While healthcare waits for the expanded data interoperability that FHIR promises, the industry needs an immediate solution for accessing and using disparate data from across the continuum of care.
With FHIR potentially several years away, continuity of care documents (CCDs) are the best option for acquiring the ambulatory clinical care data health systems need to close quality gaps today.
Because organizations that rely only on claims data to drive quality improvement risk missing out on more that 80 percent of patient information, CCDs are the current must-have answer to interoperability for successful quality improvement.

ACOs, clinically integrated networks (CINs), and those seeking to increase exposure to value-based payment (VBP) models and take on risk need more data interoperability to achieve desired outcomes. Organizations that continue to rely solely on claims data to drive quality improvement may lack more than 80 percent of available critical patient information.
This article considers health data’s current interoperability limitations and why using only claims and acute clinical data can’t close quality gaps. It poses using ambulatory clinical data in the form of continuity of care documents (CCDs) as today’s best interoperability solution.
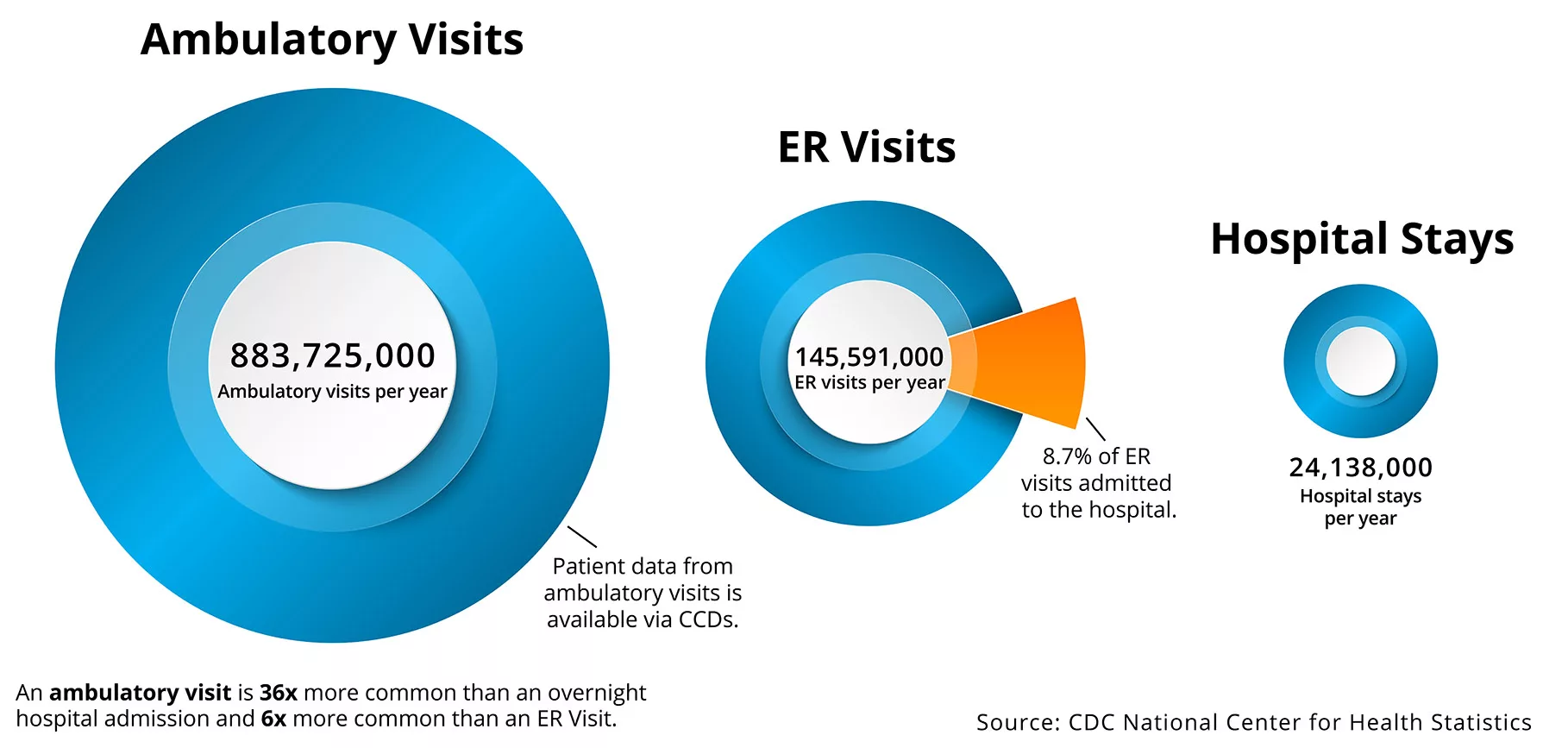
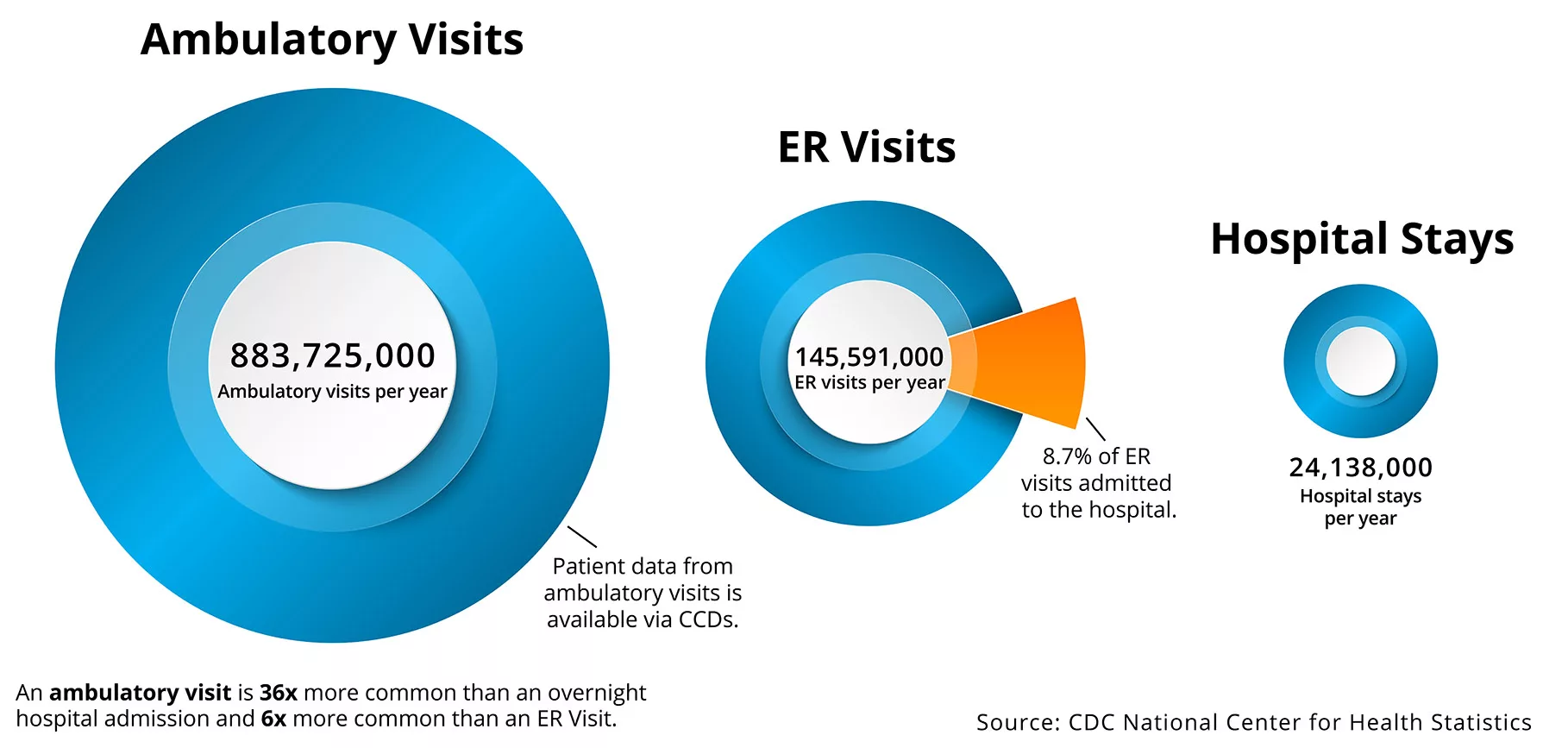
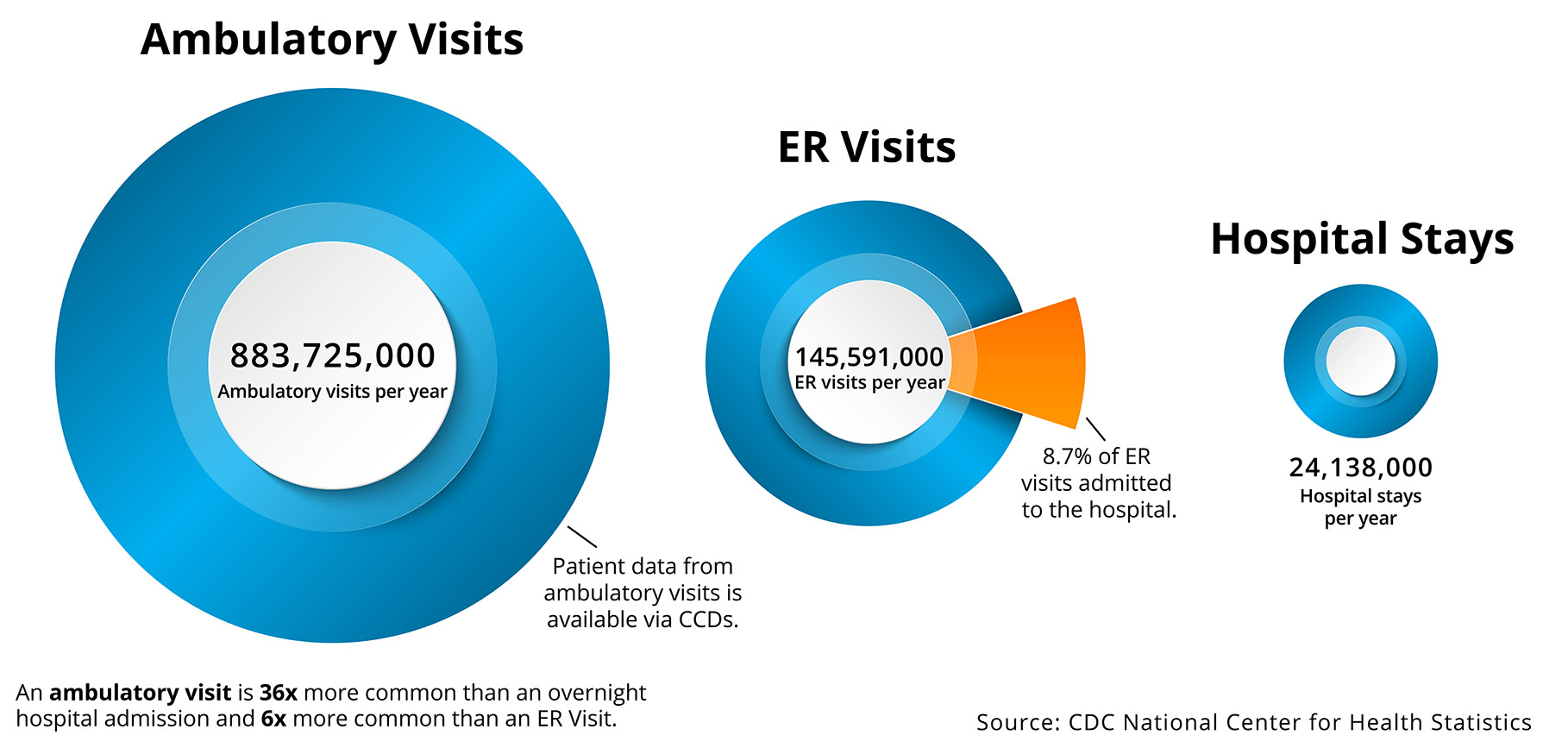
Because healthcare consumers today are much more likely to receive care in an ambulatory setting versus the acute care setting (which claims data represents), organizations must have the interoperability to access ambulatory data.
