Health systems have always faced bad debt—from charity care to insurance claim denials—and COVID-19 has exacerbated its impact on revenue. While hospitals and clinics are responsible for providing care to populations, they can still generate revenue from care delivery without compromising care accessibility or quality. An effective bad debt management approach provides the patient with every financial resource possible and allows the health systems to focus less on payment and more on delivering the best care.
With four tactics, health system leadership can identify bad debt and implement effective processes to minimize it without undue burden on patients:
1. Identify bad debt exposure early.
2. Educate patients about alternative payment options.
3. Leverage technology within the workflow.
4. Understand the true cost of care.
As health systems continue navigating the challenges of COVID-19, leaders feel pressure to increase revenue on thin margins with limited resources while facing an uncertain future. While organizations weren’t prepared for the novel coronavirus, many have done their best to respond and find ways to optimize performance. One way health systems can survive financially amid the pandemic pressures and reduce economic vulnerabilities is to manage bad debt.
Bad debt write-offs represent the amount a patient or other payer cannot (or will not) pay of its portion of the bill. The hospital considers bad debt unrecoverable and, therefore, it directly decreases revenue. Simply put, the more bad debt a health system has, the less revenue it generates.
Health systems incur bad debt (aka write-offs) they perform a service or procedure for a self-pay patient (without insurance) or underinsured patient who cannot pay for the service. Write-offs are also incurred due to registration and coding or billing errors, such as not verifying a patient’s insurance coverage for a procedure. Currently, the number of uninsured patients is increasing due to recent job losses and a rise in high-deductible health plans. These factors have increased the cost burden on patients, making it difficult for hospitals to collect full payment from patients. And, as a result, the hospital identifies these balances as bad debt and writes them off.
Although health systems are primarily responsible for providing care to the communities they serve, there are ways they can decrease bad debt and maximize their ability to collect revenue for every procedure without compromising care quality and accessibility.
Since the onset of COVID-19, many people have lost health insurance coverage due to unemployment, leaving patients with little means to pay for healthcare. Despite funding resources, such as Medicaid or government stimulus money, health systems still fail to collect money from procedures as a result of patients’ job circumstances or even high-deductible plans that employed persons cannot pay.
While financial leaders might focus on other cost-saving strategies (such as layoffs, service reductions, or reducing overhead expenses) that will also yield margin improvement, they should not overlook the financial return of minimizing bad debt exposure. Minimizing or eliminating bad debt can result in a direct increase in revenue for health systems, and even small reductions in bad debt can drastically move the revenue needle. For example, if a health system with an annual revenue of $2 billion reduced bad debt by 10 percent, it would save $3 million. Or, put another way, it would generate $3 million more in revenue.
Bad debt is inevitable, and hospitals will never eliminate it, but leaders can implement four tactics to recognize bad debt exposure and minimize it as much as possible. Reducing bad debt exposure also offers more financial support to patients as they travel through the complex patient payment roadmap (Figure 1).
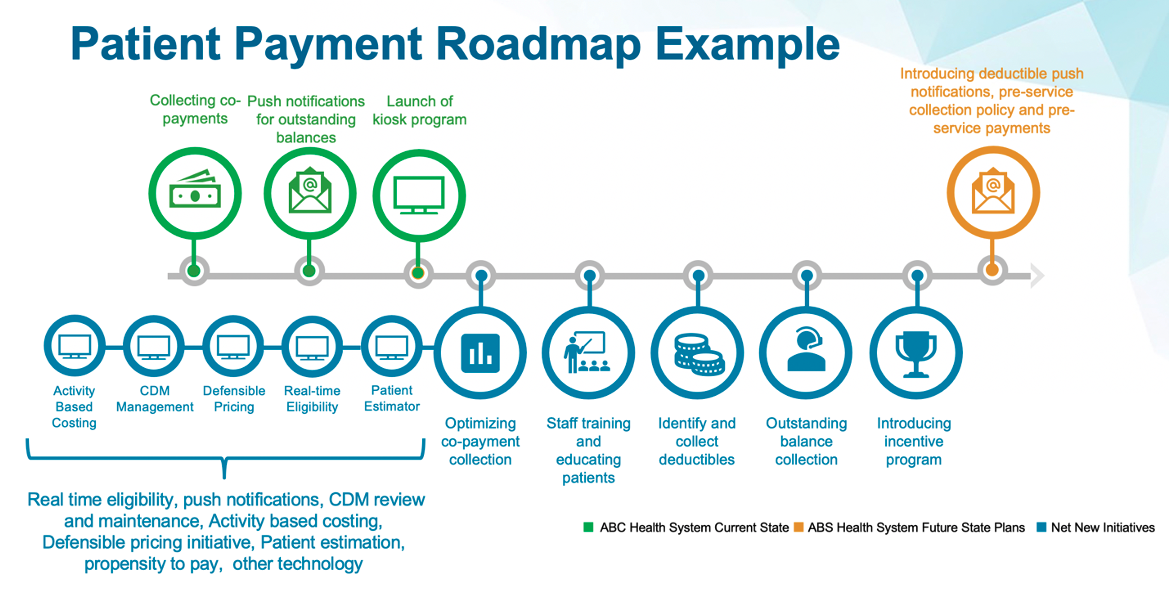
