A series of revolutions has driven the development of the U.S. healthcare system, enabling dramatic improvements in all aspects of healthcare quality and outcomes over the past century. Although healthcare organizations have focused on moving towards value-based care for decades, the data shows that the shift is indeed taking place and fee-for-service models are declining.
New changes to the Medicare Shared Savings Program (MSSP) will help drive this change as revisions to MSSP require ACOs to take on more financial risk earlier. This article covers the following topics:
1. Important moments in history that led to today’s current challenges.
2. Why financial imperatives drive cultural change in our economic model.3. Ways MSSP can help healthcare organizations achieve financial success.
4. How to utilize data to develop better healthcare delivery systems.

This article is based on a 2019 webinar given by Will Caldwell, MD, MBA, Senior Vice President at Health Catalyst, entitled, “The Next Revolution in Healthcare: Why the New MSSP Revisions Matter Now More Than Ever.”
Data is the catalyst for healthcare’s next revolution. Today’s healthcare providers and administrators have an incredible opportunity to participate in what may be the biggest societal shift of a lifetime: the move from a fee-for-service (FFS) payer model to value-based care (VBC). Effectively using data will facilitate that shift.
On December 21, 2018, CMS issued a final rule for the Medicare Shared Savings Program (MSSP), strengthening the financial incentives for ACOs to drive improved outcomes. The health systems that embrace data to achieve financial success will grow while others will struggle to compete.This article explores the high points in history that have led to the current challenges, why financial imperatives drive cultural change in our economic model, ways MSSP can help healthcare organizations achieve financial success, and ideas for how to utilize data to develop better healthcare delivery systems.
A series of revolutions has driven the development of the U.S. healthcare system, enabling dramatic improvements in all aspects of healthcare quality and outcomes over the past century. These include the following:
In the early 1900s, the industrial revolution led to financial gains and a tax base that allowed the government to create hospitals, medical schools, and educational institutions. As a result, public health began to improve as child mortality rates decreased.
Between 1900 and 1930, insights such as the Flexner Report, which looked at the quality of care provided and the quality of training physicians received, spurred a quality revolution in healthcare. As a result of the Flexner Report, almost half of all medical schools and hospitals across the country were shuttered, and processes were put in place that granted states the right to license hospitals and medical schools. These changes prompted further reductions in child mortality rates.
In 1948, two developments again moved the needle on child mortality rates, from 20 to 30 percent down to two to four percent: the advent of food pasteurization and the creation of sanitary sewer systems. Neither of these developments are what people typically think of as healthcare, but they drove the largest reduction in child mortality of any other public health efforts. Tax dollars facilitated many of these improvements, spurred by governmental regulations, rather than private individuals or companies.
These revolutions have raised the bar for healthcare quality to where there’s no question that the system is far better today than in 1900. But, looking at the Gini coefficient, inequality is growing and there’s more work to do. The question is, “What’s the next revolution?” Many experts predict that the U.S. healthcare system is headed for a payer model revolution that will help move the needle from a FFS to a VBC model to create scalable, sustainable improvements in patient outcomes. Profitability in a market economy, should be viewed not just as a result of improvement efforts, but also a mechanism to achieve success and drive sustainable outcomes.
As pressures mount for healthcare organizations to shift to VBC, it’s important to keep in mind that there’s a spectrum between a FFS model and a VBC model and that value can have different meanings in different systems. Value can mean the following:
While value can have many meanings, data management is central to any definition of value. What’s important is that healthcare systems understand where they are on the spectrum between FFS and VBC and know where they want to be five years from now.
Although healthcare organizations have focused on moving towards VBC for decades, the data shows that the shift is indeed taking place and FFS models are declining. According to the Health Care Payment Learning and Action Network, “The percentage of total healthcare payments linked to a value-based payment model (shared savings, shared risk, bundled payments, population-based payments) reached 34% of total dollars paid to providers in 2017, up 23% from 2015.” Additionally, the data shows that the shift to value is indeed real: the proportion of businesses aligned with FFS models is in decline from 51.7 percent in 2016 to 25.4 percent projected in 2021.
The move to value is working, and healthcare payers are following suit:
Medicare saw a reduction in utilization by over a billion dollars in 2018 and showed additional promising signs, including the following:
Clif Gaus, president and CEO of the National Association of ACOs, said of these statistics, “The recent results show that ACOs have turned the corner and this evidence dispels confusion about ACO performance. The hard work of ACOs is paying off for patients, providers, and for the Medicare trust fund.” And, according to CMS, the number of Medicare advantage plan choices will increase 20 percent in 2019 to more than 3,700 options in the marketplace—another sign that value-based models are here to stay.
