Waste is a $3 trillion problem in the U.S. Fortunately, quality improvement theory (per W. Edwards Deming) intrinsically links high-quality care with financial performance and waste reduction. According to Deming, better outcomes eliminate waste, thereby reducing costs.
To improve quality and process and ultimately financial performance, an industry must first determine where it falls short of its theoretic potential. Healthcare fails in five critical areas:
1. Massive variation in clinical practices.
2. High rates of inappropriate care.
3. Unacceptable rates of preventable care-associated patient injury and death.
4. A striking inability to “do what we know works.”
5. Huge amounts of waste.
 Download
Download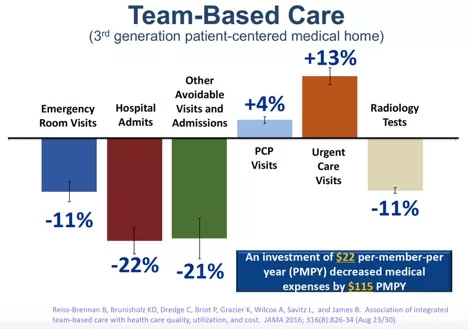
This report is based on a webinar presented by Brent James, MD, MStat, on November 6, 2019, entitled, “Making Quality Your Core Business Strategy: A Foundational Element.”
While delivering high-quality clinical care to patients is a familiar value and motivator among healthcare professionals, quality is an equally powerful business strategy with real influence on the overall health of an organization as well as its financial performance. Healthcare delivery waste (i.e., any consumption of resources that doesn’t optimally benefit the patient) drives higher costs and worsening outcomes for patients. Organizations can curtail waste, and improve bottom line, with clinical quality strategies.
According to W. Edwards Deming, the father of modern quality theory and the science of process management, higher quality outcomes eliminate waste, and value is the best quality result at the lowest necessary cost. In other words, Deming taught that by adopting the appropriate principles of management, organizations can increase quality and simultaneously reduce costs.
The key to Deming’s strategy is to practice continual improvement and think of the manufacturing or business process as a holistic system, not as separate departments. In healthcare, this holistic system is known as team-based care, a collaborative, goal-oriented approach to patient-centered care with a direct impact on a health system’s bottom line.
According Deming, process management has three classes of outcomes:
Adding cost as an outcome was fairly unique when Deming was working in the mid-20th century He then started to explore the relationship between physical outcomes and cost outcomes. He showed that, in many instances, improving the attributes of the physical outcomes (i.e., quality) caused the cost of operations to drop.
Quality theory in healthcare has an additional element when it comes to process management: every health professional (from physicians and nurses to administrators and support staff) shares a duty to pass along better quality and processes than they found at the start of their careers, producing better professionals for future generations. In healthcare, quality improvement centers on reducing waste and improving the operational areas that contribute to this waste.
The first step—the opportunity—in improving quality and process is determining where an industry falls short of its theoretic potential. Healthcare falls short in the following ways:
A closer look at the five opportunity areas above sheds light on the value of quality as a core business strategy:
Variation, the first opportunity area above, has been such a common problem in healthcare that it’s more or less impossible for all patients, even those with full access to the best care, to be getting good care. Addressing variation alone can drive down costs by about 30 percent while improving clinical outcomes.
The healthcare industry widely considers inappropriate care, the second opportunity area, care in which the risk inherent in a treatment outweighs any potential clinical benefit to the patient.
Though research isn’t conclusive, inappropriate care likely overshadows variation in care as a driver of waste and poor quality. A conservative expert estimate puts inappropriate care at 20 to 25 percent of all care delivered globally, not just in the U.S. It’s not just the costs of the care that represent waste, it’s the consequences of inappropriate care—in many cases, healthcare professionals will have to deliver more care to try to recover the initial harm.
In November of 1999, the National Academy of Medicine (formerly the Institute of Medicine) and its Committee on Quality of Healthcare in America released its report, To Err Is Human. With estimates that between 44,000 to 98,000 people die in U.S. hospitals each year or die from avoidable treatment-related harm, the report triggered a patient safety movement around the world. Subsequent research has demonstrated the 1999 estimates were conservative; the real toll is about 210,000 preventable deaths per year.
Even though U.S. healthcare outcomes are largely positive, adding an average of three and a half to seven years of life expectancy to every citizen, the industry can do better.
While patient harm (above) is an injury of commission (because the care actively harms the patient), healthcare must also look at its injuries of omission, in which clinicians fail to execute on interventions they know work for certain conditions (i.e., highly reliable care). A large national study determined that, on average, U.S. adults receive highly reliable care just under sixty percent of the time.
If U.S. healthcare can achieve miracles (e.g., adding years of life expectancy) executing correctly roughly half the time, what kind of miracles could the system realize if it delivered care correctly all the time, or close to all the time? From this perspective, the healing professions have the ability and control to change their approaches to care.
