When health system clinicians make care decisions based on their organization’s EHR data alone, they’re only using a small portion of patient health information. Additional data sources—such as health information exchanges (HIEs) and patient-generated and -reported data—round out the full picture of an individual’s health and healthcare needs. This comprehensive insight enables critical, and sometimes life-saving, treatment and health management choices.
To leverage the data from beyond the four walls of a health system and combine it with clinical, financial, and operational EHR data, organizations need an interoperable platform approach to health data. The Health Catalyst® Data Operating System (DOS™), for example, combines, manages, and leverages disparate forms of health data for a complete view of the patient and more accurate insights into the best care decisions.
 Download
Download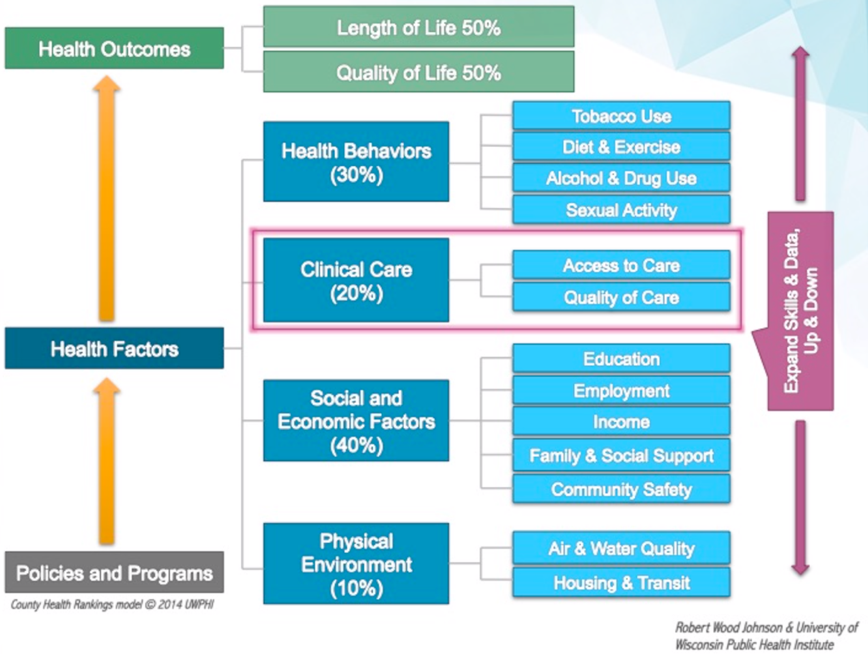
Health system-sponsored, regional and statewide health information exchanges (HIEs) have come a long way in giving healthcare providers vital patient information needed to achieve population health management (PHM) goals. Robust healthcare analytics that combine data from these HIEs with clinical, financial, and operational data from within the “four walls” of a health system with other forms of data, such as patient-generated health data (PGHD) and patient-reported outcomes (PROs), provide a more complete picture of a person’s state of health and healthcare needs.
This article explains how an interoperable platform approach to population health (e.g., the Health Catalyst® Data Operating System [DOS™]) combines, manages, and leverages HIE data, healthcare encounter data, and many other forms of data for a comprehensive view of patient and population health.
Back in 1998, my mother was diagnosed with ovarian cancer. Her symptoms were originally misdiagnosed as a gastrointestinal issue, but within a short period of time, she was (unfortunately) correctly diagnosed with stage 4 ovarian cancer. For the next seven years, my mom visited many healthcare providers of all types, within the acute and ambulatory care settings and spanning primary and specialty care providers (e.g., medical doctors, surgeons, physical therapists, naturopaths, pharmacists, home-health aides, and, ultimately, hospice).
During each visit and hospital stay, my mom had numerous procedures, lab tests, MRIs, and other scans, a multitude of medications, chemo-cocktails, radiation therapy, and a lot of love from a caring clinical community. Each of these encounters generated significant amounts of data. Due to the siloed nature of healthcare in the U.S., however, my mom’s caregivers had some data about her, but no one provider had all the data about her.
As a healthcare IT professional, I remember being extremely frustrated because we had to explain, and reexplain, my mom’s medical history to each new provider. No one clinician could provide optimal care because they didn’t have a complete picture of my mom. It was like trying to put together a jigsaw puzzle with a bunch of pieces missing.
