With clinicians driving many of the decisions that affect health system quality and cost, they’re an essential part of successful improvement efforts. Clinicians are, however, notoriously overburdened in today’s healthcare setting, and getting their buy-in for additional projects is often a big challenge. To successfully partner with these professionals in improvement work, health systems must develop engagement strategies that prioritize clinician needs and concerns and leverage data that’s meaningful to clinicians.
Improvement leaders can approach clinician engagement on three levels:
1. Clinician-led local programs.
2. Department- or division-level programs.
3. Leadership-level growth and improvement programs.
 Download
Download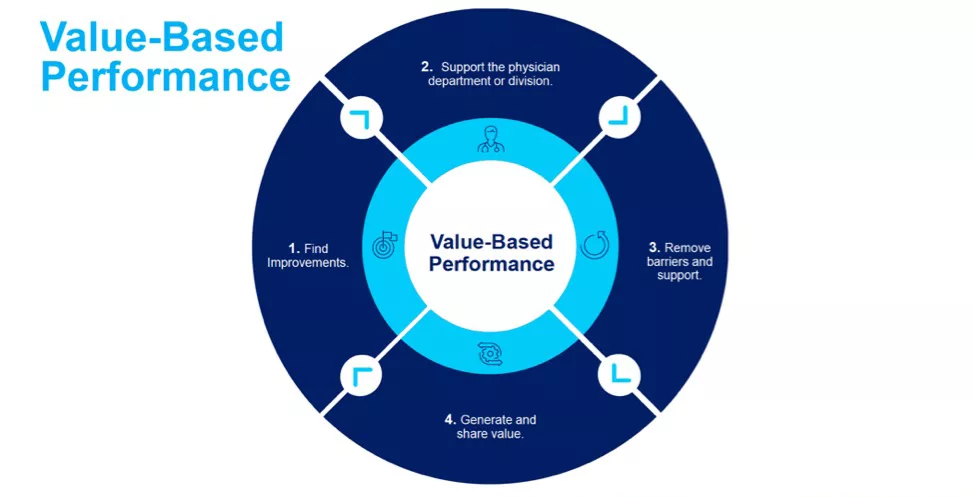
This report is based on a 2019 Healthcare Analytics Summit (HAS 19) presentation given Jack Beal, JD, Vice President, Performance Improvement and Deputy General Counsel, The University of Kansas Health System, and David Wild, MD, MBA, Vice President, Performance Improvement, Assistant Professor, Department of Anesthesiology, The University of Kansas Hospital, titled, “The Doctor’s Orders for Engaging Clinicians to Drive Improvement.”
Clinicians play a significant role in all decisions affecting health system quality and cost, making them critical players in improvement work. However, reimbursement pressures, competing time pressures, misaligned incentives, and a lack of credible data often make engaging clinicians in improvement work one of the biggest challenges in healthcare.
This report describes effective strategies for overcoming barriers when engaging clinicians in improvement work and shares how to achieve the following goals:
Clinicians face mounting challenges in addition to delivering care, including climbing student debt, administrative requirements (e.g., regulatory measures), and the undelivered improvement promise of the EMR. While clinicians are accustomed to a professional culture in which they’re the primary decision makers at the point of care, data-driven decision making and improvement work are altering that paradigm. Health systems must strategically engage with clinicians regarding improvement work by inviting clinicians to become partners in these efforts rather than adding to the burden.
Clinician engagement is not a technical problem; it’s an adaptive problem. As such, simply throwing more technology at the issue won’t solve it. Instead working to deeply understanding clinician challenges will drive solutions that account for clinician needs, provide clinician-centered data around improvement initiatives, and create partnerships with engaged clinicians.
An ideal setting for improvement work aligns and engages clinicians through ownership and shared accountability throughout the organization. Improvement leaders build this partnership with trust and transparency.
To support data- and analytics-driven improvement, organizations need a workforce dedicated to collecting, sharing, and using data efficiently. Three levels of improvement teams make this possible: a team to share information throughout the organization; an advanced analytics team responsible for predictive and prescriptive modeling; and a team to develop, support, and deploy improvement across the organization. These performance improvement teams have responsibilities across the system and the entire continuum of the organization, across clinical and business opportunities.
Health systems, however, still need to close the gap between improvement data and analytics and planning and the clinicians who will carry out changes on the frontlines. This is where clinician engagement strategies become critical.
Health systems can apply clinician engagement strategies at three strategic levels: local departmental or divisional (value-based performance), and leadership (department finance and planning sessions).
