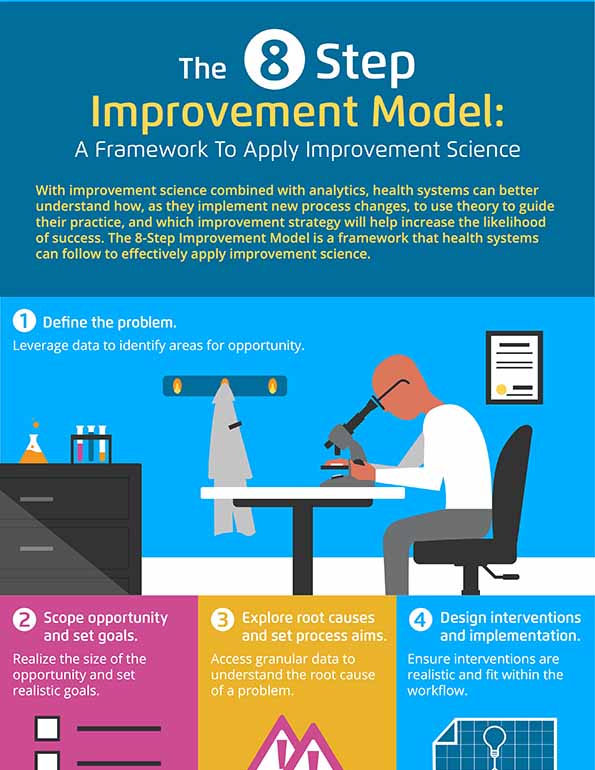
With improvement science combined with analytics, health systems can better understand how, as they implement new process changes, to use theory to guide their practice, and which improvement strategy will help increase the likelihood of success.
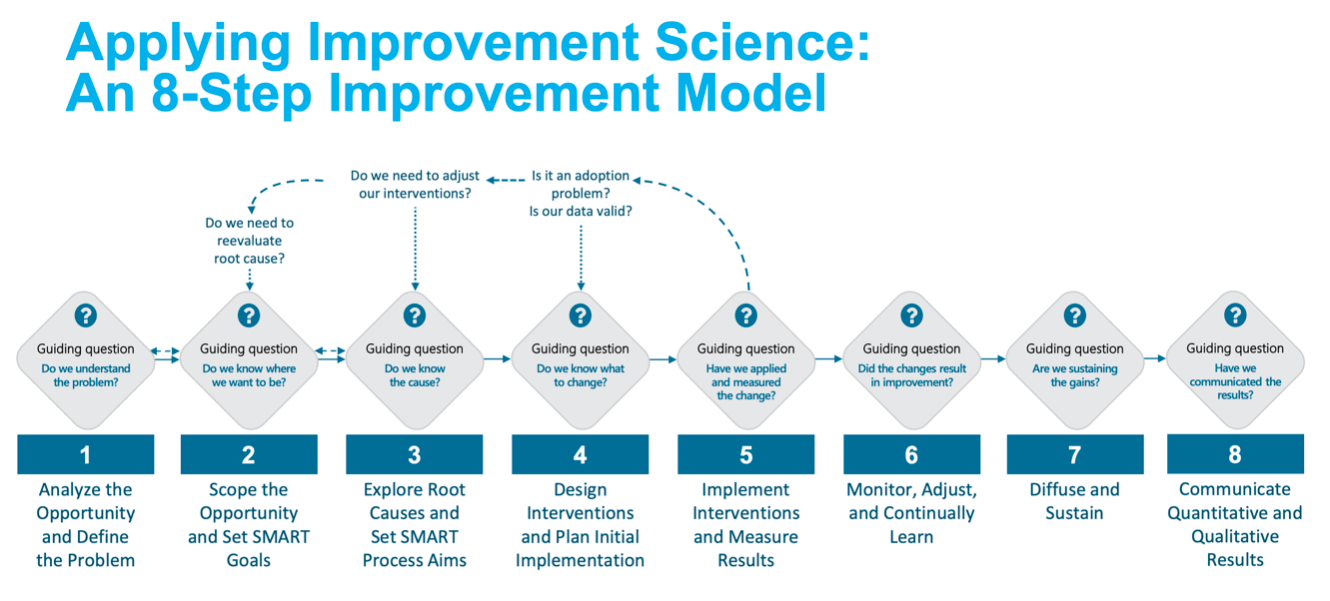
The 8-Step Improvement Model is a framework that health systems can follow to effectively apply improvement science:
1. Analyze the opportunity for improvement and define the problem.
2. Scope the opportunity and set SMART goals.
3. Explore root causes and set SMART process aims.
4. Design interventions and plan initial implementation.
5. Implement interventions and measure results.
6. Monitor, adjust, and continually learn.
7. Diffuse and sustain.
8. Communicate Quantitative and Qualitative Results.
With the right approach, an improvement team can measure the results and know if the changes they made will actually lead to the desired impact.
