The transition to ICD-10 in 2015 saw the number of available procedure codes increase from roughly 3,000 to more than 70,000. This change gives clinicians the ability to code procedures to a much higher degree of specificity and provides health systems the ability to unlock powerful clinical insights into how inpatient procedural care is delivered.
This article covers the benefits and drawback of ICD-10 PCS, as well as concrete ways health systems can use these procedure codes to provide new clinical insights. The article also walks through the anatomy of the seven-digit alphanumeric codes and provides specific clinical examples of how healthcare organizations can slice and dice this data.
 Download
Download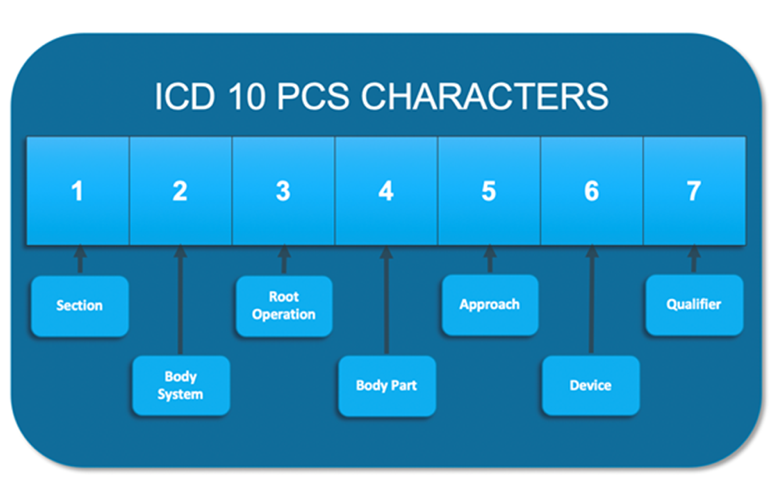
When the U.S. healthcare system transitioned from ICD-9 to ICD-10 codes in 2015, the number of available PCS (Procedure Coding System, a U.S. classification system referring to procedures in an inpatient setting) codes jumped from roughly 3,000 to more than 70,000. This drastic increase means clinicians can code procedures with a much higher degree of specificity. In addition, ICD-10-CM diagnosis codes increased from 13,000 to 68,000.
Although the shift to ICD-10 required healthcare organizations to change how medical encounters are documented, doing so gives organizations the ability to harness powerful analytics behind ICD-10 procedure codes. Armed with new insights into how inpatient procedural care is delivered, health systems can improve patient outcomes and value.
Health Catalyst uses a Clinical Integration Hierarchy, which allows for more precise analysis of the care provided—and thus more actionable data for clinicians or administrators to review.
The Clinical Integration Hierarchy heavily utilizes ICD diagnosis codes to organize and analyze data according to care processes. This hierarchy groups healthcare into work processes that reflect how care is actually delivered, across departments and care settings, and provides a relevant, focused structure for prioritizing and implementing improvement initiatives. By organizing and analyzing data according to care processes, health systems can determine which of these processes offer the greatest opportunity for improving quality and reducing unnecessary cost.
Similarly, Health Catalyst is now building a Procedural Integration Hierarchy utilizing procedure-based code. This allows healthcare organizations the ability to glean important analytics insights using procedure data as well as leveraging the higher degree of specificity that ICD-10 allows. The addition of a procedural integration hierarchy will complement the clinical integration hierarchy and allow clinicians and hospital leaders more contextual information.
For instance, health systems are currently unable to identify by diagnosis codes if transplant patients had the transplant on their current encounter, or if the admission was related to underlying management of their medical condition. This is crucial information when looking at variation in costs, length of stay (LOS), and/or rates for readmission. There’s the potential for significant variation in surgical costs and medical management from one patient to the next by simply looking at diagnosis codes. Similarly, when looking at procedure codes, three different patients may have had a portion of their colon removed for varying reasons (e.g., a gun shot, colorectal cancer, severe irritable bowel syndrome [IBS], etc.). All three patients would show as having colectomies but the length of LOS, processes, and outcomes could be intentionally different. Neither coding tool provides a full picture, as it captures single variables when classifying a patient stay; the procedural hierarchy will help add content and context to the data available. The ICD-10 system is structured for an analytics platform, such as the Health Catalyst® Data Operating System (DOS™), to harness information about a health system’s patients.
