In 2021, CMS proposes the following four key changes to the Quality Payment Program (QPP) that will impact quality measurement for ACOs and ACO participants:
1. The discontinuation of the CMS Web Interface.
2. The introduction of the alternative payment model (APM) Performance Pathway (APP).
3. The discontinuation of the APM scoring card.
4. The addition of the APM entity as a submitter type for MIPS.
Each change will create new challenges for ACOs and ACO participants. Organizations can successfully navigate these shifts by partnering with a robust quality measures solution that creates a complete picture by combining comprehensive data and measures information in performance visualizations. An inclusive quality measures solution also creates a thorough workflow by combining the monitoring and improving processes, then submitting performance to payers.
 Download
Download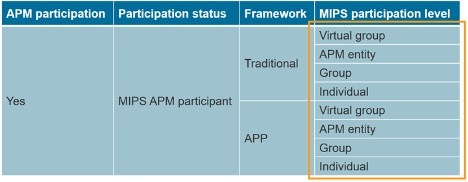
This guide explains four key changes CMS made to the Quality Payment Program (QPP). These four changes come from the 2021 QPP Final Rule and create eight new challenges in quality measurement for either 1) ACOs in the Medicare Shared Savings Program (MSSP) or 2) ACO participants still required to participate in the Merit-based Incentive Payment System (MIPS).
This guide details the four key changes from the 2021 QPP Final Rule, the eight challenges created by those changes, and Health Catalyst solutions to those challenges.
Four key changes in the 2021 QPP Final Rule simultaneously affect MSSP ACOs and MIPS APM participants: 1) discontinuation of the CMS Web Interface, 2) introduction of the APM Performance Pathway (APP), 3) discontinuation of the APM scoring standard, and 4) the addition of the APM entity as a submitter type for MIPS. This section explains each of the key changes but does not yet discuss the challenges created by those changes.
CMS announced that it would discontinue the CMS Web Interface starting in 2022. The CMS Web Interface is a submission method CMS offers for quality measurement in the MSSP and MIPS programs.
ACOs report MSSP quality data to Medicare using the CMS Web Interface. Additionally, over 100 groups report MIPS quality data to Medicare through the CMS Web Interface. However, these ACOs and groups can no longer use the CMS Web Interface to report quality data to Medicare starting in the 2022 performance year.
CMS introduced the APM Performance Pathway (APP) in the 2021 QPP Final Rule. The APP is a new reporting framework for ACOs and MIPS APM participants. (Note: CMS uses the term “reporting framework” to refer to a unique set of measures/activities and scoring.) The APP reporting framework includes the same set of quality measures for ACOs and MIPS APM participants. However, the APP reporting framework defines additional requirements for each MIPS category for MIPS APM participants.
The APP for ACOs
ACOs that fulfill the APP fulfill their requirements in the Medicare Shared Savings Program (MSSP). The APP is now the required reporting framework for ACOs participating in the MSSP. In other words, CMS no longer measures ACO quality performance using the 23 former quality measures.
Below are two tables listing the measures and activities for the APP for ACOs. Notice that the list of self-reported measures differs in each table based on the submission method, meaning eCQMs/CQMs (Table 1) versus the CMS Web Interface (Table 2). ACOs submit the list of measures that corresponds to their chosen submission method. However, remember that the CMS Web Interface is discontinued starting in the 2022 performance year.
The APP for MIPS APM Participants
MIPS APM participants that fulfill the APP fulfill their requirements in the MIPS program. MIPS APM participants can submit the APP as a group or as an individual independent of their APM entity (e.g.,, ACO). Unlike the APP for MSSP ACOs, the APP is an optional reporting framework for MIPS APM participants. It is not a required reporting framework.
For MIPS APM participants, the APP is similar to a MIPS Value Pathway (MVP). That’s because, like MVPs, the APP is a prepackaged set of measures and activities. However, the APP differs from an MVP because it is limited to only MIPS APM participants. MIPS participants that are not MIPS APM participants cannot submit the APP.
Below are two tables that list the measures and activities for the APP for MIPS APM participants. Like the APP for ACOs, notice that the list of self-reported quality measures differs in each table based on the submission method, meaning eCQMs/CQMs versus the CMS Web Interface. MIPS APM participants submit the list of measures that correspond to their chosen submission method. However, remember that the CMS Web Interface is discontinued starting in the 2022 performance year. And unlike the APP for ACOs, notice that the APP for MIPS APM participants defines requirements for all four MIPS categories.
