How can health systems avoid just talking about improvement and instead achieve real progress in clinical quality performance? First, improvement teams need access to a robust data infrastructure that can provide a complete picture of performance. This analytic insight reveals process gaps and opportunity areas where the care team can target improvement efforts.
After selecting an opportunity area, care teams are ready to follow the three-step process to achieve meaningful clinical improvement:
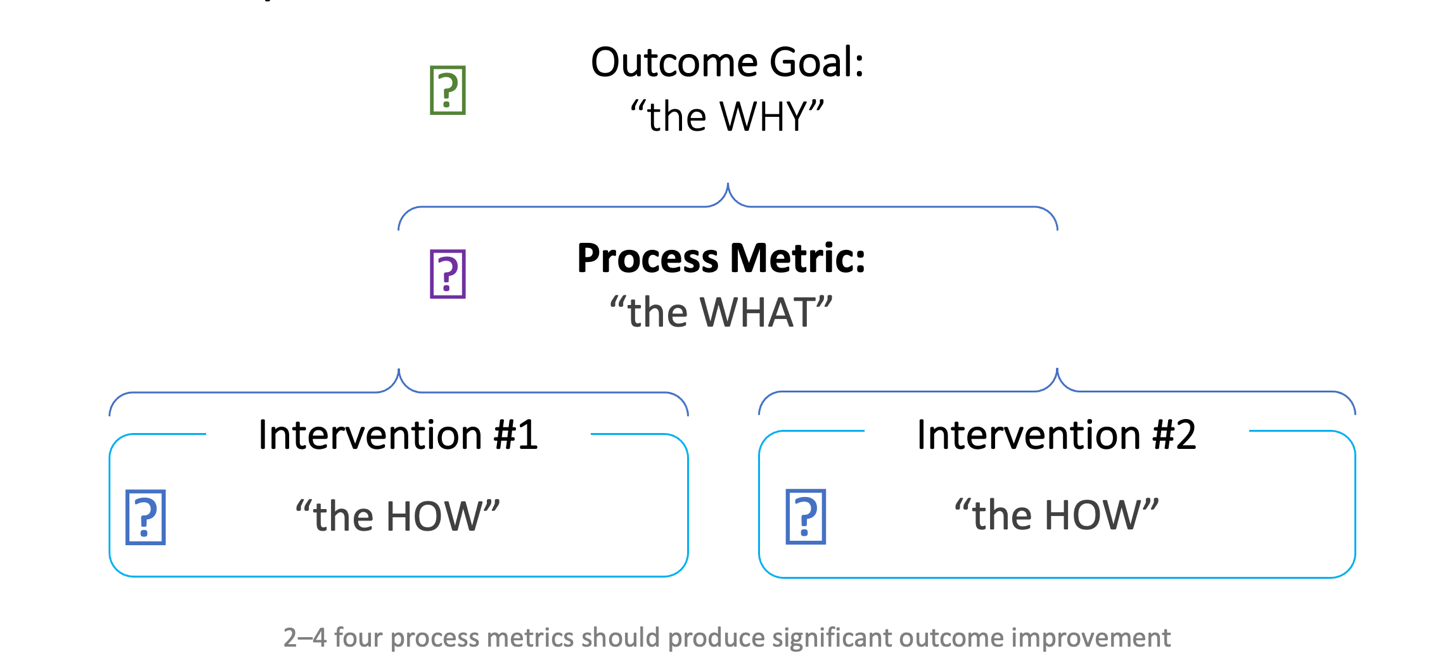
1. The “why”: Identify the outcome goal.
2. The “what”: Select a written, measurable, and time-sensitive process metric to evaluate the process.
3. The “how”: Identify the best interventions that will support the desired change in a process.
 Download
Download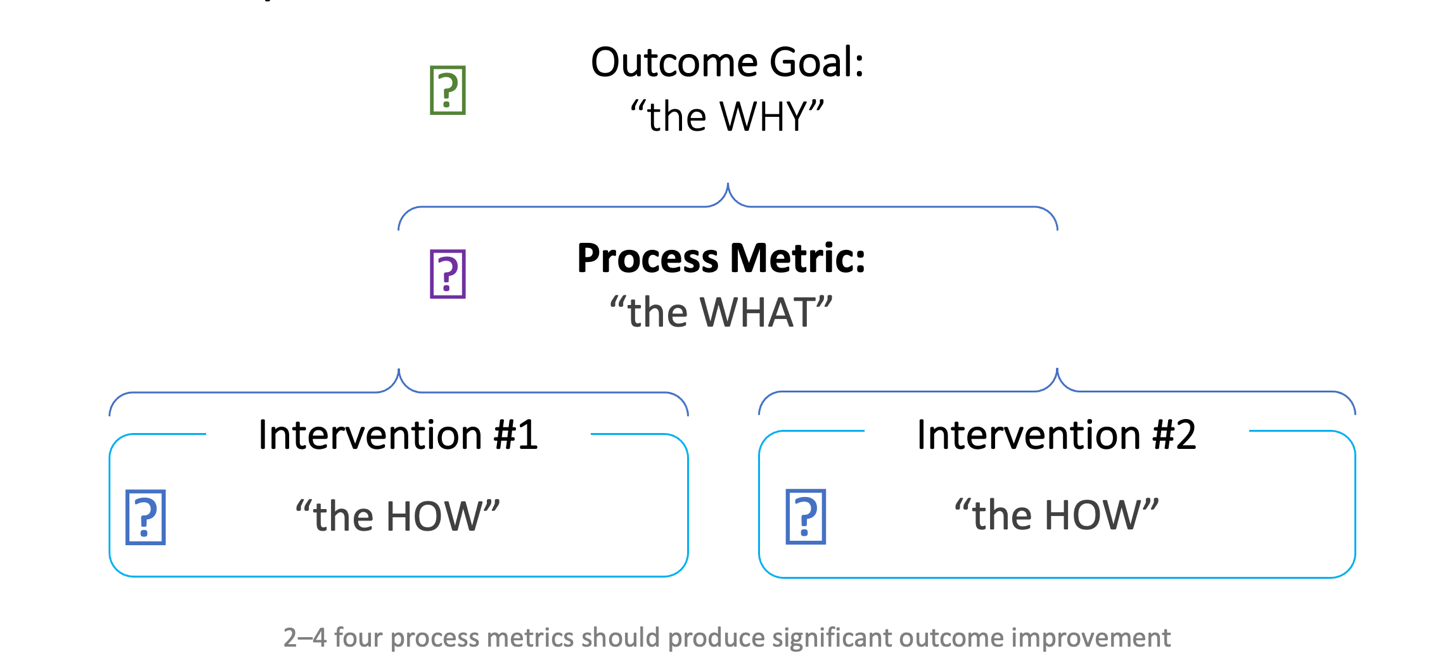