The International Classification of Diseases (ICD) was initially developed and published by the World Health Organization (WHO) to standardize healthcare reporting worldwide. According to the WHO, “ICD is the foundation for the identification of health trends and statistics globally, and the international standard for reporting diseases and health conditions.” Many revisions of ICD have been made and ICD-9 was not expansive enough for future healthcare needs with its limited number of codes and outdated information.
Even though the transition to ICD-10 in 2015 disrupted the healthcare industry, the potential analytic likely outweighed the disruption:
The structure of the ICD-10 PCS system is designed in a way that has the potential to drive powerful analytic insights. Each character can be one of any 34 possible values (numbers 0-9, and letters A-Z, excluding letters O and I to avoid confusion with numbers zero and one). Additionally, characters have a hierarchical relationship and the same character placed in a different position has a different meaning (Figure 1).
The following example identifies the meaning of each character of the code:
Right knee joint replacement = 0SRD0JZ
0 = Medical and Surgical Section
S = Lower Joints
R = Replacement
D = Knee Joint, Right
0 = Open
J = Synthetic Substitute
Z = No Qualifier
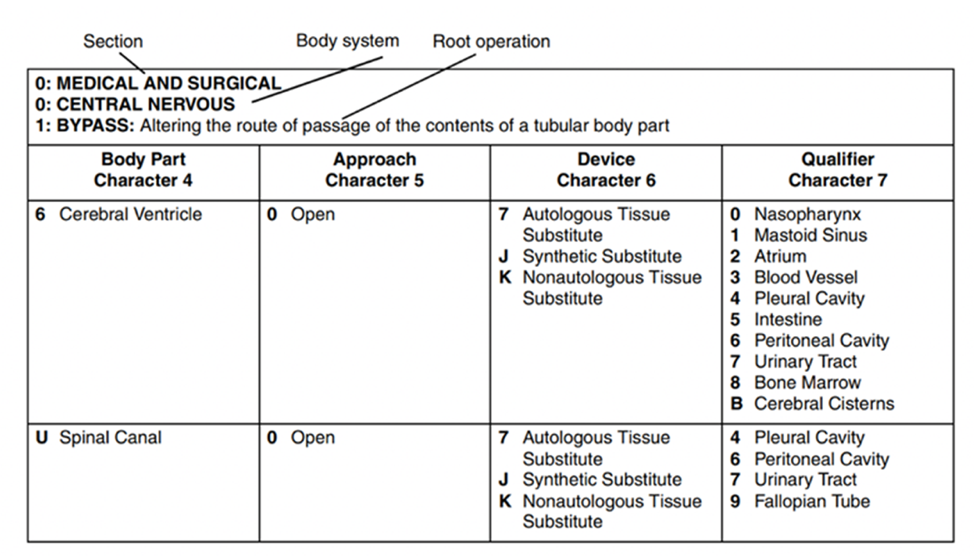
Going hand in hand with specificity, ICD-10 procedure codes precisely define procedures with detail regarding body part, approach, medical devices used, and other qualifying information. The addition of laterality, such as right-knee replacement vs. left-knee replacement can add additional clinical insights to data.
Additionally, the definition of each character is a function of its physical position in the code. For example, the fifth character of the procedure code refers to the approach type, so a hospital administrator could look at the total volume of open procedures or the total volume of minimally invasive surgeries using just the fifth character. Adding the seventh character, an administrator could look at the total number of biopsies performed across the system on a specific body part, for example. These examples help highlight the powerful level of specificity available for analysis using procedure codes.
ICD-9 procedure codes contained only three to five numeric characters, limiting space for adding new codes. ICD-10 PCS was designed to have the flexibility for adding new codes as new procedures are added or new technologies come into play.
With the release of ICD-10 procedure codes, CMS standardized the definitions of all procedure codes. ICD-10 PCS provides precise and stable definitions of all procedures performed where ICD-9 procedure codes were based on outdated technology and lacked current, accepted definitions. While this standardization is in many ways a benefit of ICD-10 PCS, there are also some drawbacks.