The top four areas above in which healthcare falls short of its theoretic potential are clinical opportunities. Together they produce the fifth, waste. The waste opportunity is huge. At least 30 to 50 percent of all healthcare resource expenditures are quality-associated waste, connected to the following:
In 2019 the U.S. will spend $3.6 trillion on healthcare and still produce unsatisfactory healthcare delivery. Two trillion dollars of that may be recoverable waste. For health systems this means that waste in current care delivery operations is by far the biggest financial opportunity leaders will see in their lifetimes.
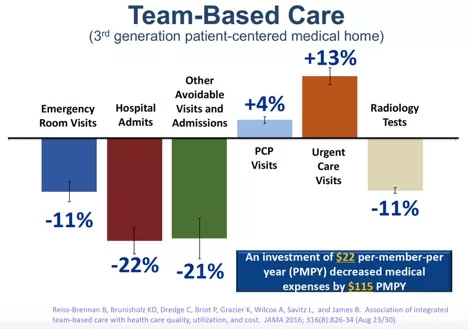
Tracking finances in a collaborative, goal-oriented team-based care approach shows that when a care team’s primary goal is improving quality of care, the improvements reduce a system’s waste and save millions of dollars. Figure 1 shows savings with team-based care at a third-generation patient-centered medical home.

In the above example of about 200,000 patients, ED visits dropped by 11 percent, hospital admits by 22 percent, and other avoidable visits and admissions (mostly specialists and outpatient procedures) by 21 percent. Not surprisingly, primary care provider visits went up a tick, which is the goal. Urgent care also went up, which is preferable over ED visits.
Overall, the investment in a team-based approach produced better care at reduced expense (specifically, a conservative investment of $22 per-member-per year [PMPY]). For every dollar spent, the team-based approach earned $5 back for a total savings of $115 PMPY, mostly by reducing hospital admits, other avoidable specialties, and outpatient procedure care.
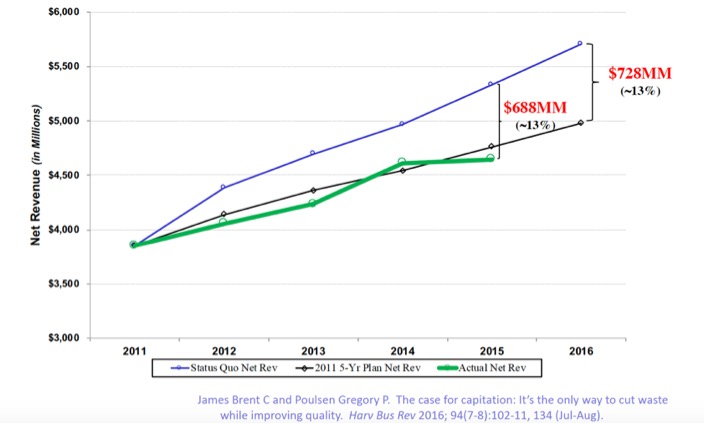
As an example of the financial impact of clinical quality improvement, Intermountain Healthcare aimed to keep its price increases lower than consumer price index (CPI) inflation plus 1 percent. The health system wanted its services available on a broad scale to the community. The blue line (going up) in Figure 2 represents Intermountain’s expected costs on a conservative projection as it grew as a system. The black line represents the target—CPI plus one. In the first four years of data, every dollar of that savings connects back to a clinical improvement project that removed waste in the system.
Intermountain dropped its total cost of operations by 13 percent—almost $700 million out of its cost of operations—showing that improving financial performance through clinical quality is an achievable reality. In most cases, better care is cheaper care, and the path to financial success leads through clinical management. This is the full financial foundation for a major international trend called pay for value.
The key factor for success in the future care delivery world is an ability to manage clinical care delivery up and down the entire continuum of care. The rate of change in healthcare delivery continues to accelerate, but the business remains clinical care delivery. Leaders in clinical change must speak the language of the key players—the physicians, nurses, pharmacists, therapists, and technicians who show up to make that care happen every day.
Healthcare professionals already have a foundational culture to drive effective clinical change within their own organizations. But how do change leaders tie the pieces together at the core of what it means to be a physician, nurse, pharmacist, or therapist down at the core of what it means to be a care delivery system? Organizations can build on endemic healthcare culture by teaching quality improvement theory and directing education at frontline care teams.
The goal is to build a widespread organizational culture layered on top of healthcare professionals’ shared values. Quality improvement theory education would also teach solving important strategic problems—driving real change for things that matter on a large scale.
Quality improvement theory education teaches the following:
This education would be costly up front, as it would pull high-paid individuals away from other work. But when organizations track these projects, they see not just the clinical outcomes of the project, but the financial savings of approaching quality improvement from an organization-wide culture. This training builds a set of colleagues to help set the culture that drives quality.
This article started by discussing Deming’s waste-based quality techniques, which changed the manufacturing world and life for all by delivering higher quality products at more affordable prices. Today, as healthcare moves into pay for value, the industry needs to echo this strategy and continuously improve clinical quality to lower expenses—delivering the best care at the lowest cost. Health systems can target waste reduction through clinical quality improvement strategies and building quality improvement-driven cultures.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.