Each provider knew what they did for her but rarely knew what other providers were doing and had done previously. The result was increased costs, duplication of tests and procedures, unwarranted variation in what/how care was delivered, and an overly complicated and disjointed patient experience.
My mom passed away in 2005, which was before the advent of HIEs born just a few years later as a byproduct of the 2009 HITECH Act. While each provider had their own data about my mom, without HIE data and robust analytics, each provider across the various care settings acted and made decisions about her treatment based on incomplete information. If every caregiver had access to all of her encounter data, the opportunity to deliver higher-quality, safer, and lower-cost care would have dramatically improved.
If we apply my mom’s patient experience across thousands, or millions, of people in an ACO or value-based care arrangement; in a geography, state, or across the U.S., the opportunity for adverse quality, safety, and cost outcomes multiplies almost exponentially. In fact, trying to manage the health and healthcare of individuals and populations without complete information is like Russian roulette—threatening, dangerous, and unpredictable.
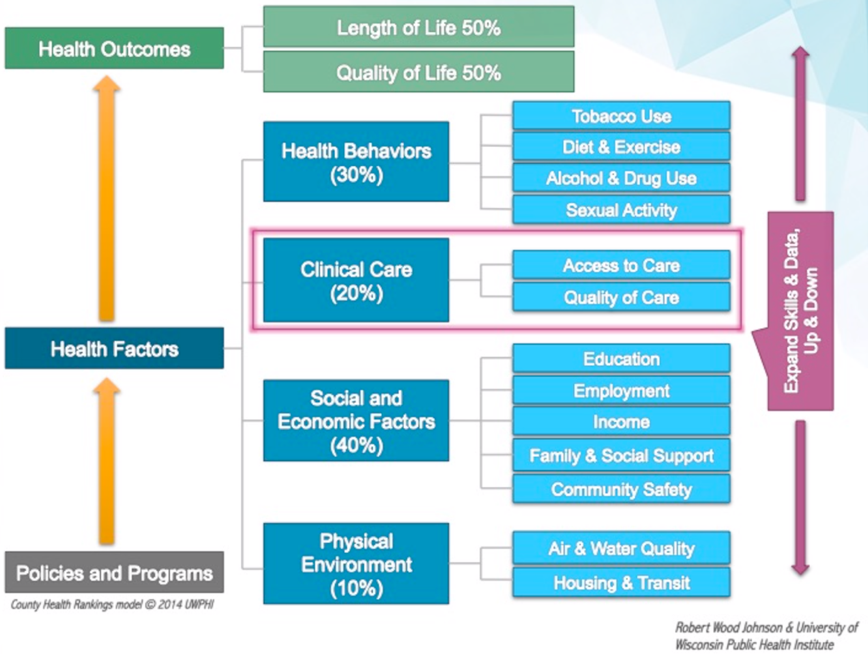
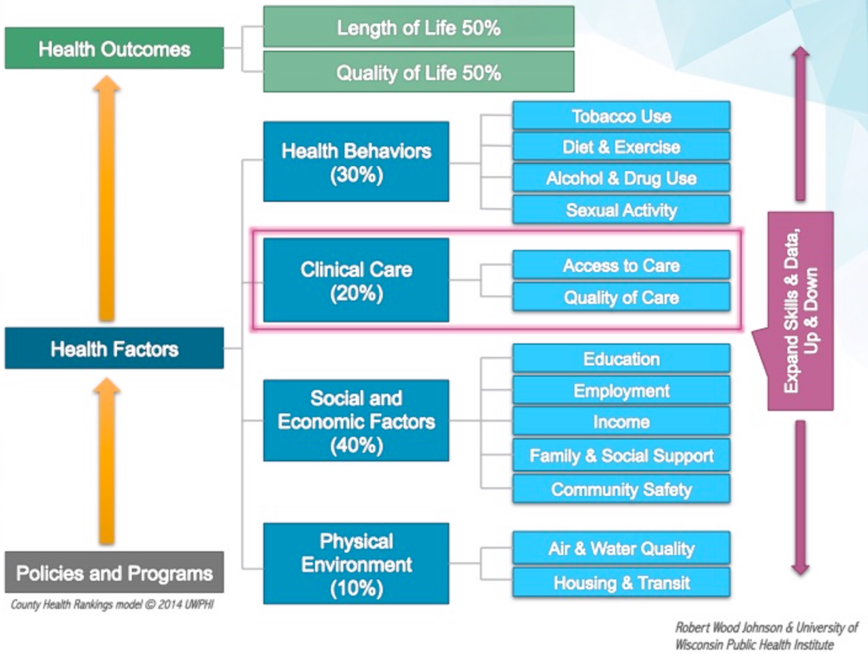
Adding to the complexity, 80 percent of the information that describes a person’s health status (Figure 1), and is essential for managing population health, is determined by factors outside a traditional care setting (e.g., socioeconomic factors). This information comes in a variety of structured and unstructured data types and resides in anything from enterprise systems to consumer devices. This data spans clinical, financial and operational realms and includes PGHDs, PROs, and social determinants of health. EHRs will always be incomplete data sources, and while HIEs are closer, a DOS-like platform approach offers the most comprehensive picture of patient health.