In the APP for MIPS APM participants, notice that CMS defers to APM requirements for both the Improvement Activities (IA) and Cost categories. Specifically, CMS credits participants 100 percent of the IA category score in MIPS 2021 because MIPS APM participants fulfill improvement activities as part of their APM participation. Conversely, CMS weights the Cost category score to 0 percent because CMS wants MIPS APM participants to focus on their cost containment efforts in APMs. And that’s why CMS does not include any measures or scoring in the Cost category in the APP.
CMS discontinued the APM scoring standard in the 2021 QPP Final Rule. The APM scoring standard only applied to the MIPS program, not the MSSP. However, it applied to MIPS APM participants, including but not limited to MIPS eligible clinicians participating in MSSP ACOs.
The APM scoring standard required that CMS only use a MIPS APM participant’s APM entity score to apply that participant’s MIPS payment adjustments. In other words, CMS used a MIPS APM participant’s APM entity MIPS score even if the participant had other final MIPS scores such as group or individual. Even if a clinician’s group or individual score was higher than a clinician’s APM entity score, CMS still used the APM entity score to apply MIPS payment adjustments.
Specifically, the APM scoring standard dictated the former MIPS scoring hierarchy. The MIPS scoring hierarchy identifies which final clinician MIPS score CMS would use to apply MIPS payment adjustments for a clinician. The MIPS scoring hierarchy is necessary because clinicians can have multiple final MIPS scores. When a MIPS APM participant had multiple final MIPS scores, CMS only used the APM entity score. That’s because the former APM scoring standard dictated the prioritization of APM entity scores in the MIPS scoring hierarchy.
Table 5 below illustrates the former MIPS scoring hierarchy. Notice that it prioritizes APM entity scores above other participation levels, meaning virtual group, group, and individual.
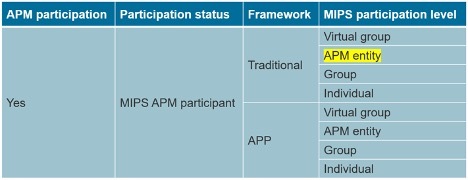
CMS revised the MIPS scoring hierarchy due to the discontinuation of the APM scoring standard (Table 6). Notice that CMS no longer prioritizes APM entity scores above other final scores.
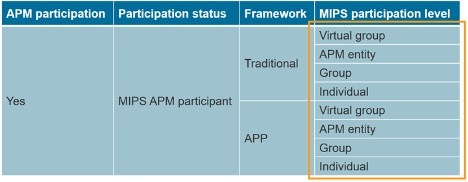
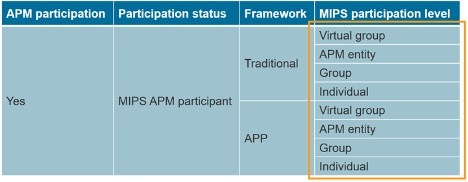
CMS now uses the highest final MIPS score for a participant when applying MIPS payment adjustments (except for virtual group scores which CMS must still use over all other scores). For MIPS APM participants that can have up to eight final scores (Figure 1), CMS will prioritize the use of a virtual group score if one exists. Otherwise, CMS will use the highest final score at any participation level in either the APP or traditional MIPS reporting framework.
CMS added APM entities to the list of MIPS submitter types in the 2021 QPP Final Rule. CMS defines submitter types as “individual clinicians submitting for themselves, or someone authorized to submit data on behalf of a clinician or practice” (CMS, QPP Website). As a submitter type, APM entities (e.g., ACOs) can now submit traditional MIPS on behalf of MIPS eligible clinicians participating in the APM entity (e.g., ACO participants).
CMS specifically summarized the change this way: “The APM entity will be able to report on the Quality and Improvement Activities performance categories. Quality measures will be selected and reported in the same manner and using the same options that are available to all other MIPS eligible clinicians or could be reported through the APP” (CMS, 2021 QPP Final Rule Overview Fact Sheet, p. 4).
CMS will use the APM entity MIPS submissions to create a traditional MIPS score for MIPS APM participants at the APM entity level (Figure 2).
The four changes create challenges for either MSSP ACOs or MIPS APM participants, or both. Some challenges are good challenges, but most are not. Some of the changes create one challenge and some of the changes create more than one challenge, such as the discontinuation of the CMS Web Interface.
The discontinuation of the CMS Web Interface creates four new challenges for MSSP ACOs and MIPS participants that previously used the CMS Web Interface to report for MIPS. First, MSSP ACOs and MIPS participants must evaluate and implement a new submission method as soon as possible. Second, MSSP ACOs and MIPS participants that previously used the CMS Web Interface must make care delivery changes. Third, MSSP ACOs and MIPS participants must make data collection changes. Fourth, MSSP ACOs and MIPS participants must determine how different benchmarks in other submission methods affect their quality measure scores.