MSSP is an alternative payment model created following the passage of the Affordable Care Act (ACA) of 2010 and was revised in late 2018. The model rewards providers and hospitals for achieving quality metrics and lowering healthcare expenditures. Revisions to MSSP require ACOs to take on more financial risk earlier, potentially incurring fees if organizations don’t realize quality metrics and cost savings and indicating an important cultural shift that will help move the needle from FFS to VBC.
By 2022, CMS estimates that 40 percent of all covered lives in the U.S. healthcare system will be part of either Medicare or Medicaid. With revisions to MSSP, Medicaid programs across the country are following suit and adopting similar payment methodologies, asking hospitals and providers to take on more financial risk, improve the health of populations, and decrease healthcare costs.
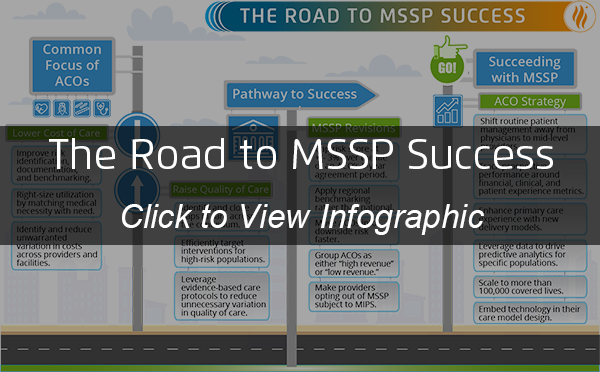
Common focuses for the management of VBC delivery include both raising the quality of care and lowering the total costs of care. In raising quality of care, ACOs must achieve the following:
In lowering the cost of care, ACOs must achieve the following:
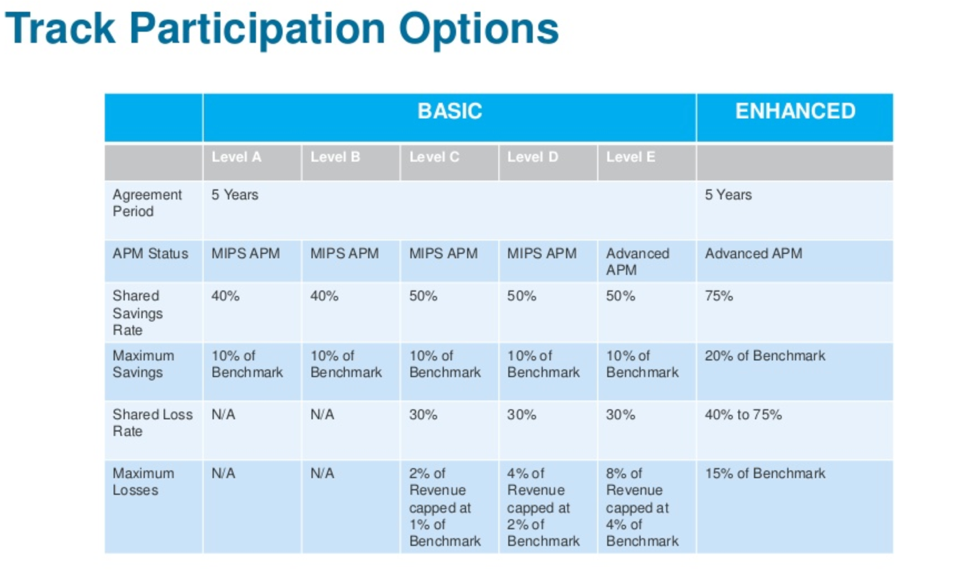
Revisions to Medicare Shared Savings Program (“Pathways to Success”) encourages ACOs to transition to performance-based risk more quickly and to incrementally increase savings. The revisions cover several important highlights:
With more financial risk at stake, ACOs need to plan for success. To do so, ACOs will need the following strategy:
Simply having the right technology, while a key component to success in a shared savings model, doesn’t necessarily drive adoption or success, making it critical that ACOs embed technology within the care model design. Healthcare systems reluctant to move away from a FFS model should keep in mind a few key points:
The ACA and other regulatory changes have encouraged health systems to digitize healthcare, but these changes have had mixed success. While EMR adoption is high, the push for digitization has also created cynicism among providers who think of technology as a box-checking exercise. EMRs are necessary, transactional tools that do the job they were designed for. As health systems adopt smarter tools that can use data to transform care and affect real change, this cynicism may turn to excitement at the possibility of driving important changes in the healthcare landscape.
Amid both new and evolving regulatory requirements, it’s an exciting time at the front lines of care. Changes to MSSP that require more financial risk earlier are the beginning of an important cultural shift. And, because other payers and Medicaid programs are following suit, this could be the financial push needed to move the U.S. healthcare system away from FFS and finally tip the balance to VBC. Providers and administrators that embrace these changes and help usher them forward can make a scalable difference that impacts the lives of countless people.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.