The operational military concept known as “left of bang” endorses continuous situational awareness to avoid harm proactively—before it occurs. Healthcare, however, operates reactively in response to patient harm, often intervening once a patient safety event has occurred, versus using practices and tools to recognize and respond to threats.
Applied to patient safety, a left-of-bang approach teaches frontline clinicians to increase sensitivity to and stay in constant vigilance for threats before they happen, moving down a scale of situational awareness levels:
1. White: Tending to the tasks at hand but largely unprepared for disruption and unaware of the conditions around them.
2. Yellow: Constantly understanding the safety vulnerabilities of day-to-day healthcare.
3. Orange: Ready to use the needed skills and tools to react to an event.
4. Red: Taking action and laser focused on the issue at hand.
 Download
Download

The current healthcare delivery system operates on a reactive framework, in which frontline caregivers and leaders respond to adverse events when and after the incident occurs. For example, patients may develop acute kidney injury (AKI) when care teams don’t preemptively identify threats associated with prolonged exposure to medications known to be toxic to the kidneys. Or a patient may get a pressure injury (PI) when clinicians don’t follow prevention guidelines. In both scenarios, care teams respond once harm has occurred, versus responding to early warning signs of risk.
But what if healthcare adopted a proactive framework, anticipating events and employing an appropriate mitigation strategy that optimized the relationship between data and technology and human decision making?
In a proactive scenario, the organization would use automated surveillance systems and methods to detect AKI and PI scenarios before patients experienced harm. Automated surveillance systems are constantly vigilant—analyzing data and providing situational awareness of pending risks. With active awareness, automated surveillance gives clinicians and their organizations analytics that focus their attention on threats before an injury occurs, enabling prevention or early mitigation while patients are receiving care.
Other high-risk, high-consequence occupations and practices—from the military to disaster management—operate on a proactive framework, as the consequences of a reactive approach would be devastating and sometimes lethal. An operational military concept known as “left of bang” emphasizes situational awareness before an event, or “bang,” occurs. In combat, bang can be an attack; in healthcare, bang can be any number of adverse events (e.g., hospital-acquired conditions [HACs]) that enhanced situational awareness can mitigate or prevent.
In their book “Left of Bang,” former active-duty Marine Corps officers and instructors, Patrick Van Horne and Jason Riley, describe methods for increasing sensitivity to and staying in constant vigilance to threats before they happen. Given the parallels between military and healthcare operations (life-and-death decision making, noisy and chaotic environments, and more), left-of-bang situational awareness offers a model for moving healthcare from a reactive to a proactive framework that supports better care and lower costs.
In both military and healthcare scenarios, the goal is to stay proactive and left of bang, as “right of bang” means the event has already occurred, leaving only reactive options to the resulting harm. In healthcare, relying on a reactive response is costly and carries significant clinical and operational downsides. Reaction doesn’t promote awareness or allow for intervention, mitigation, and prevention and can produce several negative outcomes, including diseases, harm events, clinician burnout and turnover, and more (Figure 1).

Healthcare relies on voluntary reporting, in which a team member recognizes and reports an adverse event, with either paper-based or electronic means, to another team member to investigate. With multiples steps (such as identifying and reporting the event before intervention), voluntary reporting is not only inefficient, but studies have shown it’s not accurate or comprehensive, detecting only about 14 percent of all-cause harm events.
Safety vulnerabilities and their resulting complications are ever present within healthcare settings, representing a significant burden on patients, clinicians, and health systems. Organizations vary in their ability to rapidly identify and intervene on such events. Timely recognition and appropriate intervention of patient conditions that represent clinical risk or early onset of preventable injury is essential for ensuring optimal patient safety in all care settings.
Approaching patient safety from the right (reactively) is as ineffective at recognizing early-warning signs as a driver looking at the windshield and rearview mirror at the same time—there are blind spots everywhere. To address blind spots, today’s automobiles have multiple safety systems that provide both active and passive safety monitoring—at least 10 active safety systems and six passive safety systems on board for many. Healthcare organizations must follow suit and adopt both active and passive safety systems to provide constant vigilance, mindfulness, and awareness of pending and existing patient safety threats.