Challenge #1: Submission Method Change
ACOs that previously used the CMS Web Interface to submit their MSSP quality performance must switch to a different submission method (aka “collection type”). Also, groups of MIPS participants that previously used the CMS Web Interface to submit their MIPS quality performance must switch to a different submission method. The remaining submission methods applicable to these ACOs and groups include the following: electronic clinical quality measures (eCQMs), clinical quality measures (CQMs), and qualified clinical data registry (QCDR) measures.
ACOs and groups should carefully evaluate the list of quality measures in each submission method to ensure they select measures that match their specialty and strengths. Whether ACOs and groups report the APP or traditional MIPS, alternative submission methods differ from the CMS Web Interface in significant ways. Those differences create three subsequent challenges for ACOs and groups when transitioning from the CMS Web Interface to an alternative submission method. Those three challenges are the remaining challenges in this list related to the discontinuation of the CMS Web Interface.
Challenge #2: Care Delivery Changes
MSSP ACOs and groups of MIPS participants may need to make care delivery changes when switching to an alternative submission method for two reasons. First, alternative submission methods measure quality for all patients, not just a sample of Medicare patients. Second, ACOs and groups may need to make care delivery changes if reporting traditional MIPS using measures that do not match measures in the CMS Web Interface.
Challenge #3: Data Collection Changes
New submission methods may require MSSP ACOs and groups of MIPS participants to make data collection changes for two reasons. First, the measurement of quality on all patients may require data collection changes. Second, the different value sets used in the different submission methods may require data collection changes.
Challenge #4: Scoring Changes
Performance rates vary for the same measure across different submission methods. Consequently, CMS creates different benchmarks for each submission method. CMS likely created different benchmarks to ensure that one submission method does not create a competitive advantage over another. However, the different benchmarks create uncertainty when transitioning from one submission method to another.
The quality score for ACOs and groups could increase or decrease due to the transition from the CMS Web Interface to alternative submission methods. That’s because the same performance rate for the same measure can be worth more or fewer points in the different submission methods. Consequently, ACOs and groups should be cognizant of the different benchmarks in different submission methods for the same quality measure.
For example, notice that providers with a 31 percent performance in the diabetes measure would earn different scores in the different submission methods (Table 7). Specifically, providers with a 31 percent performance earn between 7.0-7.9 points in the eCQM submission method versus 10.0 points in the CQM submission method. A 31 percent performance would have earned 7.0-7.9 points in the CMS Web Interface using MIPS scoring.
As another example, notice that providers with a 99 percent performance in the flu shot measure would earn different scores in the different submission methods (Table 8). Specifically, providers with a 99 percent performance earn between 9.0-9.9 points in the eCQM submission method versus 7.0 to 7.9 points in the CQM submission method. A 99 percent performance would have earned 10 points in the CMS Web Interface using MIPS scoring.
The two examples above demonstrate how the same performance rate for the same measure can be worth more or fewer points in different submission methods. Consequently, ACOs and groups should be cognizant of the different benchmarks in the different submission methods for the same quality measure.
The introduction of the APM Performance Pathway (APP) creates two key challenges. First, the APP will decrease quality performance scores for MSSP ACOs. Second, a decrease in ACO quality scores will decrease the APM entity MIPS scores for MIPS APM participants.
Challenge #5: The APP Decreases Quality Performance Scores for MSSP ACOs
CMS aligned the APP with the MIPS quality scoring methodology to create one scoring methodology for both the MSSP and MIPS. However, CMS estimated that the “proposed methodological changes in ACO quality scoring will reduce the mean ACO quality score by roughly 10 to 15 percentage points relative to recent historical performance years where ACO quality performance scores have averaged 90 percent or more” (CMS, 2021 QPP Proposed Rule, p. 913). CMS did not specifically identify which scoring changes will cause the decrease in ACO quality scores. However, significant changes include the decrease of quality measures from 23 to 6, the emphasis on outcome measures, and the MIPS scoring methodology.
Challenge #6: The APP Decreases the APM Entity MIPS Scores for MIPS APM Participants
MIPS APM participants receive a MIPS score based on the performance of their ACO (referred to as an “APM entity” in MIPS). The performance of the ACO is referred to as the participant’s APM entity score in MIPS. In previous years, MIPS APM participants benefited from high APM entity MIPS scores. However, as noted in the previous section, CMS projects a 10-15 percent decrease to ACO quality performance. That decrease in ACO quality performance will decrease the APM entity MIPS scores credited to MIPS APM participants.
