Customer journey analytics uses machine learning and big data to track and analyze when and through what channels customers interact with an organization, with an aim to influence behavior (e.g., buying behaviors among retail customers). Similarly, healthcare organizations want to influence health-related behaviors, such a taking medication as prescribed and not smoking, to improve outcomes and lower the cost of care. In a partnership with an analytics services provider, a payer organization is leveraging customer journey analytics among healthcare consumers to identify the best opportunities and channels for patient outreach. With this analytics-driven engagement strategy, the payer has found an opportunity to significantly improve patient engagement—a predicted overall increase from 18 percent to 31 percent.
 Download
Download

This report is based on a 2018 Healthcare Analytics Summit presentation given by Christer A. Johnson, Principal, EY Analytics, and Alexander (Alex) Marano, Customer Analytics Lead, Cigna Information Management and Analytics, entitled, “Using Machine Learning and Big Data to Drive Patient Engagement and Better Health Outcomes.”
There are moments in every patient journey in which a well-informed, well-timed intervention (e.g., phone call, personal visit, etc.) can effectively engage patients and positively influence their health-related behavior. Random engagement, however, is far less effective than analytics-driven strategic engagement. To know when to reach out to and which patients to focus on, payers need an approach that leverages machine learning and big data.
Other industries have used analytics-driven engagement strategies, or customer journey analytics, to analyze real-time data on customer interactions, demographics, and lifestyle events and use these insights to influence customer behavior (e.g., buying behaviors in the retail sector). The healthcare industry is now working to leverage a similar approach to engage effectively with healthcare consumers to help them avoid risky health behaviors in favor of behaviors that improve their health and lower healthcare costs. This report describes a collaboration between a global analytics services provider and a large payer organization to leverage customer journey analytics among healthcare consumers.
Patient engagement solutions support outcomes improvement and cost reduction by targeting behaviors that have negative health consequences but are largely avoidable. These behaviors have a significant impact on patients with chronic and multiple health conditions, who are among the costliest populations.
Considering the following examples of unacceptable high rates of avoidable risky behaviors, improving patient engagement must become an industry priority:
Addressing the above avoidable health concerns above and their like presents a sizeable healthcare improvement opportunity. But to impact these statistics and the patients who comprise them, health services providers must understand behavioral patterns and factors most linked to engagement.
Customer journey analytics follows patient behavior to identify patterns most likely associated with engagement. Analysis may show behaviors and characteristics linked with likelihood to engage and key times to reach out to those patients. For example, the period following a specialist visit can be an engagement opportunity as patients tend to seek information (e.g., internet searches) at this time. If a case manager reaches out to the patient after the specialist appointment, she may have the answers the patient is looking for.
To leverage journey analytics to improve patient engagement, payers create the journey data, follow a framework for and execute the four phases of journey analytics, and operationalize the analytics.
Patient journey data creation (Figure 1) starts with a reference library that holds events, population criteria, outcomes, steps, attributes, and respective SQL logic. From that library come the patient attributes, time-sequenced journey, and journey step attributes. These datasets allow for ongoing and future applications:

