With COVID-19 challenges continuing in the near-future, health systems must continue delivering quality care in the midst of the pandemic, without compromising financial well-being. Historical approaches to revenue cycle add value but fail to leverage data to drive financial sustainability in a time of crisis. To financially survive tumultuous economic times, health systems must leverage data to drive a more comprehensive revenue cycle strategy.
Five best practices generate the actionable data that allows health system leaders to understand financials at a nuanced level, promoting effective processes that lead to financial sustainability and optimum revenue cycle management:
1. Identify and measure the right metrics.
2. Define clear lines of accountability.
3. Create consistent workflows.
4. Define key performance indicators.
5. Understand the right metrics at the right place at the right time.
 Download
Download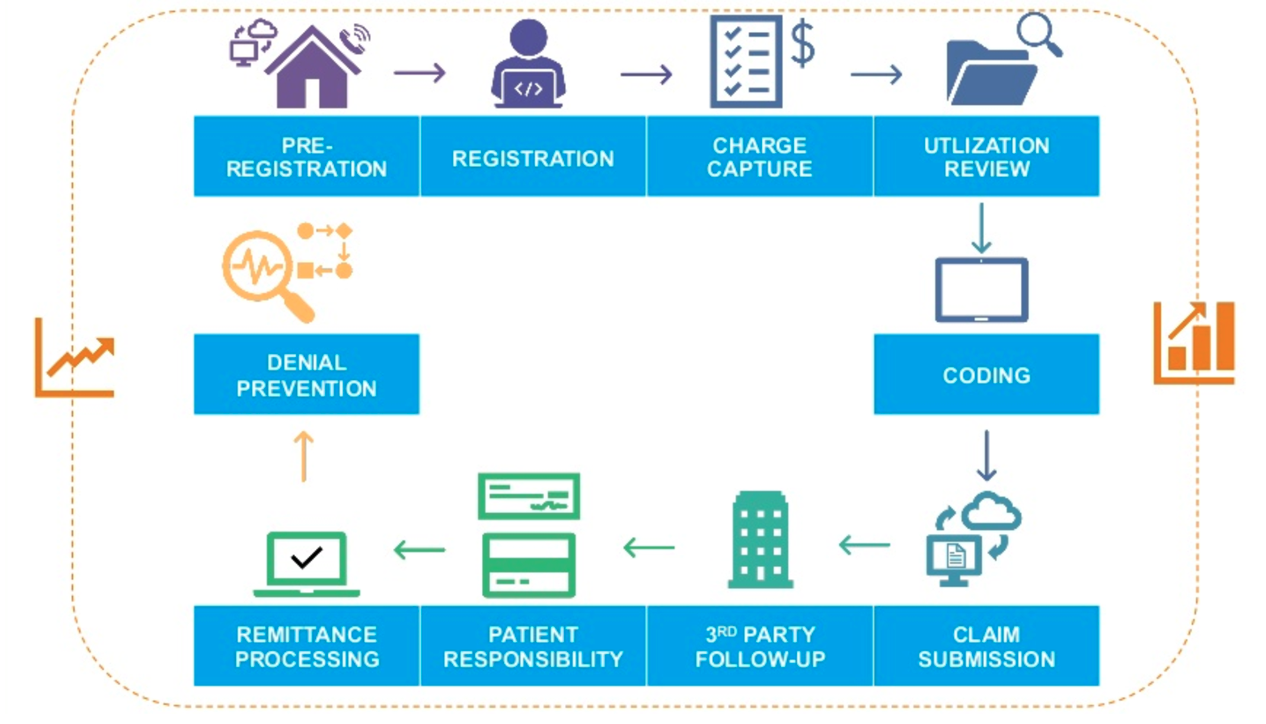
From billing and collections to completing a payment within the revenue cycle, the process to identify a patient, provide care, and then collect that revenue has come a long way from its traditional approach of billing, coding, then collecting. Now, robust healthcare revenue cycle strategies include detailed information from multiple departments within an organization because every department impacts the revenue cycle, which means leaders at every level need up-to-date data to understand high-level and nuanced financial performance.
The traditional approach to revenue cycle is a time-consuming payment process that usually involves lengthy interactions between providers, hospital staff, and payers, resulting in delays in payment. Health system leaders have realized that it’s time to change this antiquated method and take a more comprehensive approach to healthcare revenue cycle management.
Many hospitals and health systems already survive on thin operating margins with many operating at a loss and relying on cash reserves to sustain operations. Additionally, experts estimate an even bigger decrease because of lost volume and revenue due to COVID-19. For health systems to financially survive—and eventually thrive—in the new normal, they need to rethink their revenue cycle strategy, including the role that data plays in driving changes that lead to long-term financial health.
With additional cost pressures from COVID-19 (e.g., halted elective procedures, ICU resource consumption, and furloughs), hospital leaders are under more pressure to cut costs and sustain revenue. Along with financial challenges, COVID-19 has also presented opportunities for health systems to improve their revenue cycle strategy. To achieve financial viability in the short term, health systems should leverage data and analytics to identify immediate opportunities for change.