Today’s healthcare landscape is witnessing exponential growth in healthcare data. In the past, health systems were faced with collecting, collating, and classifying overwhelming amounts of data. Now, health systems face a new challenge—how to use that data to drive improvement.
Although some healthcare leaders are embracing new technological advances, historically, healthcare has been slow to adopt new technologies for a myriad of reasons, including budget constraints and regulatory burdens. Another reason for the slow rate of technology adoption is a health system’s inability, or personnel lack of experience, to effectively implement changes in practice, including using the correct methods to understand the impact of technology and practice changes on outcomes.
Improvement Science is one of the answers to these common data and technology challenges. It allows for the scientific study about which improvement strategy works best in the complex system of healthcare.
Healthcare teams can use improvement science and analytics to understand how, as they try something new (e.g., implement a new technology or change in practice), to use theory to guide their practice, which methods will help increase the likelihood of success, and how an improvement team can know if the changes they made lead to the desired impact.
Unwarranted clinical variation is all too common for healthcare systems; it occurs when notable differences in medical practice utilization can’t be explained by a predisposition to illness, medical need, etc. Although unwarranted clinical variation has improved in the overall healthcare industry overtime, it is still one of the biggest areas in which health systems can improve. In fact, it is estimated that unwarranted clinical variation represents between $20 and $30 million dollars for every $1 billion dollars in revenue, a huge financial opportunity for providers.
To apply improvement science, understand clinical variation, and take the right measures to overcome this unwarranted variation, healthcare leaders must understand the two types of variation. The first is common cause variation and the second is special cause variation.
Common cause variation is a variation that is inherent in a system (process or product) over time; it affects everyone working in the system and affects all outcomes of the system. Special cause variation is not always a part of the system and doesn’t affect everyone. Special cause variation is attributable to a specific cause and is nonrandom. Real improvement effort requires that leaders can recognize if the results are inherent to the process (common cause variation) or if they are due to some identifiable cause (special cause variation).
If leaders aren’t able to identify the type of variation, they can make one of two large mistakes: 1) Acting like something is a unique event when it’s normal for the process, and 2) Ignoring issues that are special variation, assuming the variation is normal. Without the ability to display data/performance over time, it is impossible to know if process changes are producing the desired results.
The 8-step Improvement Science Model (Figure 1) provides one approach for applying improvement science in healthcare. The key to improvement science is using and applying a consistent model to drive improvement and using meaningful data in every step.
The first step in tackling unwarranted clinical variation is using data and analytic insights to identify areas for opportunity. Robust analytic capabilities are key to identifying improvement opportunities.
A strong analytics platform with the ability to aggregate data from a variety of sources, including disparate EHRs, human resource information systems, supply chain systems, and revenue cycle systems, provides a complete picture of a health system’s performance. When leaders have access to comprehensive data and analytic insight, they can accurately identify problem areas, then focus on improvement efforts to decrease unwarranted clinical variation, improve quality, reduce costs, and improve financial performance.
Analytics help health systems scope the size of the improvement opportunity. With the ability to dive deeper into the data, health systems can drill down and understand the depth and breadth of a problem.
Access to specific, granular data allows leaders to understand what is at the root cause of a problem. Larger, high-level data sets are helpful, but they don’t allow leaders to understand the why behind specific problems.
For example, a health system experiencing high catheter-associated urinary tract infection (CAUTI) rates, needed more nuanced data to understand what was causing the increased rates. With aggregated data from eight different hospitals, leadership didn’t know if the high CAUTI rates were occurring at all hospitals or only a few.
When the health system obtained specific data, it learned that the high rates were due to several reasons, such as inconsistent CAUTI insertion techniques, failures to adhere to CAUTI maintenance bundle compliance, and lack of proper routine hygiene. The root causes at the individual facilities within the larger system varied, requiring different improvement plans and interventions at each location. With this specific information, the health system understood which problems it needed to solve and put the appropriate measures into place, subsequently reducing the incidence of CAUTI systemwide.
Change concepts help prompt new ideas for improvement by providing a basic framework for improvement team members to consult before making any drastic changes. The change concepts list (Figure 2) is based on common challenges that all healthcare organizations face. Therefore, if an improvement team is struggling to identify one specific improvement opportunity, they can review the six change concepts and the list can help generate an improvement intervention.
Successful interventions also require the right people to comprise the improvement team. It is valuable to include system leadership, day-to-day leadership, and the right technical and clinical expertise, but without engaging front-line staff—to ensure that implementation steps are realistic and fit within the workflow—improvement teams and their interventions will fail.
Before moving to implementation, teams need to prepare the implementation plan. Teams must ensure they understand the current state, resources required for change, and organizational readiness for change. Improvement teams need to develop a communication plan, provide training, including onsite support, if needed. Teams also need to determine how they will measure impact of that intervention on the outcome measures of interest, and track performance over time. When considering which intervention is best, improvement teams increase the likelihood of improving outcomes if they integrate a model of evidence-based practice into the analytics-driven improvement efforts.
