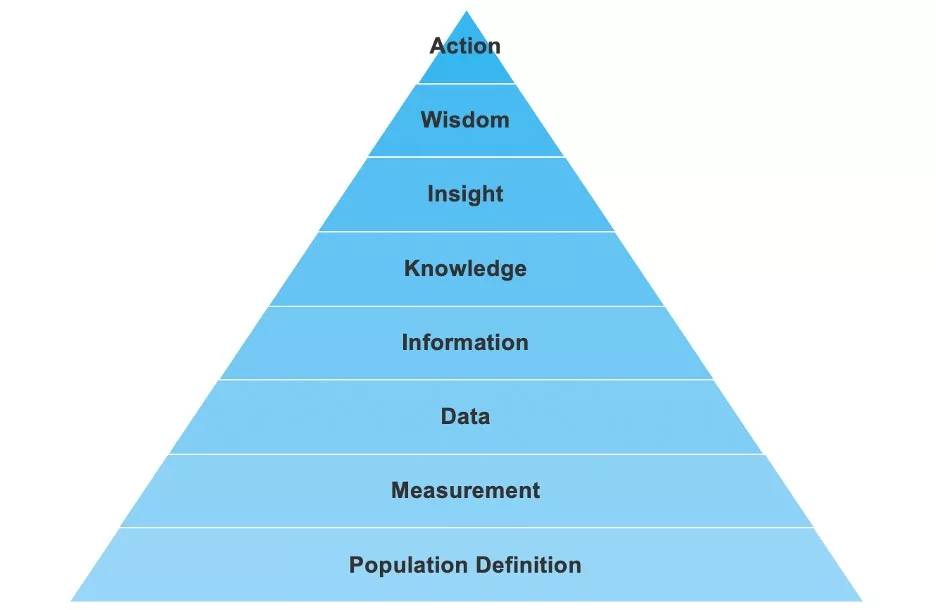
Becoming a data-informed healthcare system starts with raw data and ends with meaningful change, driven by raw data. Health systems can follow an eight-step analytics ascension model to transform data into intelligence:
1. Population Identification and Stratification
2. Measurement
3. Data
4. Information
5. Knowledge
6. Insight
7. Wisdom
8. Action
Following the analytics ascension model allows improvement teams to avoid feeling overwhelmed, focus on each step, and see how each step fits into the overall objective, allowing health systems to maximize data.
 Download
Download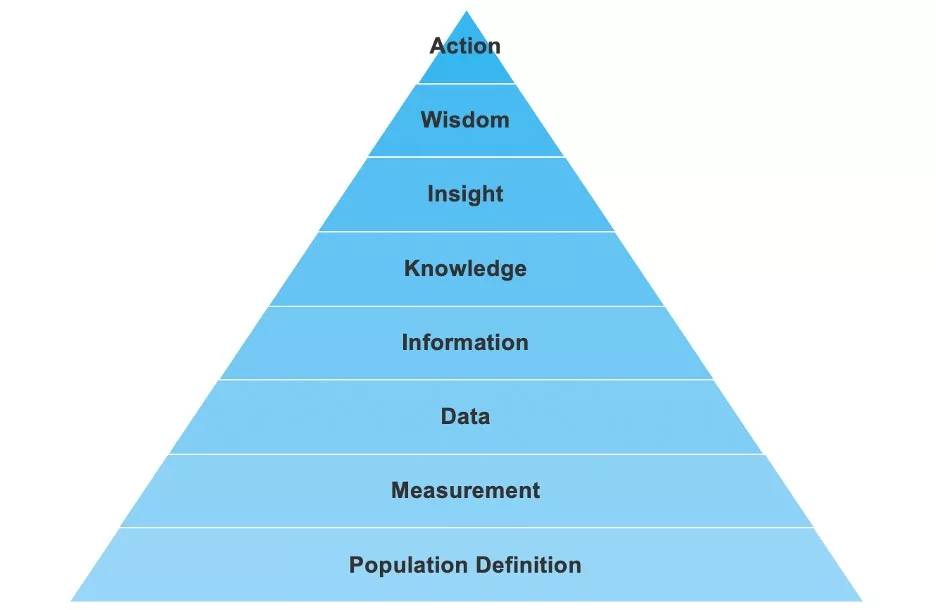
“Data driven” and “data informed” are current buzzwords in healthcare—but what do these terms actually mean for a health system? The process of becoming data informed is complex; it requires a health system to take data —in its raw form—and transform it into intelligence that should lead to action. Transforming data into intelligence is invaluable in healthcare because it is a reliable and repeatable way to identify areas for opportunity (clinical, financial, etc.) and improve outcomes.