For example, quantifying and understanding the root cause of denials or controllable loss is now essential. This includes revenue that is written off from services rendered but eventually denied due to breakdowns in the revenue cycle. Other opportunities include the identification of late charges, missed charges, or undocumented supplies or procedures resulting in lost revenue. Strategically and accurately setting prices is a critical piece of the revenue cycle, requiring detailed data and analytics, that has far-reaching effects on health system revenue, reimbursements, contract rates with payers, and predicting financial needs for the future (e.g., forecasting bad debt).
Despite facing a new healthcare landscape with the COVID-19 pandemic, some healthcare leaders still rely on historical methods to manage and improve revenue cycle performance. While these practices have worked in the past and still offer value, they fail to fully maximize revenue cycle performance in a time when health systems need to react quickly to survive financially.
To adapt to the new healthcare changes and achieve optimal revenue cycle performance, health systems can follow five best practices:
The first step to revenue cycle optimization is understanding what to measure. Whether finance teams choose to measure revenue capture or uncollectable accounts, identifying and tracking the right metric is the foundation of short- and long-term success.
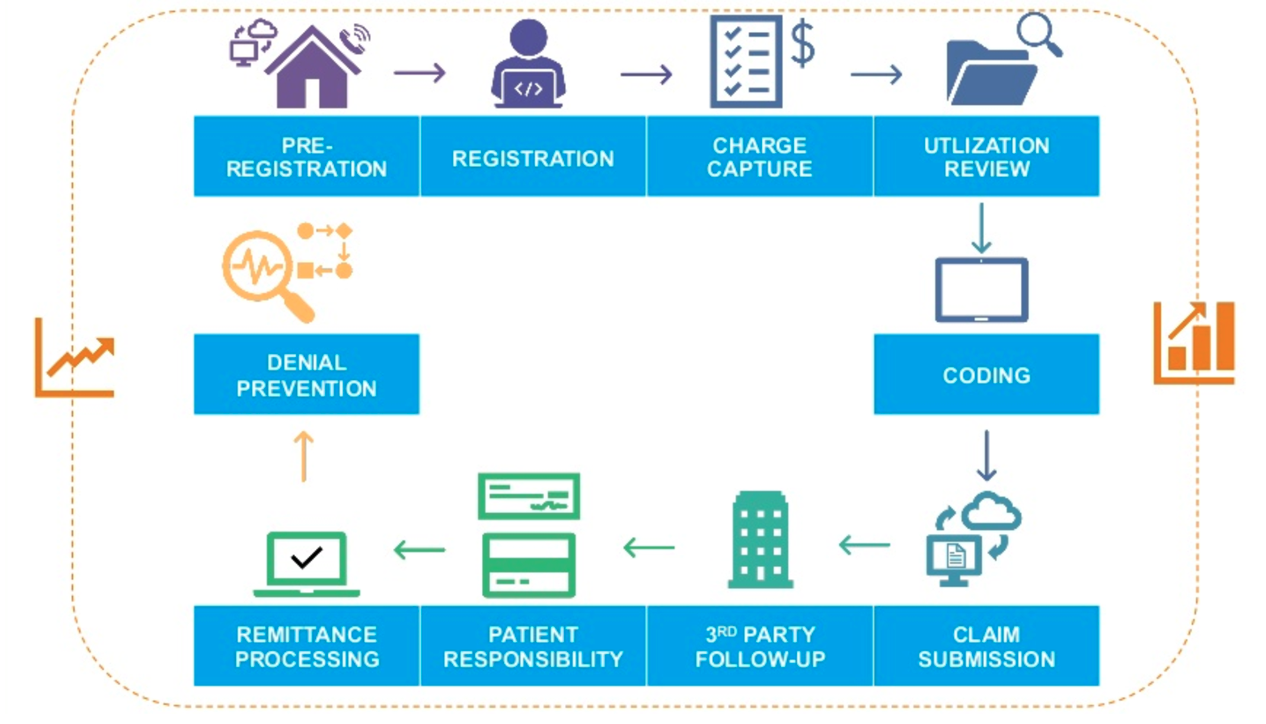
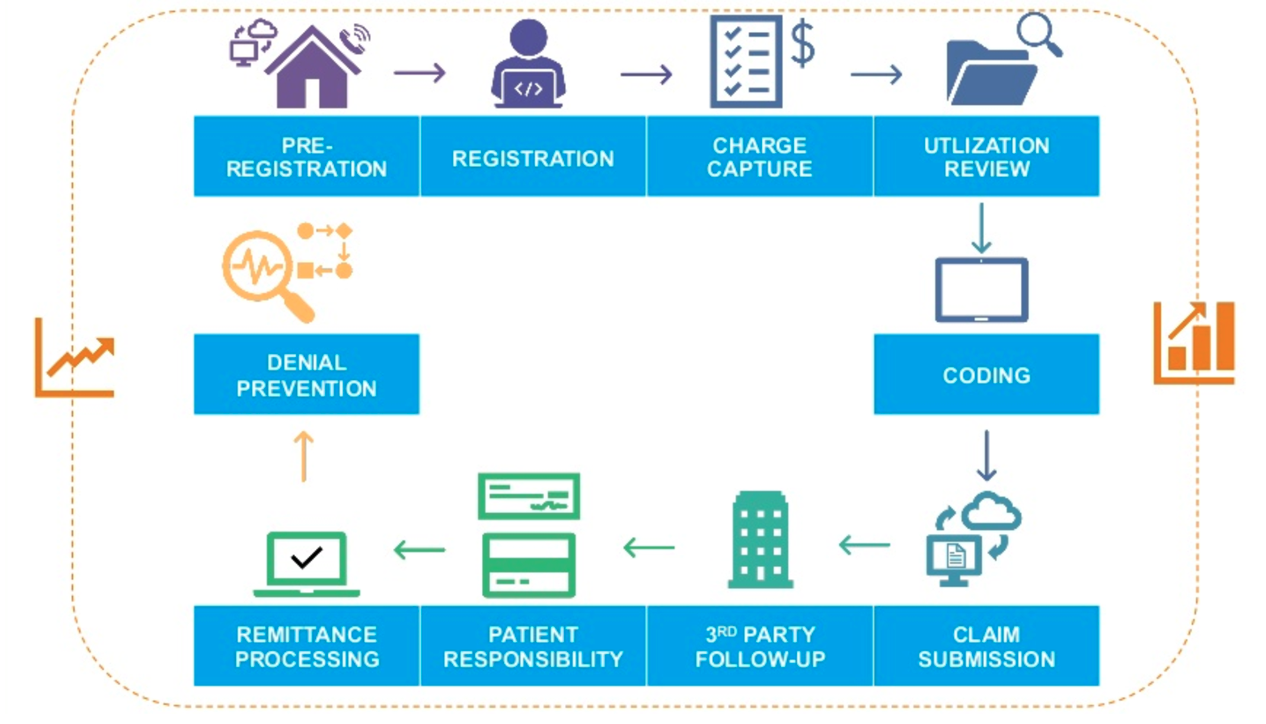
The revenue cycle is a complex process full of moving parts, making it difficult to measure every step or handoff throughout the lifecycle of a claim (Figure 1). Although it’s a tall task, health systems achieve real change when they can measure every handoff throughout the process.
Precise measurement allows clear lines of accountability. Clear lines of accountability along with clear reporting structures enable leaders to understand who is responsible for which specific metric, and therefore, responsible for driving the performance of that metric.
Identifying and measuring the right metrics also makes the health system accountable to itself. With an accurate baseline of metrics, revenue cycle teams can measure the success of new interventions, make changes accordingly, and report back to leadership, showing accountability for the resources allotted. The ability to quickly measure the effectiveness of new processes is especially helpful in a volatile market when health systems are trying new interventions to grow and improve the patient experience.
Established, standardized workflows create a uniform, disciplined approach to any process within the revenue cycle. The workflow should look the same throughout the revenue cycle process, no matter the point of access. Ensuring workflows are well-documented and teams are following the workflows correctly are critical components of effective handoffs throughout the revenue cycle journey.
