While many industries are leveraging digital transformation to accelerate their productivity and quality, healthcare ranks among the least digitized sectors. Healthcare data is largely incomplete when it comes to fully representing a patient’s health and doesn’t adequately support diagnoses and treatment, risk prediction, and long-term health care plans. But even with the obvious urgency for increased healthcare digitization, the industry must raise this trajectory with sensitivity to the impacts on clinicians and patients. The right digital strategy will not only aim for more comprehensive information on patient health, but also leverage data to empower and engage the people involved.
Health systems can follow five guidelines to digitize in a sustainable, impactful way:
1. Achieve and maintain clinician and patient engagement.
2. Adopt a modern commercial digital platform.
3. Digitize the assets (the patients) and the processes.
4. Understand the importance of data to drive AI insights.
5. Prioritize data volume.
 Download
Download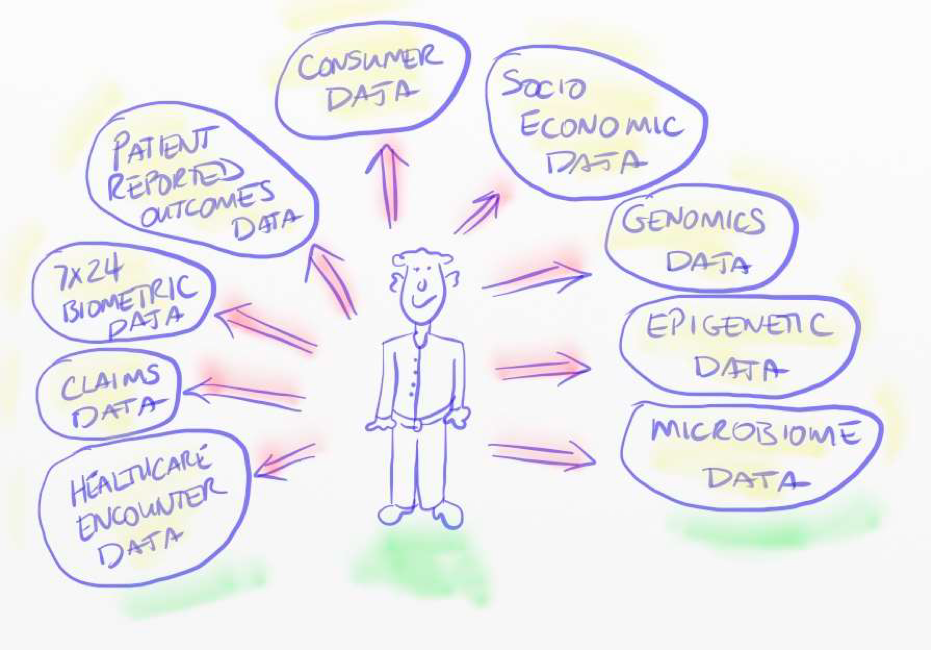
This report is based on a Dale Sander’s webinar, “Raising the Digital Trajectory of Healthcare,” presented August 15, 2018.
With ever-evolving technology and analytics capabilities, healthcare could be on the brink of a data-driven transformation. However, while many other industries are capturing the vast potential of artificial intelligence (AI) to revolutionize their work, healthcare hasn’t yet reached the level of digitization to allow it to leverage these next-generation tools and capabilities. To capitalize on the opportunities of this advanced analytics era, healthcare must raise its digital trajectory.
Global management consulting firm McKinsey ranks industries based on their Digital Quotient (DQ), which it derives from a cross product of three areas: data assets, data skills, data utilization. The healthcare sector’s DQ comes in at below almost all other industries, leaving a lot of room increase digitization. There’s a specific way, however, in which healthcare must approach digitization that’s mindful of the human side of healthcare decision making while prioritizing data and the technical infrastructure for a true data- analytics-driven industry.