Prone to the limitations of voluntary reporting, patient safety blind spots can result in overlooked harm events, reactive safety systems, and flawed data. Together, these factors raises the risk of procedural harm, workforce-related, and unrecognized harm.
Health care can overcome its safety blind spots with broader situational awareness. Left of Bang authors Horne and Riley use Jeff Cooper’s Awareness Color Code Chart to describe four levels of situational awareness or alertness: white (unaware); yellow (alert and aware but also calm and relaxed); orange (heightened awareness); and red (taking decisive and immediate action). The goal is a seamless transition between the levels.
Cooper’s color codes translate aptly to the healthcare setting:
An effective proactive healthcare delivery tool is a cloud-based module that monitors near real-time patient data from multiple sources and signals clinical attention when a patient is experiencing an adverse event or exposure to conditions that can lead to injury. The Patient Safety Monitor (PSM) Surveillance Module, for example, serves as central command for healthcare decision making.
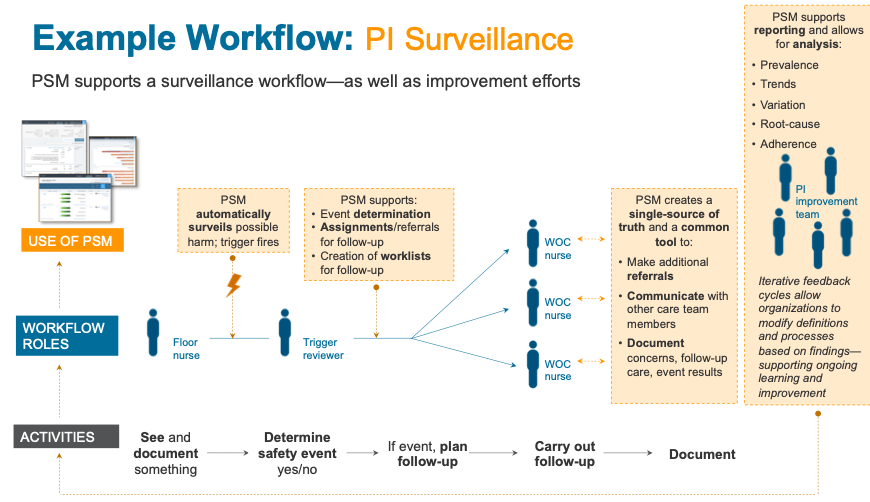
With safety monitors and triggers, the Surveillance Module enables remote patient surveillance (Figure 2). It detects injury at an early stage or when it’s about to happen, alerting care teams in time to intervene and prevent or mitigate harm. The model incorporates evidence-based guidance intervention into its actions based on different types of events, allowing teams to manage, mitigate, and prevent.
Safety measurement and monitoring that leverages a proactive, left-of-bang approach builds on and reinforces the five-dimensional safety framework outlined in 2015 a BMJ Quality & Safety paper. The publication aimed to provide a structure for determining whether a healthcare organization was safe:
Adopting and internalizing this framework for safety measurement and monitoring allows healthcare organizations to be in a constant state of yellow awareness (per Cooper’s color codes—psychologically alert, proactively prepared, and fully aware of day-to-day safety vulnerabilities.
For too many years, healthcare organizations have relied on reactive approaches to safety primarily driven by simple reliance on regulatory compliance of quality and safety measures. This reactive model has led to a false sense of safety and in fact, has not generally guaranteed a state of patient safety or the improvement of safety.
A proactive, left-of-bang healthcare alternative to voluntary reporting leverages electronic surveillance, comprehensive patient data, and pattern recognition (artificial intelligence/machine learning) to alert care teams when an event has occurred or is likely to occur. As a result, teams stay in constant vigilance.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.
Click Here to Download the Slides
https://www.slideshare.net/slideshow/embed_code/key/HuFLHbkuAx7bt2