Hospital command center leaders have never had to run an incident response on the scale of the COVID-19 pandemic. Whereas a typical emergency event (e.g., flooding, earthquakes, multivehicle collisions, or shootings) causes rapid patient influx with an identifiable starting and stopping point, the novel coronavirus has an ongoing, inestimable impact. The extensive duration, combined with high transmission risks and a massive scope of impact, demand that health systems prepare for complex facility, equipment, and staffing needs.
Their best strategy is to leverage data-driven tools to scale their existing emergency response plans for COVID-19’s unprecedented proportions.
 Download
Download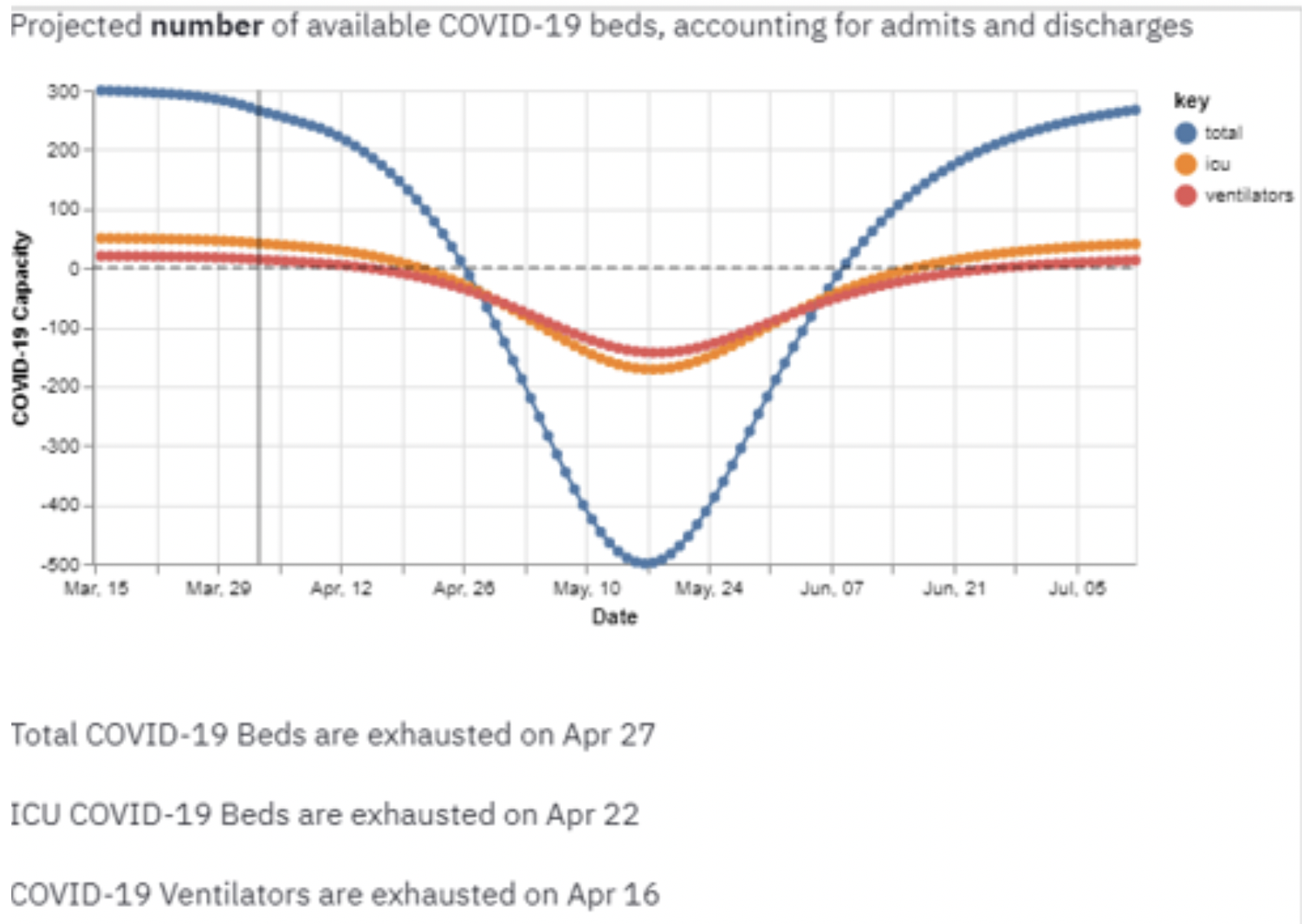
With typical hospital command center planning, organizations and teams prepare for short- and mid-term emergency responses. Major weather-related events, such as flooding, earthquakes or hurricanes, or even multivehicle collisions and shootings all have the potential to cause rapid patient influx and require significant hospital response. But, events like these usually have an identifiable starting and stopping point, mostly requiring only basic data and analytics for impact forecasting. The COVID-19 pandemic, however, is driving the need for a command center strategy to handle a mid- or long-term event with no known endpoint, calling for unique planning and advanced data and analytics support.