Health systems rely on clinical quality improvement projects to drive better patient care, but meaningful changes can only come from an improvement team’s deliberate action. This action is called an intervention and addresses a clinical quality improvement process metric and higher-level outcome goal.
Selecting efficient, effective interventions can be a challenge without knowing where to start. In response, improvement teams can identify a process metric (a standard measurement used to evaluate a process) as a working template for clinical quality improvement projects. The process metric is written, measurable, and time-sensitive and ensures the clinical quality improvement team is on track to achieve its outcome goal (Figure 1).
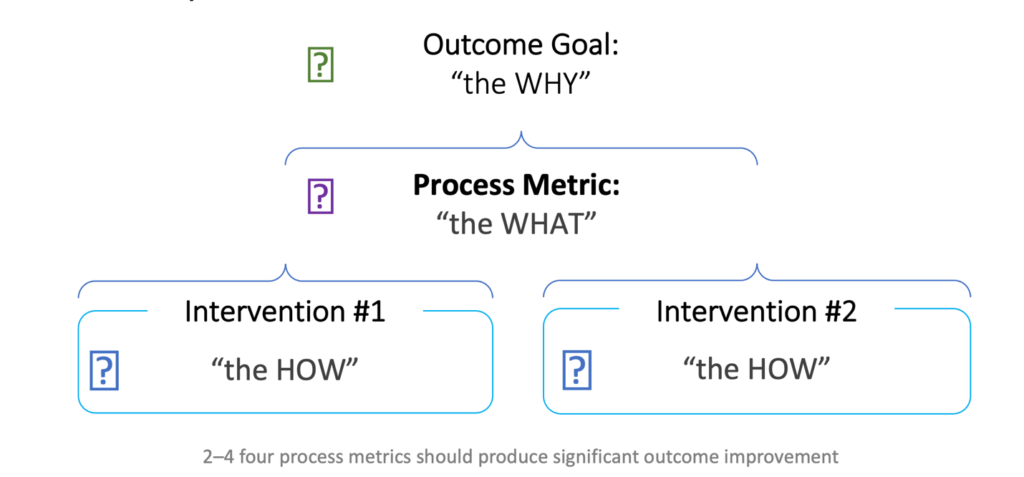
Figure 1: The outcome goal development process.