Drawbacks include the following:
The standardization of procedure codes brought stability and eliminated outdated terminology but did result in the limitations noted above. A good example is the elimination of eponyms, which resulted in the elimination of some well-known procedures like the Whipple, defined by the Mayo Clinic as “an operation to remove the head of the pancreas, the first part of the small intestine (duodenum), the gallbladder and the bile duct.” With ICD-9, the Whipple was coded as Radical Pancreaticoduodenectomy, better known as a 52.7. With ICD-10 PCS, the Whipple procedure is now often defined by the use of the following seven unique procedure codes:
Similarly, ICD-10 PCS does not include common procedure names, terms or acronyms, such as appendectomy, coronary artery bypass grafting (CABG), or total knee arthroplasty (TKA).
As a result of increased specificity, with some complex procedures or multiple step surgeries, it can be difficult to determine what procedure was performed by looking just at the primary procedure code. In many cases, it may be necessary to look at secondary procedure codes in relationship to the entire procedure in order to correctly identify the type of surgery that was performed. A good example of this is with a total knee replacement. A total knee revision is often coded the same as the initial replacement, with the addition of a secondary procedure code. For example:
With ICD-10, there can be multiple procedure codes to document and analyze. In the case of the knee replacement above, if someone looked at only the primary procedure code, he could easily misclassify the procedure. Between the two procedures–total knee replacement and total knee revision–there would be intended variation between the two procedures such as time metrics in the operating room, difference in length of stays, readmission rates, or even cost case events. All of this intended variation would be inaccurately shown as unintended variation if only looking at the primary procedure code.
Health Catalyst’s Clinical Integration Hierarchy provides access to complete, contextual information that may bring healthcare systems new and unique clinical insights. With the addition of the Procedural Hierarchy, clinicians and administrators could look at the procedure codes in conjunction with the principle discharge diagnosis to gain insight into why the patient was hospitalized in the first place. Or, they could look at what type of surgeon is performing a procedure and how the outcomes compare to a different type of surgical specialty performing the same operation. Insights can then be shared in order to improve patient outcomes and analytics can be used to facilitate such conversations.
The multitude of scenarios this Procedural Hierarchy can impact are broad. A health system could build clinically defined criteria, based upon current best-practice recommendations, incorporating procedure-based logic that in-turn can correctly identify patients who may benefit from a higher hemoglobin threshold in comparison to a healthy patient with trauma. They could create cohorts within a total joint application to construct population as to the benefits of uncemented vs. cemented arthroplasty. Clinical leaders could examine outcomes when robotic instruments are used vs. when they are not. There is an almost endless amount of possible ways that a healthcare system can use ICD-10 procedure codes to carve, slice, and examine their data. The bottom line from an improvement standpoint is that Health Catalyst is continuously building insights and consolidating data in such a manner that has not previously been available.
As with other development, Health Catalyst is employing a pragmatic approach by using the Pareto principle in order to provide the logic for 80 percent of the cases and leaving 20 percent to be customized to the specific needs of a health system or improvement project. And, as the Procedural Integration Hierarchy is being built, developers are creating the ability to pull data directly from the CMS website when changes in procedure codes are released. This is just one example of the benefits of DOS™ Marts–the ability of healthcare systems to rely on experts in a variety of areas, accessing pre-baked content to reduce the workload on analysts so they can focus on ensuring the data is valid and tailoring queries to fit their specific needs.
Just like the Clinical Integration Hierarchy, the Procedural Integration Hierarchy ties back to the three systems approach. The best way to achieve and sustain quality and cost improvement is a systematic approach (the best practice, analytics, and adoption systems). Healthcare organizations must implement all three systems to achieve ongoing success. In addition, the three systems must work together. Health Catalyst is ultimately much more than an analytics solution, but also an access point to experts in a variety of areas who pave the way for all aspects of healthcare improvement.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use these concepts or share with a colleague? Download this presentation highlighting the key main points.
Click Here to Download the Slides
https://www.slideshare.net/slideshow/embed_code/key/vTsXBY7xC5bhcd