The healthcare industry is currently obsessed with outcome measures — and for good reason. But tracking outcome measures alone is insufficient to reach the goals of better quality and reduced costs.
Instead, health systems must get more granular with their data by tracking process measures. Process measures make it possible to identify the root cause of a health system’s failures.
They’re the checklists of systematically guaranteeing that the right care will be delivered to every patient, every time. By using these checklists, organizations will be able to improve quality and cost by reducing the amount of variation in care delivery.
 Download
Download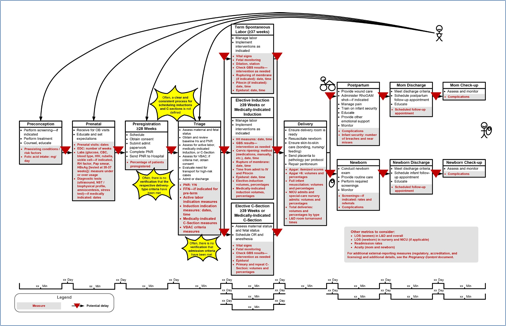
Health systems today are scrambling to identify the most important measurements they can use to generate stable, consistent growth. A friend of mine loves to hike and was telling me about a fancy one-legged stool he carries around with him. He explained that he only really needs one leg; packing three-legged stools causes extra weight. While this mentality might work for time spent on the trail, it doesn’t hold up when it comes to measuring healthcare outcomes—I’d choose the balanced stability offered by the three-legged variety any day.
Similarly, healthcare systems shouldn’t rely on the single “leg” of outcomes measures to improve quality and costs, even though these metrics are plentiful. In addition, we must create a solid foundation of evidence-based process measures that provide more granular data, and then stabilize these metrics with balance measures, to help drive better outcomes.
What exactly are evidence-based process measures? First it helps to understand the three types of measures we use in healthcare analytics:
Process measures are the evidence-based best practices that represent a health system’s efforts to systematize its improvement efforts. To illustrate this, I’ll use a patient injury prevention example. Let’s say your organization needs to reduce the incidence of pressure ulcers commonly known as bed sores. That is your outcome measure. You know your baseline rate, and you want to reduce it, but how are you actually going to drive improvement?
The answer is straightforward: by implementing and tracking the right process metrics. Process measures in this example are the steps that should be performed every time for every bed-bound patient in the intensive care unit (ICU) or in the med-surg unit. The first and most important process measure would be performing a risk assessment using the Braden Scale for predicting pressure ulcer risk on all the appropriate units in the hospital.
Patients identified as “at risk” would then receive treatment for preventing bedsores according to your organization’s chosen best-practice protocol. For example, you might set up protocols for reassessment, nutrition, lifting and repositioning the patient, providing a special mattress, and skin care. The important thing is that each of these steps in the process can be can be tracked and measured. Over time, as you develop an adequate sample size, you can begin to identify which process steps are the most important for preventing negative outcomes.
One of the greatest benefits of having this process metric data on hand is the ability to identify what is really causing the problem with pressure ulcers in your organization. I can assure you that the problem does not stem from your people. It stems from your process. In most organizations, however, the system of incident reporting doesn’t recognize this fact. There is a stigma attached to filling out the report: “You failed. You’re a bad nurse because your patient got a bed sore.” Often, many borderline cases go unreported because of the lack of a culture based on a learning environment and too much focus on outcomes metrics.
Really, it is the process that failed, not the person. One of my favorite quotes is from Paul Batalden, MD, and it goes like this: “Every system is perfectly designed to get the results it gets.” If you don’t have a well-designed process in place to prevent pressure ulcers, it should be no surprise if you don’t perform well on that outcome metric.
By tracking process measures, you can pinpoint the root cause of the system’s failure. You might find that you have a shortage of pressure-redistributing mattresses in the supply room, or that you didn’t do a risk assessment for every patient who arrived on the unit, or that the right skincare products aren’t accessible on the floor when needed. Whatever the problem, you can then assess it and fix it.
What you’re trying to do is move from a craftsmanship mentality to a system of production. And process metrics are the way that you do that. They’re the checklists to systematically guarantee that the right care will be delivered to every patient, every time.