The right way to increase digitization will also increase the sense of humanity around healthcare to better address patient and clinician needs. Healthcare may have largely ignored the human, or softer side, of a digital strategy. Clinicians today feel the brunt of a less human-centered digital environment and suffer from the emotional burdens of burnout, including the highest rate of suicide of any profession. Healthcare’s current data-driven strategy is ineffective, and even harmful to the industry it’s meant to serve. It’s nonhuman-centered approach is robbing clinicians of their sense of mastery, autonomy, and purpose and holding them to performance measures that don’t adequately represent the quality of their work.
A 2018 article documented physician burnout, attributing much of it to the EHR era and the poor way the U.S. healthcare system has implemented a data-driven strategy. In a survey, the Medical Group Management Association (MGMA) identified that 84 percent of physicians are now participating in the Merit-based Incentive Payment System (MIPS). Of them, 82 percent consider the Medicare Access and CHIP Reauthorization Act (MACRA) Quality Payment Program very or extremely burdensome, and 73 percent said MIPS does not support their practice’s clinical quality priorities. These data points indicate how far healthcare’s data-driven strategy has alienated physicians, as compulsory measures that have little to do with the quality of the outcomes or patient relationships are increasingly burdensome.
Most of the data that’s generated in healthcare is about the administrative overhead of healthcare (e.g., claims data), not about the current state of patients’ health and well-being. On average, healthcare collects data from patients three times per year, leaving another 362 days of the year without tracked health information. To optimize diagnoses and treatments, predict health risks, and develop long-term care plans, clinicians need whole-patient data that provides a comprehensive picture of daily health and circumstances as well as healthcare encounters beyond the acute-care setting (e.g., primary care providers and specialists).
At best, EHRs hold only 8 percent of the data full healthcare digitization and advanced analytics require. Only 20 percent of the factors affecting health outcomes fall inside a traditional healthcare delivery system, as most of what affects health outcomes falls outside of the four walls of healthcare delivery (e.g., social determinants of health). This model also leaves no data on healthy patients, as they have no clinical encounters, who represent the ideal artificial intelligence training set. This leaves no data to train AI algorithms about how to achieve more healthy patients, not treat sick patients.
While healthcare’s digital strategy has largely ignored the digitization of the patient’s whole state of health, innovations are coming to market over the next several years that will capture more daily health data. Health tracking innovations, such as biosensors individuals can wear at all times, will eventually give patients more health data and AI-driven insights than health systems will have, empowering patients in the decision-making process.
For example, John Rogers, the founder and executive director of the Center for Bio-Integrated Electronics at Northwestern University, is producing bio-integrated electronics in the form of microns-thin, one-inch squared, skin-pliable sensors. The tiny wafers have a Bluetooth antenna, a CPU, physiologic monitors, and a wireless power system. Some professional sports teams are already starting to wear these during competition. Rogers and team aim to eventually print the sensors on skin as a dissolvable tattoo.
In the current healthcare data ecosystem, patients are embedded within a largely disintegrated healthcare delivery system, allowing for problems with handoffs between the bubbles surrounding the patients. These different bubbles are generating very little data about the patient, and, as noted earlier, the data is mostly administrative versus telemetry about the patient’s health. A data ecosystem with the patient at the center shares biosensor-enabled patient-generated data back to the healthcare system. The process constantly updates and uploads data to a cloud-based AI platform, where algorithms diagnose the patient’s condition, calculate composite and specific health risk scores, and recommend options for treatment or maintaining health.
Figure 1 shows a recommendation for a data assets roadmap for healthcare to guide data acquisition and data government strategies to truly understand the patient at the center of healthcare. Much of healthcare is stuck in the lower left quadrant of this diagram (healthcare encounter and claims data).
As data becomes more available in other areas (e.g., socioeconomic and genomics data) and healthcare prepares the resources to use it, the industry stands to broaden the scope of its data and leverage that data effectively in work-flow decision making. Guidelines can help health systems understand what the need to accomplish and have in place to achieve digitization.
To digitize in the right, sustainable way, health systems must follow these five guidelines:
Healthcare must ensure that its data-driven and digital strategies are adding to clinicians’ sense of mastery, autonomy, and purpose. Data must support their passion for their skill and sense of mission, rather than making them feel constantly monitored. These same principles must eventually apply to patients, as data-driven and digital strategies need to help patients feel like they’re mastering their own health and are autonomous.