Due to the discontinuation of the APM scoring standard, clinicians classified as MIPS APM participants could have up to eight final MIPS scores when a participant has multiple MIPS submissions. MIPS APM participants must now determine which MIPS reporting framework (whether APP or traditional MIPS) and which level of MIPS participation (APM entity, group, and individual) would put forward their best MIPS score.
Due to the addition of the APM entity as a MIPS submitter type, APM entities can, but do not have to, submit traditional MIPS quality measures. Consequently, APM entities must determine whether they will submit traditional MIPS quality measures on behalf of the MIPS eligible clinicians that participate in the APM entity. For example, ACOs must determine whether they will submit traditional MIPS quality measures on behalf of MIPS eligible ACO participants. Alternatively, ACO participants could pressure ACOs to submit traditional MIPS quality measures if ACO participants believe that the APM entity MIPS score would be higher with those measures. Additionally, health systems that manage an ACO and employ participants in the ACO must determine whether submitting traditional MIPS quality measures could increase the APM entity MIPS score and, therefore, increase the MIPS payment adjustment for the system’s employed providers.
The Health Catalyst quality measures solution overcomes each of the challenges created by the four key changes affecting MSSP ACOs and MIPS APM participants (and groups that previously submitted quality data using the CMS Web Interface). Specifically, the Health Catalyst quality measures solution creates a complete picture by combining complete data from a complete list of data sources, complete measures from a complete list of programs, and complete performance visualizations. The Health Catalyst quality measures solution also creates a complete workflow by combining the process for monitoring, improving, and submitting performance to payers.
The rest of the guide explains how specific components within the Health Catalyst quality measures solution solve specific challenges facing ACOs and MIPS APM participants in the 2021 QPP Final Rule.
The Health Catalyst quality measures solution overcomes all the challenges created by the discontinuation of the CMS Web Interface. Those challenges include the following:
Submission Method Changes
The Health Catalyst quality measures solution offers clinical quality measure (CQM) submission through its submission engine and qualified registry (the Able Health Qualified Registry). Quality teams can measure and submit their performance directly to CMS from within the Health Catalyst performance dashboard. Specifically, ACOs and MIPS APM participants can submit their performance to CMS for the three self-reported measures in the APP. Additionally, MIPS APM participants or groups that previously reported MIPS quality performance through the CMS Web Interface can report any CQM available in traditional MIPS.
Care Delivery Changes
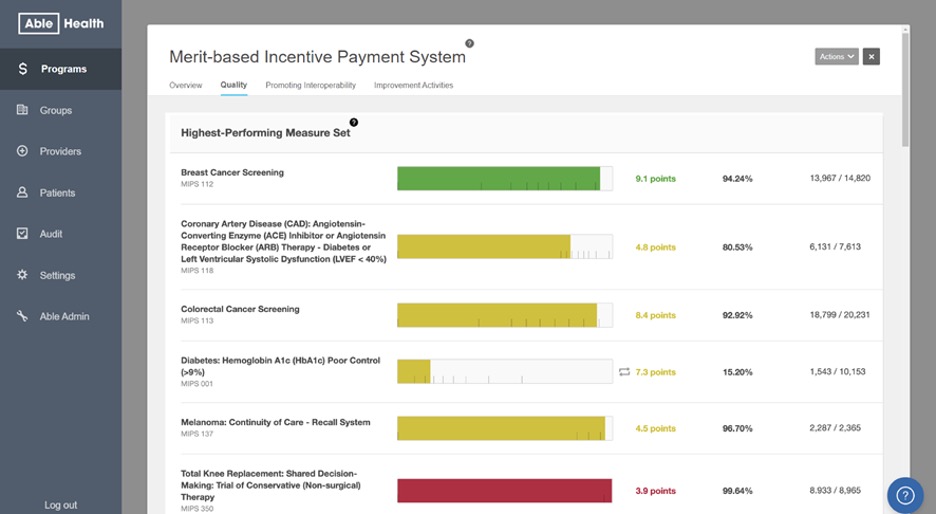
The Health Catalyst quality measures solution enables ACOs and MIPS participants to rapidly expand care delivery for quality measures to all patients, not just a sample of Medicare patients. Specifically, performance dashboards create visualizations that empower quality leaders and providers to monitor and improve their performance throughout the performance period across all measures and all patients (Figure 3). Additionally, Health Catalyst solutions embed care-gap lists into native EHR workflows for use by the care team at the point of care.