The framework for patient journey analysis (Figure 2) asks questions about the patient journey in three key categories:
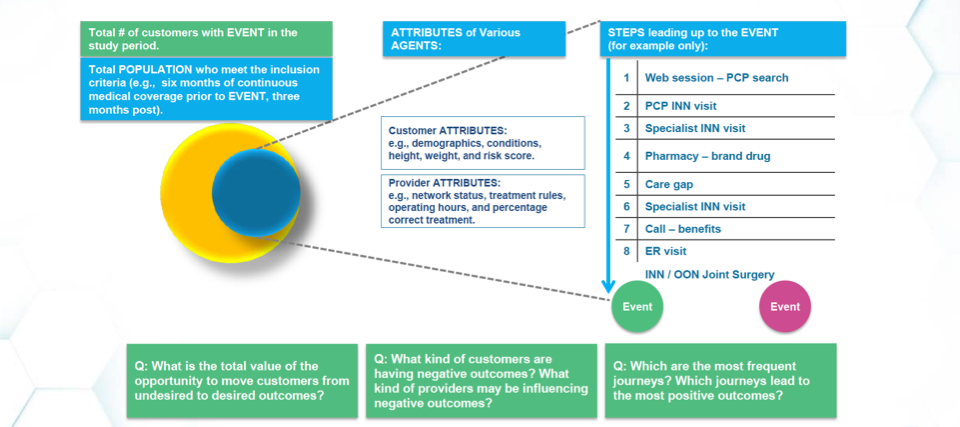
The framework also considers patient attributes (e.g., demographics, conditions, height, weight, and risk score) and provider attributes (e.g., network status, treatment rules, operating hours, and percentage correct treatment) and patterns (“steps”) most associated with engagement or lack of engagement (“event”). Steps may include internet searches, in-network primary care physician visits, in-network specialist visits, care gaps, ED visits, and more. These insights can help payers improve the timing, channel, and content they use to engage members with chronic and complex conditions in coaching that lowers medical costs and improves healthcare outcomes.
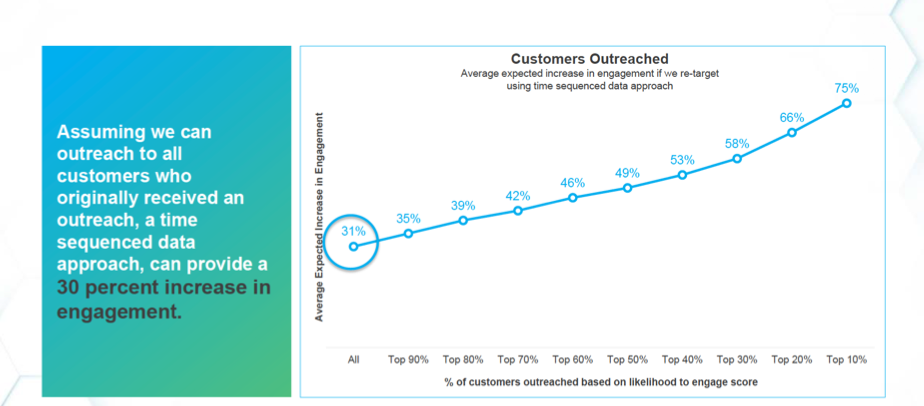
Journey analytics also helps payers identify the most impactable candidates for engagement using likelihood-to-engage score leverages. When the payer mentioned in this report compared using the likelihood-to-engage score with a traditional approach to outreach, predicted overall engagement increased from 18 percent to 31 percent.
Payers have previously based engagement strategies on claims data. As a layered approach to data, a time-sequenced customer journey data lake (Figure 3), combines claims and EMR data, negative events, physical and verbal signals, and digital signals. Payers can apply data to the journey to find moments when interventions will increase the probability that a patient will choose a better path (e.g., keeping follow-up appointments or taking medications as prescribed). These insights identify paths that help create alerts for good times to take action to improve outcomes and reduce cost. Actions include the following:

Patient journey analysis occurs in four phases. Each phase yields detailed journey data for patients identified for case management, a list of the most important journey steps by case management category, and potential engagement and engagement lift by case management category (e.g., oncology or OBGYN):
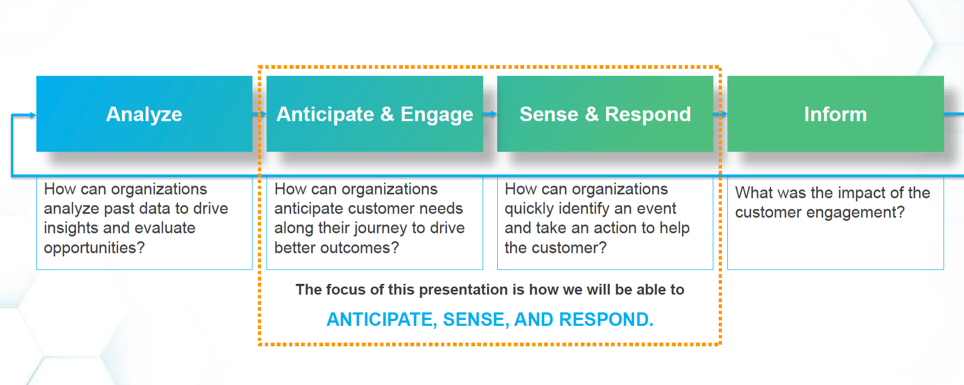
To be effective, payers must operationalize customer journey analytics. The key differentiators between basic analytics and operationalized analytics is that basic analytics only analyzes and reports (informs), whereas operationalized analytics, anticipates, engages, senses, and responds (the middle orange box in Figure 5). With the added capabilities of operationalized analytics, payers can better sense opportunity, engage in real time, and personalize these interventions over time.
Operationalized journey analytics have significant benefits over basic analytics:
Healthcare organizations can’t help patients if they can’t engage them effectively, and in an increasingly complex health landscape, better patient outreach is an imperative. Engagement improves significantly with an analytics-driven strategy that identifies whom to engage, when, and how. With patient journey analytics, payers and other healthcare organizations can influence better health behaviors to improve outcomes, customer satisfaction, and lower healthcare costs.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.