Once a workgroup identifies a process metric, it does process mapping to identify the right intervention to implement and officially starts the clinical quality improvement process. Intervention types include a process intervention or an outcome measurement intervention.
A process intervention focuses on an activity or aspect of a care-delivery process, while an outcome measurement focuses on results and measures the effectiveness of the change in the care process. Not all process interventions will have a direct outcome. However, by focusing on care processes, improvement teams can measure the outcome and identify areas with a direct impact on improvement.
Current practice, clinician ideas or input, and documented best-practice research in accordance with workflow analysis can all prompt proposals for interventions. Before selecting the intervention, the improvement team should identify appropriate datasets to measure each intervention’s success (e.g., reduction in HbA1C levels for an intervention targeting patients with Type 2 diabetes) and review the latest literature to ensure the team follows up-to-date best practices.
Health systems often target common outcome goals (reductions in mortality, length of stay, cost, or readmissions) as a good starting point for clinical improvement projects. For example, many health systems struggle to lower high readmission rates for patients with heart failure, resulting in expensive medical costs for the patient, health system, and payer.
Before starting any clinical improvement project, a healthcare organization needs a comprehensive data platform (e.g., the Health Catalyst® Data Operating System (DOS™)) that can aggregate data from multiple sources. Once the health system can access specific heart failure data, for example, the improvement team can identify areas for improvement and use that insight to create outcome goals and process metrics targeting these problem areas.
An example of an outcome goal for lowering high readmission rates for patients with heart failure could be: “To achieve and sustain a 30 percent reduction in the 30-day and a 15 percent reduction in the 90-day all-cause readmission rates for patients with heart failure in six months.” Associated process metrics would be to improve discharge bundle compliance from 45 to 70 percent within the next year or standardized diuresis protocol adherence from 55 to 75 percent in the next six months.
After the health system has agreed on the process metric, the care team can create interventions that support the metric. The health system’s clinical leaders can develop evidence-based, heart failure-specific best practice readmission bundle interventions, such as the following:
After the care teams decide on the best interventions (listed above), improvement teams can work with data experts to integrate intervention baselines and practices into the Heart Failure analytics accelerator, allowing clinicians and administrators to easily track and understand each intervention’s impact on readmissions. The analytic insight and the data visualization also allow teams to assess the interventions’ impact on costs and ;patient satisfaction.
Additionally, because the health system’s focus on reducing readmission rates could impact other areas, such as increased emergency department (ED) visits or decreased patient experience scores, the teams could add balance measures to track ED encounters, observation stays, length of stay, and patient satisfaction rates. After six months, the care team can compare heart failure readmission data and see if the interventions have led to significant clinical improvements (e.g., a 10 percent reduction in 30-day heart failure readmission).
The secret to selecting the right intervention for a clinical improvement goal and process metric is choosing something that offers gain (or improvement) and provides a means to sustain that gain. For example, by selecting a heart failure intervention, which includes timely follow-up appointments, patients gain medical surveillance and improved care. At the same time, the hospital is preventing readmissions by monitoring the patient soon after discharge, also reducing the financial penalties associated with readmissions.
Many clinical improvement teams use custom dashboards to display the key metrics they want to monitor to track the intervention they have selected (Figure 2).
Figure 2: A heart failure patient follow-up dashboard.
These dashboards help clinical teams easily recognize gains and sustain them. The dashboards also allow team members to monitor key metrics, such as the percentage of scheduled follow-up appointments and the relationship to readmission rates. By providing a current view of the team’s goal and progress toward that goal with an actual visualization, clinical teams avoid falling back into suboptimal healthcare practices.
For clinical quality improvement projects to work—and keep working—team members must create an environment that fosters success. First, improvement teams must carefully choose the best process metric to impact the higher-level outcome goal for the project and associated intervention. Then the team can use data and data visualization tools to constantly monitor and measure progress to ensure the interventions are achieving the desired results. With constant monitoring, improvement teams can recognize undesirable results immediately, reducing wasted time and resources. By following this clinical improvement roadmap, clinicians enhance care processes so that patients receive the best care available.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download this presentation highlighting the key main points.