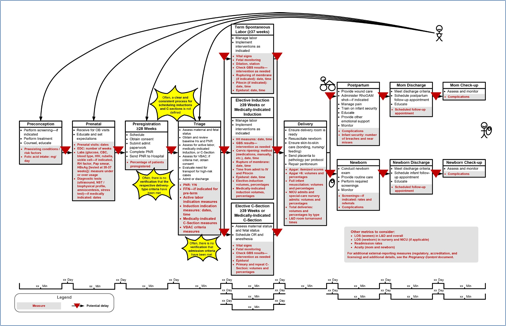
Process measures improve quality and cost by enabling organizations to reduce the amount of variation in care delivery. When you establish process metrics at potential points of variation in a care process, you can monitor and reduce inappropriate variation. A value stream map is a great tool to outline a care process and identify potential points of variation that can be measured.
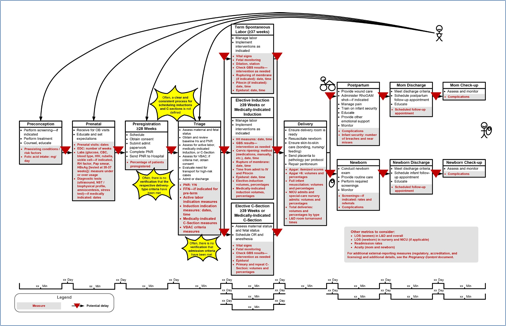
A value-stream map outlines the steps in a process that deliver value to a patient. Each of those steps may have a process measure useful in measuring process consistency. By measuring these steps, you can discover points of variation. For example, you might discover that one step in the process takes some units one hour to complete and other units five hours. Or it might cost some units $2,000 and other units $8,000. Those instances of variation provide opportunities to explore the data to understand why the variation exists. From there, it’s possible to standardize processes so that all patients consistently receive the highest-quality care at the lowest possible cost regardless of which unit, which hospital, or which clinic they are visiting.
So why don’t more healthcare organizations have these kinds of systems in place? The answer is that they don’t have the infrastructure to handle outcome, process, and balance metrics. If they only have the resources to track one of these, they’ll choose outcome metrics, because those are the measures that must be submitted to CMS.
The reason organizations struggle to track all types of measures is because their analytics methodologies rely too much on manual work. When you don’t have the right technology infrastructure in place to automate the extraction and distribution of data, you end up having to do it all manually. You might be able to successfully use manual methods to track improvement for one process or even two, but once you get to the third, fourth, or fifth process, the manual work becomes unsustainable. And without continuous measurement, you won’t be able to sustain the gains you made in one process once you move on to the next.
That’s where an enterprise data warehouse (EDW) with a robust and flexible analytics architecture comes in. An EDW forms the foundation for healthcare analytics by bringing all of a health system’s data into a single source of organizational truth. This makes it possible to eliminate the manual process of gathering data and instead, delivers the automation you need to track a wide variety of outcome, process, and balance measures simultaneously. With an EDW, analysts can then focus their time on discovering patterns in the data that will lead to understanding, insight, and ultimately action. But without an EDW, it will be very difficult for analysts to provide reliable and repeatable reports and in-depth analyses of areas that will reveal the best opportunities for improving outcomes.
Traditional data warehousing, which solved some of the data integration issues facing healthcare organizations, is no longer good enough. As Gartner reported, traditional data warehousing will be outdated and replaced by new architectures by the end of 2018. And current applications are no longer sufficient to manage these burgeoning healthcare issues. The technology is now available to change the digital trajectory of healthcare.
The Health Catalyst Data Operating System (DOS™) is a breakthrough engineering approach that combines the features of data warehousing, clinical data repositories, and health information exchanges in a single, common-sense technology platform.
DOS offers the ideal type of analytics platform for healthcare because of its flexibility. DOS is a vendor-agnostic digital backbone for healthcare. The future of healthcare will be centered around the broad and more effective use of data from any source. Clinical and financial decision support at the point of care is almost nonexistent in healthcare, restricted to a few pioneering organizations that can afford the engineering and informatics staff to implement and maintain it. With DOS, this kind of decision support is affordable and effective, raising the value of existing electronic health records and making new software applications possible.
Would you like to use or share these concepts? Download this presentation highlighting the key main points.
Click Here to Download the Slides
https://www.slideshare.net/slideshow/embed_code/42485462