Patient and clinician engagement require sensitivity to the human receiving the message, allowing people to face the truth without feeling threatened or over-measured. This is the human side of the data-driven strategy in healthcare, and, for successful digitization, it’s just as critical, or more so, than technology and advanced analytics.
Healthcare needs a modern, data-integrated platform that can handle the digitization. It’s still very difficult to manage the data within a domain, especially a complex domain like healthcare. The application developers working at the data layer have to wrangle and deal with data on their own. No one has pre-processed the data and made the data layer easy to access and utilize. In a data operating system (e.g., the Health Catalyst® Data Operating System [DOS™️]), however, data is the last layer in the stack, making it easier for application developers to take advantage of complex software.
A modern digital platform has seven attributes:
Figure 2 shows an example of a modern data operating system architecture (Health Catalyst’s DOS). The diagram shows curated data content in the upper-third of the diagram; this contains the intermediate data models that have comprehensive and persistent agreement about logic, making it easier for application developers in the upper-right (the DOS marketplace) to develop apps and take advantage of all the infrastructure underneath it.
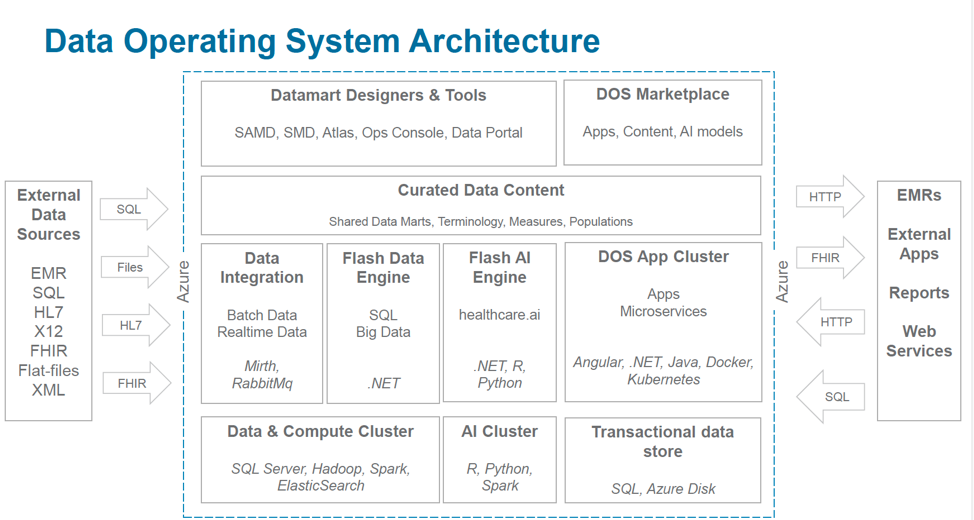
With AI algorithms as the commodities, healthcare must understand the significance of the infrastructure required to pull off machine learning in AI. Even though the public cloud makes platform infrastructure accessible and affordable, organizations that choose homegrown over commercial solutions are likely lacking the scalability and capability advanced analytics require.
Any industry requires digitization of the assets it’s trying to manage and optimize, followed by digitization of the production system for managing those assets. Using the aircraft/airline industry as an example, airplanes are the digital assets. The processes that the industry has digitized—including air traffic control, baggage handling, ticketing, and maintenance—shows the ability to manage both the people as well as the aircraft.
For healthcare to understand its assets (patients), it needs to make patients more digital. Healthcare has digitized registration, scheduling, encounters, diagnosis, orders, billings, and claims. Healthcare must now digitize beyond the clinical encounter to capture the whole picture of patient health and healthcare optimization.
Healthcare aspires towards making health optimization recommendations for patients that are informed not only by the latest clinical trials but also by local and regional data about similar patients and their real-world health outcomes over time. From a data perspective, this requires outcomes in cost data, predictive analytics, machine learning, social determinants of health, and recommendation engines.
To succeed, AI needs breadth and depth of data within the domain. This doesn’t mean only the number of records an organization has, but rather the number of facts about those patients. To round out that digital ecosystem, healthcare needs to collect more facts about each of those patients.