The long duration, high transmission risks, and massive scope of impact of the novel coronavirus are driving more complex facility, equipment, and staffing needs than U.S. hospitals have ever addressed. With no roadmap or recent events on which to base a pandemic-ready command center strategy, health systems need to leverage data-driven tools to scale their existing emergency response plans to COVID-19 crisis proportions.
Patient care, disease control, and, eventually, recovery will rest on health systems’ ability to address a bigger, more fluid situation than leaders and team members have trained in or experienced. Scaling the response will necessarily focus on the areas of highest impact: clinical capacity, equipment, and staffing and rely on comprehensive, accurate, and accessible data.
In the shift from short- to mid-/long-term emergency response, the service orientation and data projection needs change over time to forecasting extended capacity implications, equipment utilization, and staffing needs. The command center focus transitions from the immediate action of “who’s here now, what do we expect over the next few days, and how are we going to staff and provide equipment and supplies?” to a prolonged and more comprehensive look at the same essential elements.
Due to the sustained duration of a mid- to long-term event, the emergency response requires more complex management than its short-term counterpart. Extended demands and a steady flow of critically ill patients require the command center to move to a virtual platform and demand complex analytics. Care shifts from urgent/emergent to more chronic and more extended-term needs—for example, moving the focus from trauma surgery and Emergency Medical Services-related rescue care to ventilated patients and ICU-related acuity.
Regardless of scale, the right information and data is operational currency for hospital command centers. Emergency planners use projections and sophisticated algorithms to continuously project what’s coming next, how to respond best, and how to prioritize actions and resources. Because inaccurate information leads to incorrect estimations, a command center response, and the eventual outcome, is only as good as the data behind it.
Emergency response leaders can plan to scale their typical command centers to meet pandemic needs by leveraging tools that derive insight from predictive models (e.g., disease progression, services and supply utilization, and identification of at-risk populations). These insights assess the impact and help the organization plan for longer-terms needs related to capacity, equipment, and staffing.
