As data in healthcare becomes more available than ever before, so does the need to apply that data to the unique challenges facing health systems, especially in a pandemic. Even with massive amounts of data, health systems still struggle to move data from spreadsheets to drive change in a clinical setting.
These six methods allow health systems to transform data into real-world analytics, going beyond basic data usage and maximizing actionable insight:
1. Create effective information displays.
2. Add context to data.
3. Ensure data processes are sustainable.
4. Certify data quality.
5. Provide systemwide access to data.
6. Refine the approach to knowledge management.
Advancing data use in healthcare with real-world analytics arms health systems with effective tools to combat COVID-19 and continue delivering quality care driven by comprehensive, actionable insight.
 Download
Download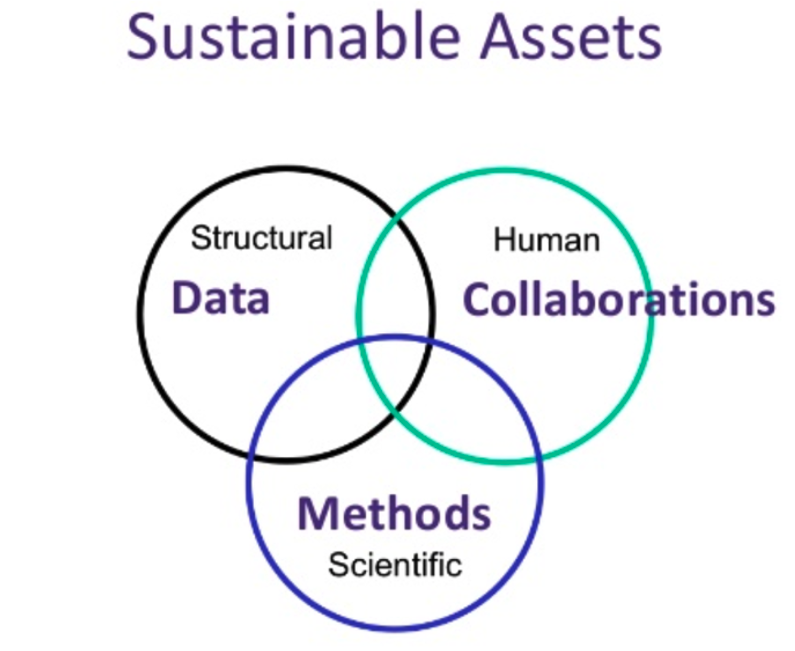
This article is based on the webinar presentation, “Real World Analytics: Advancing Methods and Literacy in Healthcare” by Adam Wilcox, PhD, Chief Analytics Officer for University of Washington Medicine and Professor of Biomedical Informatics and Health Education at the University of Washington, and Dale Sanders, Strategic Advisor at Health Catalyst.
Historically, to access data, health systems had to collect data manually from patients or providers. Organizations have now moved from hunting for data to gaining access to more data than ever before due to widespread EHR adoption. However, even with abundant data, organizations still struggle to leverage effective methods that result in real-world analytics. Health systems may successfully locate and aggregate data, but they often don’t advance the data beyond this point and therefore fail to leverage data to drive processes, workflows, and decisions.
While health systems have gotten by with this antiquated approach to data, COVID-19 demands more actionable strategies. The rapid onset of the novel coronavirus has made health systems realize that the most effective way to fight COVID-19 is to leverage more than data—real-world analytics. However, data approaches that focus on finding and aggregating data don’t fully equip health systems with the timely, comprehensive information they need to keep up with the ever-changing virus, making it more difficult for organizations to quickly respond to COVID-19.
With little data available about COVID-19, healthcare organizations (e.g., health systems, healthcare governing bodies, and pharmaceutical companies) have had to rely on each other to collect as much data as possible and then quickly share that data to track the evolving coronavirus. However, if these healthcare organizations lack sophisticated data interoperability, the delay in data sharing can result in worse patient outcomes, such as higher mortality rates.
For example, at the beginning of the pandemic, the Centers for Disease Control (CDC) requested that a health system with high volumes of positive COVID-19 cases submit weekly data reports including extensive information about where patients with COVID-19 received care (e.g., ambulatory care, urgent, emergency department (ED), or ICU). The information included total COVID-19 cases, the number of people tested, and the number of positive cases. The CDC requested this data broken down by race and ethnicity. Even though this health system had a robust and skilled team of data analysts, it struggled to provide this data on a weekly basis due to the time-consuming nature of the work.
The above example of collaboration—and roadblocks to collaboration—between the CDC and the health system highlights the importance of prioritizing new methods to access real-world analytics. Although organizations can provide easy-to-use data tools like common data models, query tools, and analytics applications to increase team member analytics involvement, the following six methods push health systems beyond basic data use to gain a better understanding of data and leverage data to drive improvement in a day-to-day clinical setting.
Effective information displays allow leaders and decision makers to view data within the scope of the health system as a whole and avoid seeing data in silos. The sum of the parts of the information display is less meaningful than the display itself. For example, based on the colors or density of information in a dashboard, providers might interpret the data as a busy day in the ED. But, if the elements that make up the display take away from the bigger picture (e.g., that the ED had a busier day than yesterday), the display fails to achieve its full purpose.
An insightful display aggregates all of the data related to a health system’s key performance indicators (KPIs) into one place, including peripheral data that adds to the bigger picture. Effective displays also provide accountability, so decision makers at every level know who is responsible for which measure.
In today’s healthcare world, patients often receive care from sources inside and outside the hospital. Multiple care sources mean health systems must aggregate data from each source to provide a full picture of patient health. Also, just as crucial as aggregating the data, health systems must provide information to the community in ways healthcare consumers can understand.