Many health systems use scorecards to evaluate the effectiveness of their improvement efforts. While scorecards are important and promote internal accountability, they are not the right tool for measuring results. When measuring improvement work, the right measurement tool should be able to answer the question, “Are we getting better?” To answer that question, we need to understand common and special cause variation, and need to visualize performance over time—something run charts do well.
Run charts are simple to use, making it one of the best tools to measure improvement. A run chart provides a variety of benefits for teams trying to measure improvement success. For example, a run chart (Figure 3) shows improvement teams how well or how poorly a process is performing at the start of the improvement work. Teams can apply the run chart rules to determine when changes in the data are actual improvements versus common cause changes over time, and it offers direction as team members work on additional improvement projects.
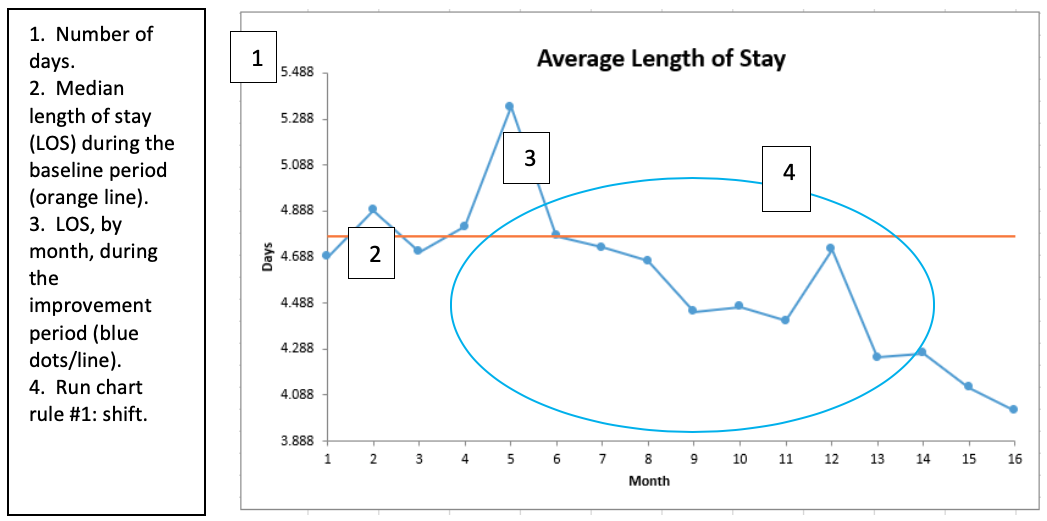
After an improvement team has implemented the right intervention and selected the best way to measure results, the team must stay focused on that improvement effort. Consistent monitoring and adjusting will allow team members to make changes that allow improvement efforts to reach their potential. Teams can continue to use a run chart to monitor the effectiveness of improvement efforts. If the run chart shows that improvements aren’t happening, teams can immediately adjust interventions quickly, reduce unnecessary waste, and apply better-suited interventions.
Improvement science, combined with measurement tools, empowers health systems to diffuse and sustain gains. One of the biggest challenges associated with improvement work is sustainability, which is often just as hard, if not harder, than making the initial improvements.
With an improvement model that delivers the desired outcomes and an experienced improvement team, a health system can spread its improvements to other areas of the health system and avoid starting from scratch when defining future improvement projects. Because scalability is a common challenge with improvement projects, it is important that improvement teams—from the start of every project—consider how the improvement efforts can be replicated or tweaked slightly to work for another part of the organization.
After a successful improvement project ends, it is also important for the improvement team to ensure sustainability over time. This may take regular check-ins or continued conversations with leaders, but it is a must-do to keep improvement work going.
A valuable step that is often overlooked or forgotten by improvement teams is communicating results, whether good or bad. Reporting results internally holds team members accountable and acknowledges the value of each team member’s work. Acknowledgment can also motivate team members to stay committed to (often) challenging improvement work.
Sharing results is also a way to garner executive support for current improvement work and gain momentum for improvement work in the future. Improvement leaders also have a responsibility to communicate what works so that other departments can apply the same (or similar) principles, accelerate improvement, and benefit the patient populations they serve.
Improvement science provides a valuable framework for improvement efforts in the complex world of healthcare, and analytics is a key part of that framework. Without the ability to deeply understand performance through data, health systems cannot improve. It’s also imperative for health systems to select the right members to comprise the improvement team and equally imperative for the improvement team to understand how to identify and validate improvement through the right tools, such as a run chart. Lastly, improvement team leaders must communicate results to other team members throughout the organization and executive leadership to gain support for improvement efforts and instill a sense of accountability. After all, improvement strategies and roadmaps are only useful if team members actually apply these new improvement principles in their everyday work.
With so many challenges to tackle every day, identifying areas for improvement and executing an improvement plan can seem daunting to healthcare leaders, but the results are far worth it. Effective improvement science in healthcare can eliminate unwarranted clinical variation, resulting in improved outcomes for patients, improved financial performance, and reduced costs of care.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.
Click Here to Download the Slides
https://www.slideshare.net/slideshow/embed_code/key/KwtwG2yHzuJiWe