As health systems continue to adapt to the pandemic healthcare landscape, certain challenges remain—including generating revenue on thin operating margins. Poor charge capture is a common reason behind lost revenue that healthcare leaders often fail to address. Because charge capture is the process of getting paid for services rendered at a hospital, poor charge capture processes mean the hospital does not get paid in full for a service, resulting in lost revenue that is typically unrecoverable.
Health systems can avoid financial leakage and increase profits by focusing on five problem areas within charge capture practice:
1. Emergency services.
2. Operating room services.
3. Pharmacy services.
4. Supply chain and devices.
5. CDM mapping.
 Download
Download
This article is based on a webinar by William Malm, Senior Vice President of Client Strategy at Vitalware®, titled, “Charge Capture-Hotspots in Your Facility.”
The Healthcare Financial Management Association reports that up to 1 percent of a health system’s net charges comes from lost charge capture opportunities, a significant amount of money for any healthcare organization. Charge capture is the process of getting paid for the services a health system provides and is based on a health system’s master list of all billable services and associated costs, also known as the chargemaster or charge description manager (CDM).
Unfortunately, due to its complex nature, charge capture leaves much room for error. Typically, the EHR or a team member will assign a code to a specific service (e.g., a primary care visit) and then submit that as a claim for reimbursement to payers, insurance companies, or CMS. However, due to commonplace coding errors in healthcare, many claims are inaccurate, delay reimbursements, or decrease payment, negatively impacting a health system’s revenue stream.
Charge capture, or the process of getting paid, is an essential function of business operations, especially in healthcare when hospitals survive on thin margins—now even thinner because of COVID-19. Therefore, health systems should invest in improving charge capture processes that decrease leakage and lead to a bigger bottom line.
With every department at a hospital directly affecting a health system’s financial state, organizations struggle to know where the lost 1 percent of revenue goes. However, there are five hot spots—areas susceptible to poor charge capture processes—that health systems can target to improve charge capture and decrease charge loss:
Emergency services (ES) are a loss leader in charge capture due to high volume. Patients are always the priority, meaning that providers often forget documentation and coding or leave it to the last minute, especially on a busy emergency department (ED) day.
Poor documentation also occurs in the ED when providers fail to adequately document procedures. For example, a nurse might document a laceration repair as “suture by physician” in the EHR when the charge capture actually requires more information to qualify for reimbursement, such as the location, depth, and size of the laceration. To improve this process, the charge capture team could create a laceration template in the EHR so that a nurse includes the correct information when he documents a laceration. This not only eases the burden on providers by eliminating any guesswork about sufficient laceration documentation but ensures adequate documentation for reimbursements.
Other frequent causes of lost charges in the ED include:
Similar to ES, poor documentation can become even more complicated with the combination of hard- and soft-coded items. For example, an item is hard coded when the CDM automatically assigns a code to a service, and an item is soft-coded when a team member manually assigns a code to a service. Unclear documentation processes (e.g., Is the item hard- or soft-coded and if soft-coded, who is responsible for assigning a code?) can lead to confusion in the operating room (OR).
To decrease confusion and improve documentation in these areas, charge capture software, such as Vitalware® VitalIntegrity™, allows teams to easily analyze charge capture within any department, such as the OR, to identify missed charges and over or under charges that have downstream revenue implications.
Other areas of the OR that charge capture teams can improve include the following:
The pharmacy is notoriously a health system’s greatest cost center and one of the biggest areas in which charge capture improvement can increase revenue. The pharmacy has unique charge capture challenges because of its own coding convention, the National Drug Code (NDC), a CDM that is often not updated with new drugs on the market or revised codes, and its own revenue cycle that must sync with the larger health system’s revenue cycle. These distinct revenue cycles cause many charge capture problems because oftentimes the health system’s revenue cycle team doesn’t fully understand how the pharmacy revenue cycle works.
It is best practice for leaders to regularly review the pharmacy’s purchase history and what they submit to the charge master. However, most of the errors in pharmacy occur during the conversion from dispensing units to billing units (the red triangle in Figure 1, below). Many facilities use a category system where all NDC with the same HCPCS are in the same category. These categories then require a specific equation to convert the NDC dispensing units to the specific billing units. This conversion factor is a common reason for failed pharmacy charge capture.