For example, Washington Heights/Inwood Informatics Infrastructure for Community-Centered Comparative Effectiveness Research (WICER) conducted a study focused on public health by distributing self-assessment health diagrams to community members. The health diagram had four areas that health experts considered necessary for assessing health. When researchers delivered the findings to community members, they provided context by including information about how each individual compared to an ideal baseline and their peers. This context helped individuals understand how they fared in the bigger picture, common health challenges within their community, and what they could improve. Adding context in this way was critical to helping community members improve their health and understand and interpret the community health data from the health system.
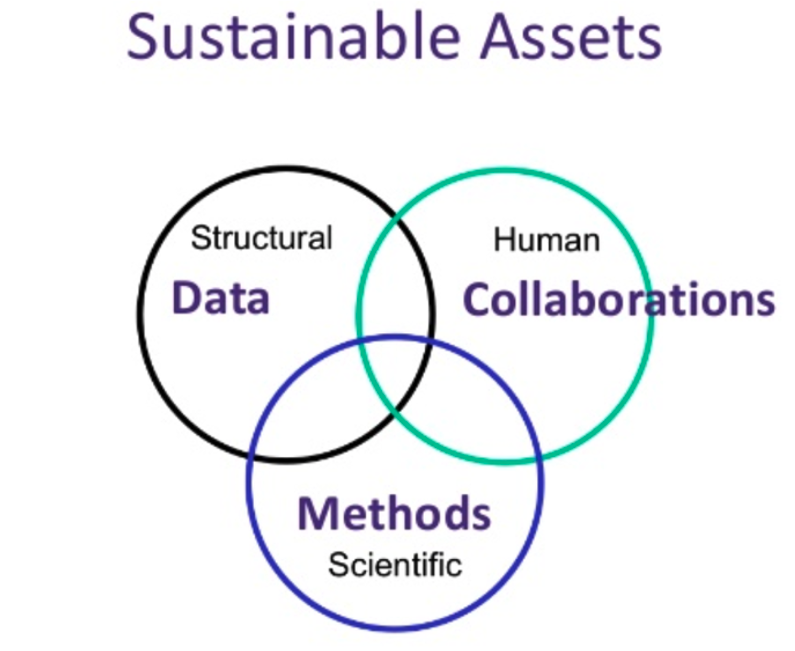
To build data sustainability, health systems need to understand their assets as more than just data, but also human collaborations, and scientific methods (Figure 1).

When health experts review their assets, they often see the data as the most critical asset in driving change, but over time, experts see that the data alone becomes less important without scientific methods and human collaborations. For example, the WICER research team had data based on interview responses from community members but when they stopped conducting those interviews, the data became less relevant over time. However, team member collaborations resulted in applying the data to scientific methods, such as leveraging the data in research efforts and using it to guide community outreach. These methods helped the data become more valuable and more sustainable as time went on.
Many health systems can identify poor-quality data but fail to identify high-quality data. By creating measures that define high-quality data, organizations will know when their data meets their quality threshold. For example, a care team could define and measure quality data by completeness, fidelity, and plausibility. Historically, data users would write a query, generate a report, and then consider the data analysis complete. Reaching a high data-quality threshold goes beyond the former process: now, a data user has to review the report in depth and decide if the data looks correct, identify variances, and ensure the data offers insight. Too often, the data reflects what it can measure but not necessarily what is happening in the real world, making a data user’s understanding of quality data (e.g., completeness, fidelity, and plausibility) critical for data to reflect real-world events and outcomes.
Widespread data access—or data democratization—means team members at every level have access to data and can make data-informed decisions. However close health systems may seem to data democratization, most still face significant barriers. One obstacle is the time it takes to deliver the right data to the right people. Data stewards need to understand which team members have access to what data. Typically, health systems have a group of analysts or developers who have access to all data sets. Team members then make data requests through the data analysts. Sometimes it can take months to access data because people don’t know where to find the data sources or don’t know the process for requesting access.
To improve data access, health systems can provide instruction, or an analytics curriculum, that addresses what data is available, how to request data access, how to access the data, and finally, how team members can use that data in their day-to-day tasks. While an analytics curriculum doesn’t eliminate the time-consuming processes of accessing data and generating reports, it can speed up the process. Another way to improve data access is to build query libraries (existing data searches that non-data experts can use) and data models (existing common data models, so non-data experts don’t have to reinvent the wheel).
In the past, knowledge management focused on data modeling and hierarchies, with decision support driving documentation. Knowledge management has changed drastically since then, as health systems focus on storing data, data definitions, and phenotypes. For example, phenotypes act as breadcrumbs that reveal what different data sources represent. Rather than decision support driving documentation, predictive analytics and pattern recognition should drive decision support.
Many health systems still revert to their previous knowledge management approaches that focus too heavily on data modeling and data hierarchies. Health systems need to change their mindset and see data usage as driving knowledge management because data-driven knowledge management is a critical step in advancing healthcare to real-world scenarios.
For health systems to quickly react to COVID-19 with the best defense—comprehensive, actionable data—they must go beyond basic data use and processes and derive real-world analytics from their data. Relying on old data approaches that prioritize finding and collecting data delays effective analytics use and creates an environment in which team members depend on analysts to query thousands of data elements for each report and then wait weeks or months for the information.
With the novel coronavirus threatening long-term financial strain (and collapse, in some cases), draining resources, and halting typical revenue-generating procedures (e.g., elective surgery), real-world analytics are now paramount for health systems to survive the pandemic. While data maximization strategies are continually evolving, healthcare organizations can advance real-world analytics use by applying the six data methods described above and foster a culture that uses data to drive meaningful improvement—in a pandemic and beyond.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.
Click Here to Download the Slides
https://www.slideshare.net/slideshow/embed_code/key/3kIpo981DKJf95