To maximize the value of comprehensive patient data, health systems and HIEs need a platform approach to managing data—one that is open, interoperable, scalable, and can apply intelligence to the data at whatever velocity it comes in, whether the data is structured or unstructured.
Consider an everyday example: an iPhone comes with the iOS mobile operating system, which has numerous native capabilities (e.g., GPS, cellular or Wi-Fi connectivity, a camera, biometric security, a compass, a clock, etc.). iOS is interoperable with other platforms, such as Android, and is an open application development platform. I have more than 200 apps on my phone from different software companies, all of which leverage the native iOS capabilities. For example, when I travel, I use Apple maps for navigation, Waze for monitoring traffic, and Citymapper for getting around unfamiliar cities in Europe.
All three of these apps leverage the native GPS that comes with iOS via open APIs (application programming interfaces), so each app developer doesn’t need to reinvent the GPS wheel. My iPhone also integrates data from my Apple Watch, recording figures such as heart rate, sleep patterns, and physical activity; these all interoperate with my other exercise apps (e.g., Strava). These apps provide all sorts of analytics, suggestions, and predictions, which help me stay healthy and fit.
Following the iOS interoperability model, as an interoperable analytics platform, Health Catalyst’s DOS delivers the comprehensive health system and HIE data that care teams need to fully understand a patient’s situation and make the most informed treatment decisions. HIE data feeds into the DOS platform, capturing patient information along the continuum of care, from primary care physicians and specialists to labs, skilled nursing facilities, visiting nurses, and emergency departments.
Now, imagine if hospitals and health systems took a platform approach to managing data and analytics at an enterprise scale and were able to integrate and interoperate with data from across the healthcare continuum, as well as integrate and interoperate with the 80 percent of health determinants not found in a clinical care setting. Like the iOS or Android operating systems, a healthcare data and analytics platform includes critical capabilities:
If a healthcare analytics platform like DOS had been in place when my mom was in treatment, her healthcare providers and I would have had a comprehensive view of her health. This view would include not only the myriad data from her hospital and clinic visits, but other forms of data from beyond the clinical care setting (e.g., diet, exercise, and lifestyle).
This data would be “liquid” and easily exchanged with everyone on my mom’s care team—and with the rest of my family, allowing us to be proactive (versus reactive) in managing her care. She could have avoided the numerous repeated and duplicative tests and procedures, and her care would be better coordinated. I wouldn’t have had to be a “human DOS,” lugging boxes of her medical records to each doctor visit. All members of her care team could communicate openly and securely, putting my mom at the center of the focus, rather than each individual encounter. My mom and I would be able to interact with the care team in real time, via voice, text, and video, reducing the number of onsite visits to hospitals and clinics (these visits were exhausting, costly, and time consuming for all of us, especially my mom).
She would have been able to use a multitude of apps to more effectively manage her care and treatments. Her data, combined with research and genomics data, could have helped to align her with a clinical trial quickly, bringing the best of modern medicine to the forefront of her care.
If we think about a broader population than just my mom, and if we had more data than that found just within the four walls of the hospital or health system, we could proactively identify people at risk for contracting illness well in advance of the person becoming sick. We could move from today’s world of managing illness to managing health and wellness and keeping people out of the hospital. Quite literally, an intelligent and interoperable healthcare data operating system could possibly have saved my mom’s life.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.
Click Here to Download the Slides
https://www.slideshare.net/slideshow/embed_code/key/ooGmgrHkTUaKAi