Reliable data and analytics in the following key areas support command center scaling for COVID-19 needs:
COVID-19 has created intense pressures on hospital capacity, and the overflow has pushed patients to hallways, tents, hospital ships, convention centers, and more locations beyond the typical care setting. In the meantime, health systems must still register all patients, and track distributed patients to properly document patient care, monitor the disease as well as recover costs or lost revenue (e.g., to obtain federal recovery funding).
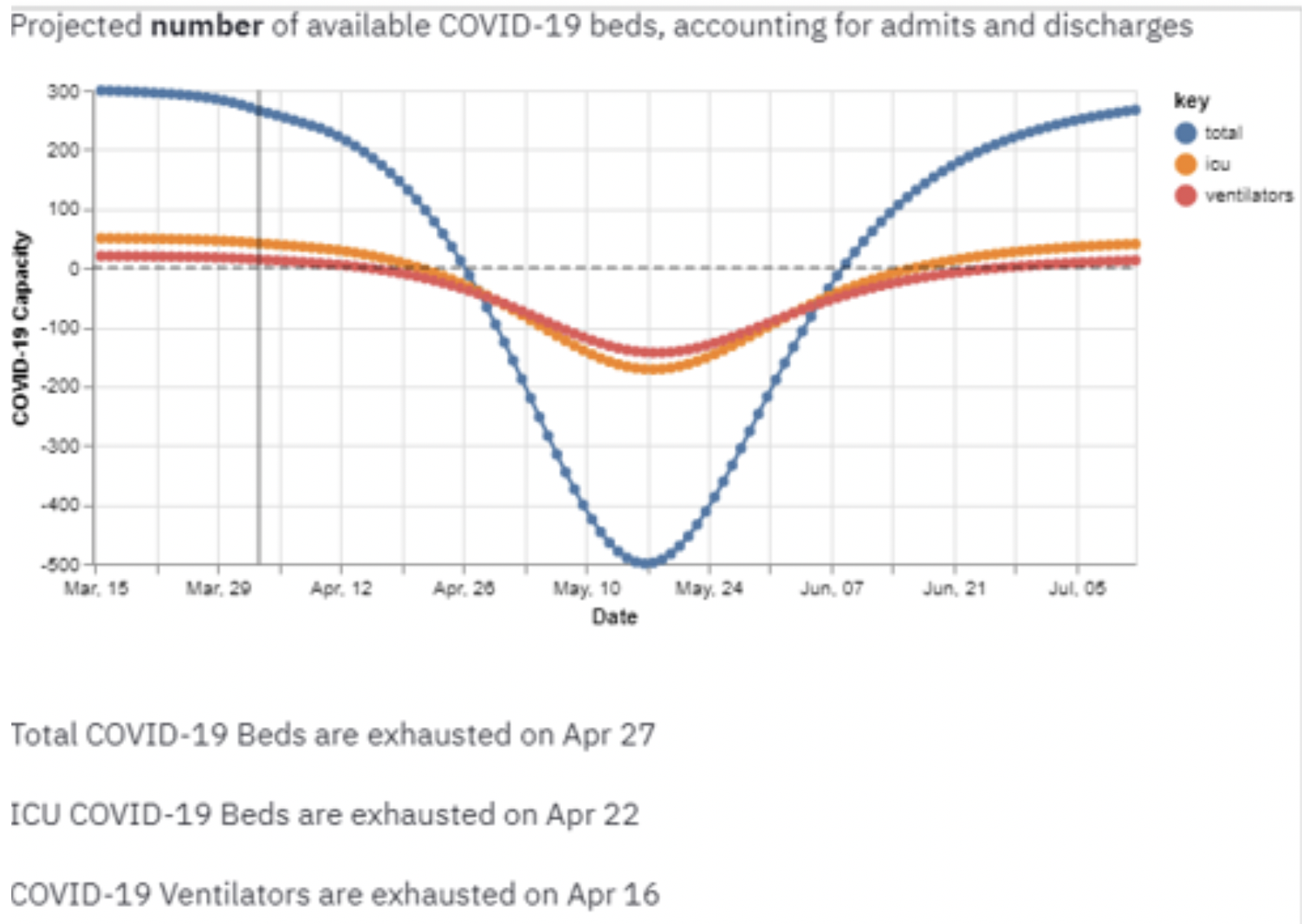
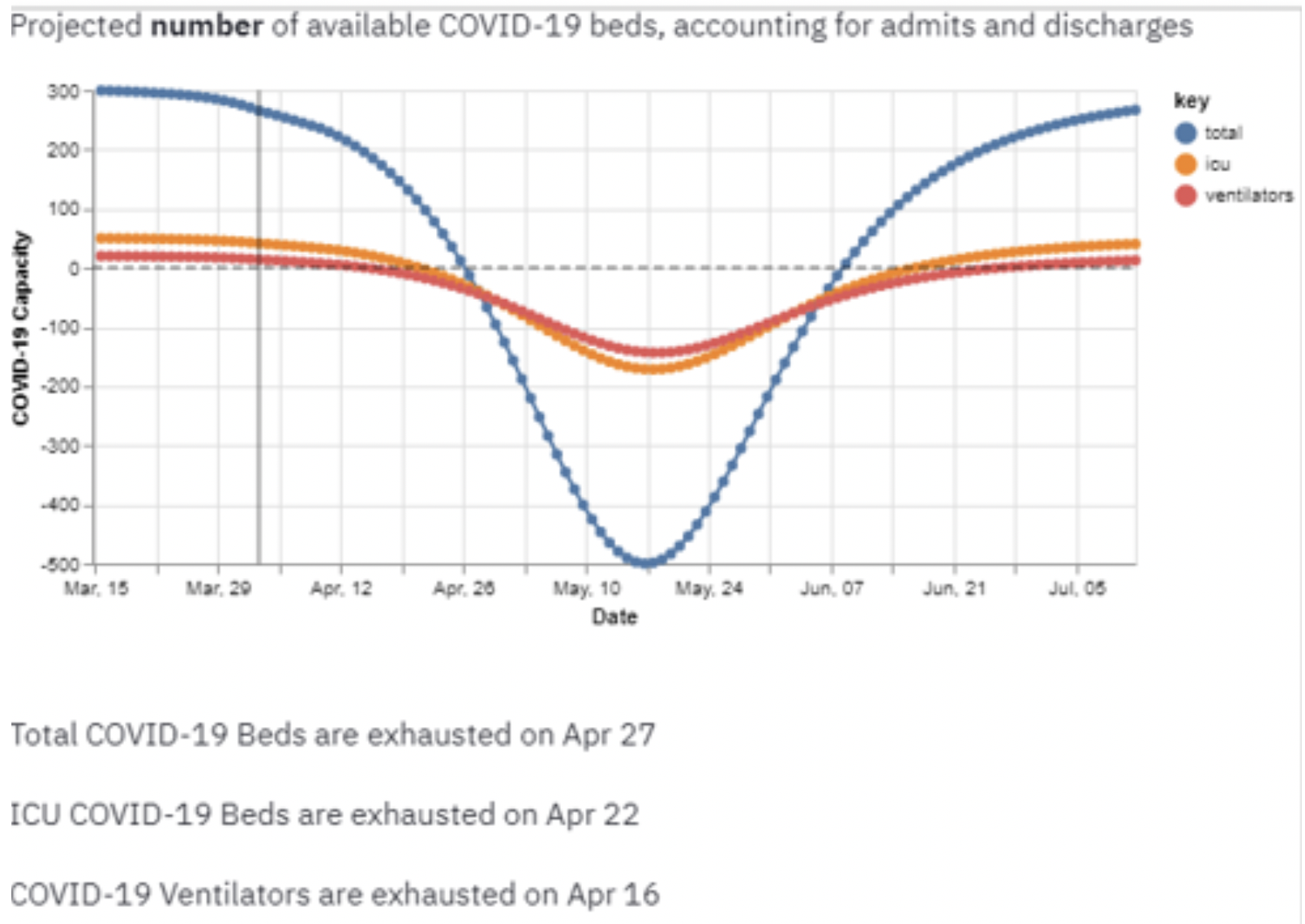
An epidemiologically-driven capacity planning tool (Figure 1), such as the Health Catalyst® Capacity Planning Tool, part of the organization’s COVID-19 response, forecasts community-level pandemic-related demand in the context of a system’s capacity, supplies, and staffing—and the subsequent impact of infection rates on care delivery capacity. Command center leaders can use this insight to set expectations and inform an overflow mitigation strategy.
With the high contagion rates of COVID-19, understanding contact history among patients and hospital staff (i.e., who may have risked exposure to the virus) is a vital component of a response strategy, informing testing, quarantine efforts, and decontamination activities. Health systems can use a monitoring tool (e.g., the Health Catalyst® Patient and Staff Contact Tracker) to access reports that track the location and interactions of patients and staff with confirmed or suspected COVID-19.
An effective pandemic response requires timely, accurate data to generate quick insights for critical decision making. The Health Catalyst® Self-Service Analytics Solution™ for COVID-19 features quickly accessible prebuilt, curated, reusable data content (DOS™ Marts), including continually updated COVID-19 codes and value sets. Command center teams can add new data to their source systems via the Instant Data Entry Application (IDEA). They can then leverage the Population Builder™: Stratification Module to build COVID-19 disease registries swiftly and create, visualize, share, and monitor COVID-19 dashboards using the Leading Wisely® application.