A robust analytics platform is critical for providers to deliver data-informed healthcare that leads to better outcomes. However, if healthcare leaders and organizations do not approach the platform with the correct understanding of how to transform data to intelligence, process improvement measures will not reach their full potential and outcomes improvement may fall short.
One example of the process to turn data into intelligence is an analytics ascension model (Figure 1)—an eight-step hierarchy that guides health systems through the process of taking raw data and turning it into meaningful action, or intelligence. The process enables data analysts to develop muscle memory they can rely on as they drive data-informed healthcare decisions in everyday projects or when working as part of a larger framework, such as the 8-Step Improvement Science Model or the Healthcare Analytics Adoption Model.

For example, an improvement team may become blocked in the first phase—attempting to agree on an accurate definition of their population—but the ascension model helps team members progress by reminding them of the purpose of the current step and allowing them to see the next step. The model provides a conceptual framework for tracking progress from data to intelligence and can serve as a common language for all team members.
In step 1, improvement teams need to identify and define the patient population they are trying to influence. Typically, health systems will develop populations based on similar diagnoses (e.g., diabetes patients, heart failure) or procedures (e.g., hip surgery, orders placed, medications administered). Regardless of the target population, teams must define who or what they want to impact or change.
Agreeing on a population definition at the start of project increases project buy-in and makes it easier to gain insights from brainstorming and problem-solving meetings because every team member is focused on the same population definition. Teams will also avoid wasting time in subsequent steps by not having to revisit the population definition each time they review a new measure or result. Having a shared and thorough understanding of the target population will pay dividends as the work progresses.
In step 2, measurement, as teams work to discover and define data elements of interest for the population (e.g., frequency of specific events or a lab result), they must understand what they can currently know about the population. Understanding which data elements are available in various source systems will allow teams to quantify any gaps they may have for measurement. If teams cannot measure or make reliable observations of needed data elements, the improvement work may not be meaningful.
If a project starts without a defined understanding of the specific data elements needed to develop measures of interest (a common scenario), project teams can create a thorough documentation of the data exploratory process. This can help the team understand what knowledge they can track about the patient population defined in step 1.
It is also important to make provisions for missing data within the defined population. Patient populations may not have certain data elements available to them because of different hospital workflows, regulatory requirements, etc. For example, Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) are patient surveys that rely on volunteer participation. If only half of the defined population has replied to the HCAHPS survey, the team may lack sufficient HCAHPS data to understand their full population.
The improvement team should discuss examples like HCAHPS because these scores can be easily overlooked and impact the accuracy of the data as teams progress through the ascension model. In some cases, discussions about measurement and the data available may prompt adjustments to the patient population (step 1) or the measures selected.
In step 3, teams start to retrieve data elements they defined in step 2 and evaluate quality against other known data sources (internal or external). There may be times when comparing directly to benchmarks is not possible. Therefore, teams may substitute their own measures in place of similar benchmark values where appropriate (e.g., emergency department metrics or a functional evaluation test).
Teams can now start to validate actual data to assess quality (e.g., outliers, missing data, or use of free text fields), then clean the data to ensure it is accurate and reliable. It is important for teams to condition the data because any statistical testing that has too many outliers or empty fields can result in inconsistent, misleading, or erroneous information.