Data Collection
The Health Catalyst quality measures solution includes the Health Catalyst Data Operation System (DOS™). DOS integrates all your source data (claims, clinical, payer, etc.) into a single computing ecosystem by combining features of data warehousing, clinical data repositories, and health information exchanges. With DOS, you can combine complete data types and data sources into one place and then map all your structured data to the appropriate code types for the specific value sets used by the measures in your new submission method. Practically speaking, DOS allows your physicians and care teams to use the documentation workflow they prefer, not the unfavorable workflow prescribed by your EHR. Then, DOS does the heavy lifting of data aggregation, deduplication, and normalization.
Benchmarking
CMS creates different benchmarks for the different submission methods because of a consistently different performance rate across clinicians in each submission method. The consistent performance differences between submission methods are most likely due to different bottlenecks in the prescribed data collection for each submission method. Health Catalyst solutions can offset bottlenecks in data collection. That’s because the DOS and the Health Catalyst flexible measures engine can use all your structured data in performance calculations, not just some of it. The use of all your data increases your performance rates. And an increase to your performance rates will offset any increased benchmarks between the CMS Web Interface and CQM submission methods. Additionally, the CQM benchmarks and measure scoring are embedded into performance visualizations in Health Catalyst solutions.
Health Catalyst solutions overcome the challenges created by the introduction of the APM Performance Pathway (APP). Those challenges include the following:
Decrease in Quality Performance Scores for ACOs in the MSSP
CMS attributed the 10 to 15 percent decrease in ACO quality performance to changes it proposed to the revised quality scoring methodology for ACOs. CMS did not identify the specific factors that would cause that decrease to ACO quality scoring. However, one key difference would be the use of MIPS quality scoring. And as discussed in the previous section, Able Health by Health Catalyst can offset bottlenecks in data collection that reduce quality performance for various measures in different submission methods. That’s because the Data Operating System (DOS) and flexible measures engine included in the Health Catalyst quality measures solution can use all your data, not just some of it. Consequently, the increase to your performance rates can offset increased benchmarks.
Additional factors that could explain a decrease in performance include the reduced list of measures which excludes process measures with historically high performance for most ACOs. The Health Catalyst quality measures solution allows you to improve your quality performance with specific improvement tools. As noted previously, those tools include intuitive dashboards that empower quality teams to quickly identify the highest-priority improvement opportunities across measures, groups, and providers. Additionally, the solution includes care-gap lists automatically embedded into native EHR workflows for use by the care team at the point of care.
Decrease in APM Entity MIPS Scores for MIPS APM Participants
The Health Catalyst quality measures solution allows MIPS APM participants to monitor, improve, and submit their MIPS performance independent of their APM entity. Consequently, MIPS APM participants should seek to improve and submit their MIPS performance independent of their APM entity since CMS estimates that ACO quality scores will decrease by 10-15 percent. As described in previous sections, the Health Catalyst quality measures solution includes improvement tooling such as comprehensive performance dashboards and integrated care gap lists embedded into native EHR workflows.
As noted previously, clinicians classified as MIPS APM participants could have up to eight final MIPS scores. And due to the discontinuation of the APM scoring standard, CMS will now apply payment adjustments using the highest final MIPS score for MIPS APM participants. Consequently, quality teams can use the Health Catalyst quality measures solution to monitor, improve, and submit performance for MIPS APM participants at the different levels of participation for both the APP and traditional MIPS.
Here’s why that matters. Loosely speaking, half the groups in an APM entity will have a group score higher than the APM entity score. Consequently, quality teams should report these groups independent of the APM entity. Additionally, half of individual clinicians in a group will have an individual score higher than the group score. Consequently, quality teams should report these individuals independent of the group. CMS will receive and assign multiple final MIPS scores for these groups and individuals. However, due to the discontinuation of the APM scoring standard, CMS will only use the highest final score to assign MIPS payment adjustments. Consequently, monitoring, improving, and submitting performance at all four levels of participation will increase MIPS payment adjustments for roughly half of MIPS APM participants.
As noted previously, APM entities can, but do not have to, submit traditional MIPS quality measures now that CMS includes APM entities as a MIPS submitter type. APM entities such as ACOs can use Health Catalyst solutions to monitor APM entity performance in the APP and traditional MIPS. Health systems that manage an ACO and employ participants in the ACO can submit the APP for MSSP participation and traditional MIPS quality measures to increase the APM entity MIPS score and, therefore, increase the MIPS payment adjustment for the system’s employed providers.
Would you like to learn more about this topic? Here are some articles we suggest:
PowerPoint Slides
Would you like to use or share these concepts? Download the presentation highlighting the key main points.