One cohesive, agreed-upon approach also allows revenue cycle leaders to more effectively train staff and help them understand the process at a higher level. Understanding the revenue cycle goals at a high level, and how each person’s role fits within the big picture, empowers leaders systemwide to consider the complete revenue cycle in the decision-making process.
Revenue cycle leaders need to comprehend that data and metrics don’t equate to information. Data and metrics are the building blocks to reach meaningful information, but a crucial in-between step is developing key performance indicators (KPIs). KPIs play a valuable role in helping staff identify the data that will drive decision making.
Leaders should choose KPIs according to relevancy and organizational goals and apply KPIs where they can affect real change. Another essential part of the KPI development phase is developing indicators for each process at the functional level, not just at a high level. KPIs need to target metrics that will help solve problems and drive change within the workflow. KPIs should drive most important organizational decisions, so leaders should review them regularly and choose wisely.
Leaders can drive real change when they can access the right metrics. For example, a chief financial officer might be more interested in overall strategic metrics instead of operational measures, such as bill edits or late-charge metrics, but a VP or director-level leader wants to consider more granular, detailed data while making financial decisions. Production measures and overturned denial metrics could be significant operational insights to a manager who can drive change in that area. In this way, establishing the needed metrics for the targeted role means actionable information surfaces to the person who has the power to change it.
As the uncertain future of healthcare delivery continues to affect revenue cycle management, health systems need safeguards to ensure their financial well-being. Data and analytics provide critical insights to financially survive COVID-19 and future operational challenges, pushing aside the outdated billing, coding, and collections approach that fails to include key departments that impact the healthcare revenue cycle.
Data and analytics are the lifeline for successful, sustainable revenue cycle management, but optimization can’t stop there. Tracking the right metrics, promoting accountability, creating consistent workflows, and identifying the right KPIs—all based on the right data—are necessary for health systems to optimize revenue cycle and achieve higher profit margins. With the right processes that turn data into action, leaders can focus on achieving the optimum revenue cycle model.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.