In step 4, teams aggregate, stratify and trend the trusted data to compare performance across categories. This is the first time teams would perform a statistical test on the data elements. For example, it would be the first time a team member would see the median length of stay for their patient population or the average time between two workflow timestamps. Access and exposure to the real information allows teams to check anecdotal understanding against the verified information from their own dataset, setting the stage to adjust expectations.
Often, the information may differ from the team’s expectations resulting in concerns with the population definition. Team members may think: “Where did we go wrong in our process? Who’s to blame?.” However, if team members were properly engaged in the data retrieval and validation process (steps 2 and 3), they will be ready to entertain and accept information that is different from what they expected, having a posture of learning from the information rather than projecting onto it.
In step 5, teams compare their outcome measures against a set of balancing measures, process measures, and potential drivers, such as risk or acuity. This allows teams to achieve a broader awareness of their organization and make connections between other projects happening in the organization. Team members should ask, “How does this give me new context for other work experiences and how can I incorporate them?.” For example, a team focused on reducing readmissions may also consider length of stay as a correlated component in the system and will want to understand the work and priorities happening in that adjacent space.
The “Knowledge” step is also known as the information layer because team members are starting to see possible explanations of the why behind given performance or certain challenges in the organization (e.g., poor patient satisfaction). Having a robust set of project measures—including outcome, process, balancing, component, and explanatory measures—will help this step be successful.
Team members learn to trust the information in this step, weighing the new knowledge against what they already believe to be true, and have the opportunity to receive additional context that will provide a more robust set of perspectives on the project.
In step 6, improvement team members view the results in the context of benchmarks, literature, and other considerations within the organization. The leader who is accountable for the performance the specific project is targeting should have a vested interest in knowing how other health systems perform. In particular, if a project is meant to support an ACO network or address specific CMS recommendations, then having an understanding of how other systems perform will help establish the magnitude of potential penalties or shared savings.
When leaders fail to review the results in proper context, they miss out on understanding that other organizations are experiencing the same challenges and have the same objectives. Discovering shared challenges among peers can be encouraging for leaders because they understand they are not alone when facing this problem; leaders also gain a community to work with and share knowledge, frustrations, and wins. Since health systems generally share the same vision of improving patient outcomes in one form or another, applying insight from one organization to the next is possible more often than not.
In step 7, teams assess whether actionable opportunity exists in the context of operational complexity and readiness, with consideration to prior stories of success or failure. This is where team members prepare for the actions the organization needs to take to see improvements.
Wisdom would suggest that improvement teams find areas where there is an appetite for change and begin efforts in those areas. For example, if multiple improvement efforts are simultaneous, the team may find more success by identifying different parts of the organization that are receptive to piloting the changes.
In step 8, teams create and implement the improvement plan. This will require components of the work to be prioritized, where each component will be assigned accountability. If not already in place, the team will need to develop a robust communication structure and cadence. In the action step, the goal(s) should be explicitly stated and agreed on by all team members and executives who are supporting the initiative. There will often be competing perspectives on what the goal thresholds should be, which is why finding a balance between motivating, but achievable, goals will be essential.
After everyone has agreed on the goal to a reasonable degree, the team can now work to implement the change. If the goals have been set properly, meeting a goal would mean the improvement in outcomes from baseline has passed both a statistical and practical significance test. It would be best practice to revisit goals on an annual basis to recalibrate against system obstacles or opportunities.
Health systems can benefit greatly from following the analytics ascension model, but only if improvement teams follow each step. It can be tempting to skip steps or rush through a step in order to more quickly start implementation (step 8), but this risks misguided efforts and wasted resources.
Following the model hierarchy and giving each step the time it deserves creates a culture of data literacy and sets teams up for success in the often challenging field of outcomes improvement, delivering data-informed healthcare. It also empowers teams to achieve cultural alignment and illustrates how to approach data in the context of improvement projects. Rather than leaning on buzzwords like “data informed” or “data driven,” the Analytics Ascension Model gives team members the approach and vocabulary to take data from its raw state all the way to an action that results in meaningful patient outcome improvements.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.