A program that engages clinicians in point improvements at the local level (e.g., the University of Kansas Health System Care Connections Program) establishes clinician partnerships in improvement work. Through Care Connections, the University of Kansas Health System provides foundational support for each improvement project with data, measurement, and analytics resources. The program has four main features that engage clinicians from the ground up:
Two arms make up the Care Connections Program: care advancement and care transformation:
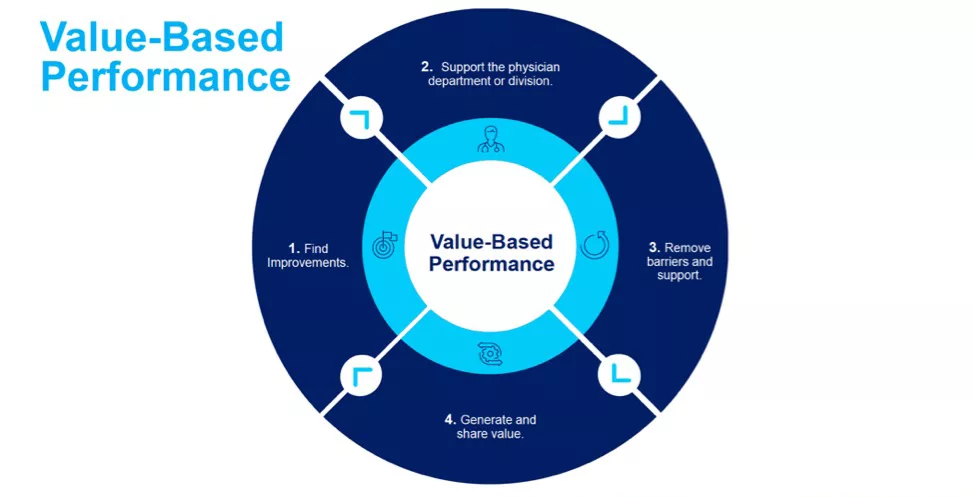
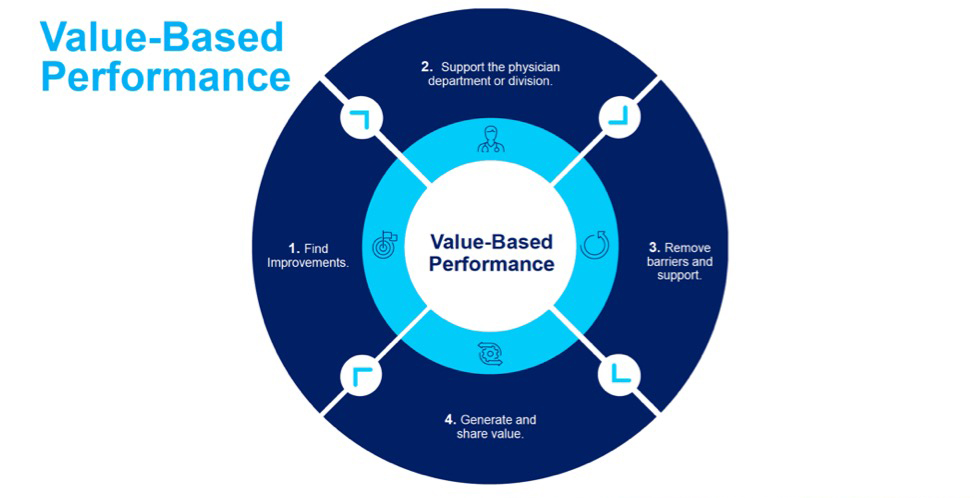
Value-based performance (Figure 1) engages clinicians at the divisional or departmental level (e.g., all pulmonologists or orthopedists) in line improvement. This level engages a group of clinicians to provide data to problem solve, present solutions, and measure and share financial gains with department on a quarterly basis in four steps:
The department planning and finance sessions engage senior clinician leaders in conversations about what to improve, why, and how. This level engages with multiple departments and specialties to discover how the health system delivers care as well as the quality of that care. At this engagement level, improvement teams produce information for clinicians on improvement work, hold office hours with analytics leadership and a planning meeting with senior leadership, and develop an annual improvement plan.
With clinicians making the vast majority of decisions that affect quality and cost, improvement efforts can’t succeed without their engagement. Health systems that create alignment with clinicians around improvement projects, rather than dictating to them, will build lasting partnerships to delivery high quality of care at lower costs.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.
Click Here to Download the Slides
https://www.slideshare.net/slideshow/embed_code/key/fEcV54NDtn4pJU