AI-enabled registries can provide more accurate patient information than rules-based registries. A Swedish study evaluated the ability of k-means clustering (a popular unsupervised algorithm) and hierarchical clustering (clusters with predetermined ordering from top to bottom) in AI to identify previously unidentified sub-groups of patients with diabetes. Current diabetes definitions tend to use a rules-based registry defined according to ICD codes (e.g., a lab test). Going forward, however, these registries will be more defined by the patterns that data show, not in the rules that registry users apply to and impose on the data. Increasing the density of patient data with more digitization will further enable these advanced analytics insights.
Figure 3 represents the analogy between a human brain and AI pattern recognition. In this context, a human is looking at a crowd of people and using the retina as the data collection system for feature extraction. As this individual is looking at people, she’s starting to extract features about the people—their height, weight, skin color, hair color, age, etc. When the observer immediately starts thinking about number of women in the crowd, the number of men in the crowd, the number of red heads, the number of blonds, brunettes, etc., and passes through this loop repeatedly with different data, the faster and better she becomes at feature extraction and classifying people by whatever it is that she’s looking for.
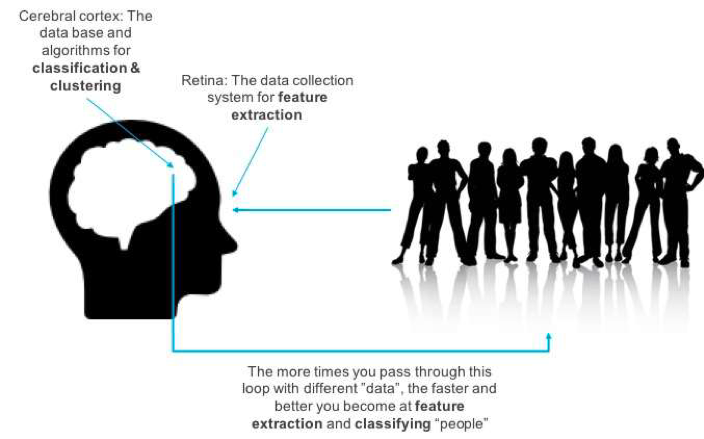
Using a neural network framework, AI mimics the human pattern recognition and classification process (e.g., telling the viewer she sees people). Generative adversarial networks (GANs) mimic the opposite human process; they describe what people look like. These GANs can start producing images of people and images of data in general. From an AI perspective, GANs might produce the ability to generate training sets like never before.
AI concepts have existing in healthcare for some time, but their application stands to change, as healthcare gains more data and AI techniques improve. A 2018 journal article about the real-time use of AI for the identification of small polyps during a colonoscopy followed clinicians using AI-enabled scopes during the diagnostic process. The study found 94 percent accuracy in the detection of small polyps. That’s significant, as these polyps are hard to identify with the human eye.
There’s a long-existing debate about data volume versus AI model sophistication—whether a complex AI model can overcome a lack of data volume and data features. There was a school of thought that sophisticated models could overcome a lack of data. A paper, however, from a team at Google revealed that simple models with a lot of data trump more elaborate models based on less data. The findings suggest that as AI models increasingly become a commodity, the data will make the difference. To achieve personalized, precision healthcare, the industry needs to invest in the accumulation of better data about patients. AI model sophistication on its own is not going to overcome the limitations of poor data and inadequate data size.
The foundational goal of healthcare’s digital strategy must be to enhance mastery, autonomy, and purpose for clinicians and patients. Keeping that human perspective first, the industry must also understand the urgency for more patient data the modern data platforms that can fully manage and leverage the information tell a more complete story about patient health. To raise the digital trajectory in the right people- and data-centered way, organizations can follow the guidelines for digitization, including engaging clinicians and patients, adopting a modern digital platform, digitizing the whole patient, understanding the importance of data for AI, and growing data volume.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.
Click Here to Download the Slides
https://www.slideshare.net/healthcatalyst1/the-digitization-of-healthcare-why-the-right-approach-matters-and-five-steps-to-get-there