Emergency response to the novel coronavirus makes the complete data story for the disease more significant than ever. By monitoring COVID-19 infections beginning at the initial point of contact within the healthcare organization (e.g., ED registration), providers can identify and flag unusual symptom/clinical test patterns that could represent illness. A public health application that leverages a comprehensive analytics platform can perform enhanced biosurveillance monitoring and analytics, enabling a quick and effective public health response. With a tool such as the Health Catalyst® Patient Safety Monitor™ Application: Public Health, hospital epidemiologists and infection control personnel can perform local, rapid, and preliminary assessments of patient-level clinical data.
A national COVID-19 registry enables a deep understanding of COVID-19 treatments and outcomes, making a critical part of a long-term emergency response. The Health Catalyst® Touchstone™ COVID-19 National Data Sets and Registry (Figure 2), for example, consists of three patient types: high-risk patients; patients suspected of being infected, but not confirmed; confirmed COVID-19 patients. Organizations can use the registry to derive insights about surveillance, testing, capacity planning, and treatment response to deepen and accelerate their understanding of the outbreak. With registry-driven insights, health systems can inform care pathways for patient management and outcomes improvement during recovery, as well as identify indicators to inform clinical trial design, feasibility, and recruitment.

Analytics accelerators, tools that health systems can implement and configure quickly, help organizations meet the clinical, operational, and financial challenges of COVID-19. By providing decision-making insights, the following types of accelerators help organizations prepare for and respond to, as well as recover from, COVID-19:
Health systems’ best emergency response to the novel coronavirus pandemic is to take what they know in the form of their customary command centers and scale them to unprecedented levels. Organizations can meet these new volume and impact challenges by fully leveraging data and expanding their insight and analytic competencies. With advanced analytics-driven COVID-19 response tools and informed decision making, health systems can transform their emergency frameworks for the outsized proportions and agility a pandemic requires.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.
Click Here to Download the Slides
https://www.slideshare.net/slideshow/embed_code/key/eLsAfm0p6sNNlV