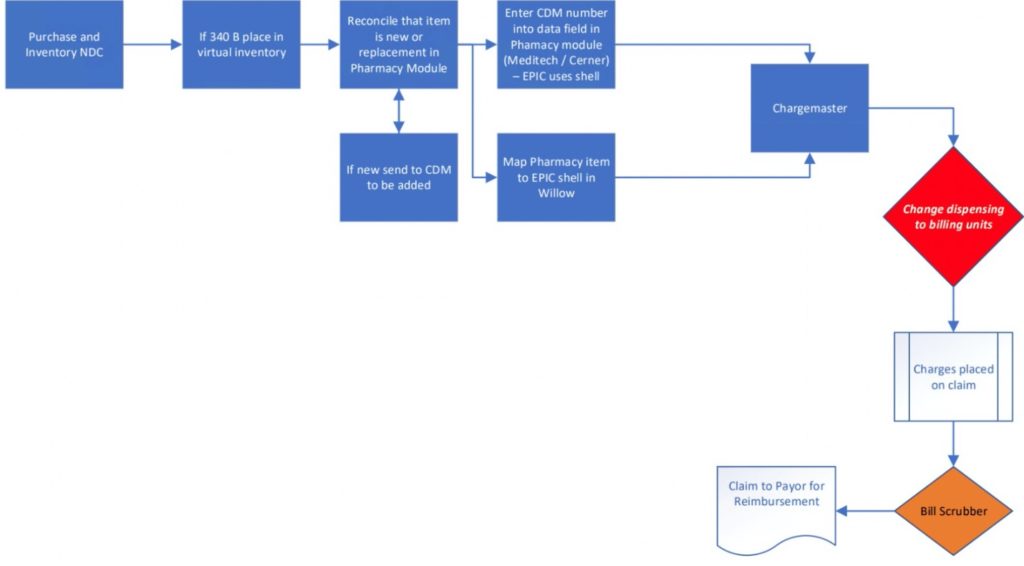
Figure 1: The pharmacy revenue cycle.
The key to preventing pharmacy charge capture errors is to ensure that the NDC is always up to date with the latest HCPCS codes. Another way to avoid pharmacy charge capture errors is to leverage pharmacy charge capture software (e.g., Vitalware Pharmacy Analysis) that has a low- and high-dosage range to capture billing units that are out of normal ranges for the average adult.
Supply chain and device charge capture is difficult because it relies on charging for the correct device with the correct HCPCS code. Team members must confirm they assign the correct code to the device, so they charge for the correct device. While this sounds simple, the manufacturer and model determine the device charge, and many manufacturers will provide a “suggested HCPCS” code. While the suggested code might be correct, team members should treat these as coding guidelines and always confirm the code.
Other examples where supply chain and device charge capture fall short include insufficient current procedural terminology (CPT) coding for devices and failing to manually document charges in the OR. The OR is the most likely area where charge capture will fail because most devices are not on a preference card, therefore, providers must manually enter the codes, leaving room for delayed submission and human error.
Effective CDM mapping includes testing that can drive smoother charge capture processes, leading to increased savings and new financial opportunities. For example, documentation-driven charging begins in the clinical module. After documentation, the charge goes to the CDM to assign the HCPCS/CPT code and patient charge. The transition from the clinical system to the CDM occurs because the two systems are mapped. However, the mapping system is prone to problems if team members seldom review or test the maps with a new charge to ensure charges are generated correctly.
The other critical piece of CDM mapping is maintenance. Most facilities use an automated CDM software maintenance system. However, the CDM analyst usually sends the hospital department (e.g., cardiology) the report of changes, adds, deletions, and audit findings, showing that most departments lack procedural coding skill. The analyst should meet with the department leaders once a year and ensure they have a charge for all services rendered. Other areas to improve maintenance include working with departments to identify and remove zero-volume usage items that are more than 18 months past their last use.
Effective charge capture is a health system operational essential, as it generates income from services or procedures. Instead of letting charge capture fall behind other priorities, health systems should prioritize understanding the nuances of charge capture best practices to identify corrective actions and decrease charge capture leakage.
Focusing on the five hot spots—ES, OR, pharmacy, supply chain and devices, and CDM mapping—allows health systems to target loss leaders and decrease common charge capture leakage (the 1 percent of lost revenue). Implementing charge capture best practices can directly increase a health system’s earnings, putting the organization’s financial state back in the hands of hospital leaders.
Would you like to learn more about this topic? Here are some articles we suggest:
PowerPoint Slides
Would you like to use or share these concepts? Download the presentation highlighting the key main points.