Data interoperability drives insights behind and takes steps towards significant quality improvements, including the following:
With a variety of healthcare delivery settings, it’s important to understand some of the key limitations and differences, including identifying where most of the valuable clinical data resides (Figure 1).
Health systems have used claims data to inform quality measurement and calculate required metrics, but as the industry evolves further towards population health and value-based care (VBC), organizations need more timely, comprehensive, and higher quality data. CCDs, which contain patient-centric clinical data, are not an ideal solution, but as the industry finalizes interoperability standards and removes the hurdles to sharing data, CCDs are today’s most capable and broadly adopted healthcare clinical data source.
Organizations that overlook CCDs and wait for a more comprehensive data solution (i.e., FHIR) will miss out on years of improvement opportunities and fall behind industry benchmarks, as they’ll rely on delayed or incomplete data:
The 21st Century Cures Act sets the stage for FHIR, however, it is several years away, and many EMRs do not currently offer an effective way to ETL (extract, transform, and load) data. FHIR is likely the preferred method of the future, but its standards were out for commentary until May 2019 and not expected for release until the fall of 2019. The release date for the latest and fourth version of FHIR also has one- to two-year grace period, meaning it may not happen until 2021 or 2022. While healthcare waits for FHIR, CCDs may be the best available solution to interoperability.
By providing a standard way to document and transmit clinical data, CCDs provide interoperability between multiple acute and ambulatory providers, pairing retrospective analytics (e.g., claims) and robust near real-time clinical analytics. Interoperability is increasingly critical as QMs require certain data that often only resides in ambulatory clinical records:
The following guidelines help healthcare organizations best leverage CCD interoperability for QMs:
An organizational data quality program drives success for quality measures and alignment to other strategic objectives:
The following strategies support an effective approach for QMs:
Interoperability to capture ambulatory clinical data from CCDs is an essential part of improving outcomes, but healthcare still involves a diverse set of public and private data collection systems (e.g., CCDs, surveys, enrollment, and claims data). Driving better outcomes starts with blending more data together, particularly two data types—near real-time CCDs and retrospective claims.
To meet healthcare’s modern goals, organizations must leverage a fully interoperable analytics platform to acquire near real-time clinical data and harmonize it with a range of data types from a variety of sources. An optimal modern healthcare data approach includes use of a cloud-based analytics platform, such as the Health Catalyst® Data Operating System (DOS™).
Interoperable CCD clinical data and claims data can support an effective continuous quality improvement process in healthcare, as the blended data more effectively measures quality, creates new ways of evaluating impact of interventions (near real-time and retrospective), and evaluates applied interventions with a dashboard that incorporates the best of real-time clinical and claims data. The top benefits of interoperable data can include, but are not limited to, the following:
Organizations that wait for FHIR, and do not find an interim interoperability solution for acquiring cross-community CCDs, risk missing out on opportunities to enhance their overall data asset. The ability to provide different methods (e.g., the Health Catalyst® Interoperability Suite) to acquire cross-community CCDs and clinical data is critical to support care delivery (operationally and clinically), boost confidence around population health, and enable more accurate performance measurement.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.