Besides improving your information systems and educating your staff on the ins and outs of managing revenue, there are many more opportunities for improvement. Here are five suggestions to help health systems improve their revenue cycle management:
1. Trend and benchmark your healthcare data.
2. Use DOS to Mine Your Healthcare Data.
3. Constantly ask frontline staff for suggestions.
4. Monitor all payer contracts.
5. Maintain convenient and caring touch points with patients.

With cash flows declining, margins tightening, and bad debt increasing, it’s more important than ever to maintain a steady stream of income for your hospital. This goal may seem difficult, but there are many opportunities to significantly improve your revenue cycle management.
As a long-time executive in the healthcare finance realm, I’ve spent years implementing financial solutions for various health systems.
Along the way, I’ve discovered a few tried and true solutions. While it’s important to choose the appropriate information system components based on a health system’s size and to educate the staff on the ins and outs of managing revenue, the following five suggestions will also help improve your revenue cycle management.
We all know the maxim: you can’t measure what you don’t manage. This is true with healthcare data as well. If you start trending and benchmarking your data, you’ll be able to identify areas to improve your revenue cycle.
The best way to trend your data is to use the healthcare data operating system(DOS™). DOS combines data from your disparate IT systems — clinical, financial, human resources, patient satisfaction scores, and more — and optimizes it for analysis. As you review the data, you’ll be able to use visualizations, which will help you better understand the results as you drill down and discover the root cause of certain trends. When trending, be sure to look at both hospital and physician billing data for a full picture of your revenue cycle.
To find out how you compare to other health systems, you can purchase benchmarking data. An economical option is HFMA’s (Healthcare Financial Management Association) MAP (Measure, Apply, Perform) initiative, which sets the industry standard for revenue cycle excellence. If you’re an HFMA member (a nominal fee), you can access benchmarking data through MAP.
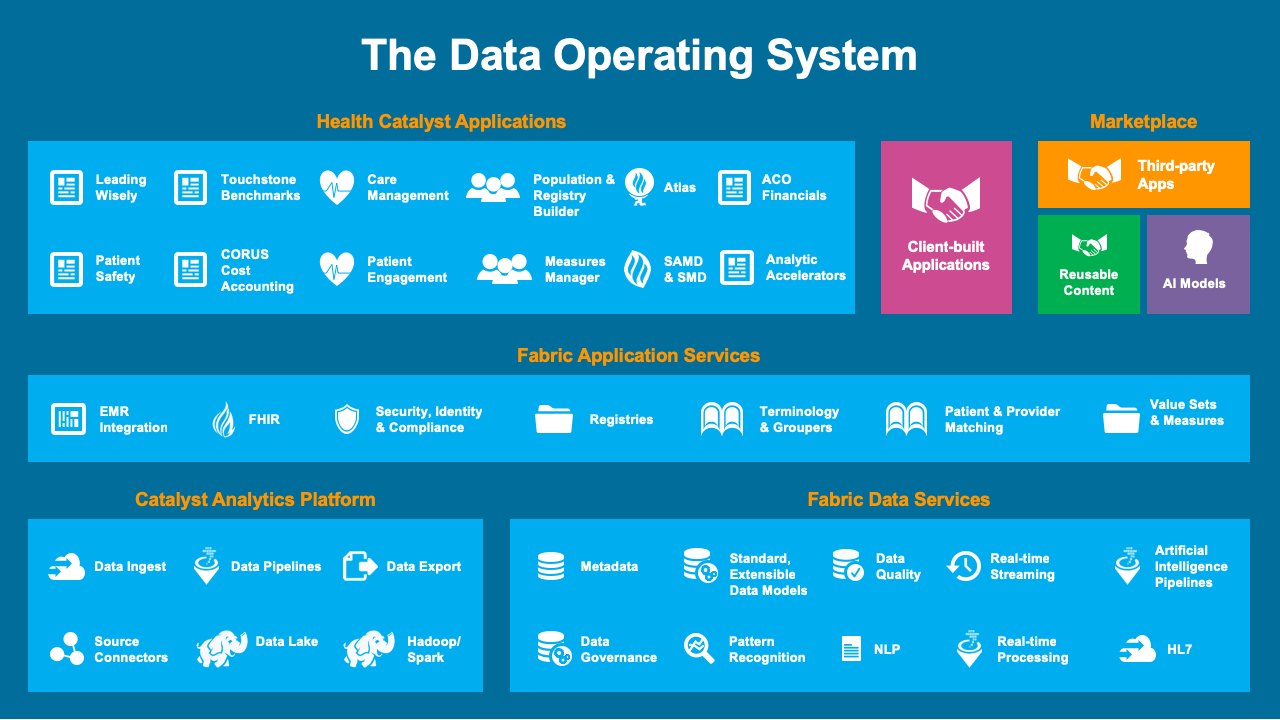
DOS is a powerful solution that enables you to mine your data, discover roadblocks, and determine how to improve. Get a good analyst to go behind the scenes and see what the data reveals — and then work to implement change in your organization. This process must be done in a positive atmosphere. To illustrate: I was helping a client who had a lot of denials that were significantly affecting their revenue cycle. We analyzed their work queues and discovered that many of the queues weren’t being touched; outstanding bills were just sitting there. I loved the response of the manager; he simply said, “How can we improve?” There was no blame game, just an atmosphere of improvement. After doing a workflow analysis, we discovered the roadblocks, set up new queries to automate the manual work, and created exceptions to monitor. With DOS, experienced analysts, and a culture of improvement, this process was easy.
Trending and mining data with DOS is invaluable for gaining insights to improve your revenue cycle management. But don’t forget an equally important resource: your frontline staff.
After you’ve identified a roadblock, consult your frontline staff for suggestions about the best way to solve the problem. Then, continually check back with them for additional suggestions. Reexamine your workflow on a periodic basis, and ask the following questions:
Frontline staff have a lot of insight to share — and making them active participants in a culture of improvement helps to guarantee sustainable change.
With margins growing tighter, monitoring your contracts and communicating clearly and frequently with payers can make all the difference. Make sure payers aren’t under-reimbursing you, denying too many claims, or putting unreasonable demands on your patient accounting office. Use your analytics system to easily measure the yield. Is it changing over time? What should it be? As we move to value-based purchasing, such monitoring will become far more difficult — and an analytics system absolutely necessary.
Use any touchpoint you have with patients as a public relations possibility. Every person who registers or schedules a patient should have skills to do their job efficiently and with a caring attitude. By making it convenient and pleasant for the patient to do business with you, you are far more likely to get correct and complete registration and insurance information. It also pays to offer a well-designed, branded patient portal to increase patients’ satisfaction and give them the opportunity to pay bills online.
Here is a brief example. I worked with a physician group who was having problems with increasing collection time in accounts receivable. We discovered that the root of the problem was a poor process at the registration desk. By simply scripting questions for the registration staff, we were able to decrease collection time in accounts receivable, thus increasing cash flow, while also continuing to provide a good first impression for patients.
See how North Memorial Health Care increased labor productivity, reduced costs, and improved clinical quality by adding an advanced analytics application.
Have you had success improving your revenue cycle management? If so, what processes or solutions were the most helpful?
Would you like to use or share these concepts? Download this Hospital Revenue Cycle Management presentation highlighting the key main points.
Click Here to Download the Slides