A health system should prioritize identifying bad debt exposure and consider how it currently identifies that exposure. If the system does not have the right steps in place, it can alter existing workflows to improve early identification. Ideally, a health system has the right workflows in place to identify bad debt exposure as early as possible in the patient encounter. For example, a health system could implement a pre-registration program to register and financially clear or flag a patient prior to the day of a procedure. If it flags a patient as a financial risk, the health system can create a payment plan or require a deposit for non-emergent procedures to avoid incurring bad debt.
Early bad debt identification allows health systems to adjust workflows and implement new mechanisms to work with and identify possible payment sources, patients on high deductible plans, and patients without insurance. Technology, like a propensity to pay (P2P) machine learning model, can also enable effective bad debt identification processes and workflows. For example, Allina Health implemented a P2P machine learning model to predict if patients will pay their healthcare bill within the month of their procedure and, in doing so, increased overall collections by $2 million in one year.
Once health systems understand the technology chasms, they can implement appropriate technology that will flag early signs of bad debt possibilities. Health systems can then collect revenue by arranging alternative payment methods to meet the patient’s needs while still providing care.
The principle of providing care specific to each patient’s unique needs doesn’t only apply to the clinical side of healthcare. On the administrative side (including finances), registration and patient accounting department team members can offer financial payment alternatives that meet the specific needs of patients. For example, if a self-pay patient can’t pay for a procedure in full, the hospital can offer alternatives, such as seeing if the patient qualifies for Medicaid or offering an interest-free loan program. Often, patients don’t pay for services because they don’t understand their bill and aren’t aware of different payment options.
Price transparency can help health systems communicate these costs and therefore identify the best payment options for patients. Tools that offer price transparency, like the Vitalware Hospital Price Index, allow health systems to understand the nuanced costs of any procedure, such as the gross charges and the minimum and maximum procedure charges for individual services. With transparency into a procedure’s total cost, revenue cycle team members can work with patients to find the best solution for everyone.
The next way to minimize bad debt is to leverage an analytics platform that maximizes data—such as the Health Catalyst Data Operating System (DOS™)—within existing workflows:
Although health systems have come a long way in understanding cost, some financial leaders still fail to understand the true cost of delivering care. Leaders don’t always know the true cost of care; they usually know the general cost of care and cost for a particular unit, but access to the granular, service-line-level and procedural-leveldata will reveal specific opportunities to decrease bad debt. Leaders must understand the true cost of care for every type of patient—from fully insured to self-pay patients—because the true cost will drive decisions around decreasing bad debt. Without understanding the true cost of a procedure, a health system could be writing off revenue and still expending resources to perform the procedure.
It is critical that financial leaders have data-informed activity-based costing infrastructure in place. For example, the Health Catalyst CORUS® Suite, the Vitalware CDM and Hospital Price Index create a defensible pricing strategy—a strategy using cost, reimbursement, and market information to defend the price a health system places on any given procedure. Because many organizations don’t know what procedures cost (only what they charge patients), it’s difficult to justify the cost of a procedure. A defensible pricing strategy is key to defending prices when patients, payers (used as leverage to negotiate), or community members ask. The health system can use accurate cost information to communicate that they may not be the highest price provider and why a procedure has a certain price tag.
In understanding what it costs to deliver care, organizations create tighter policies or employ mechanisms to help patients make more informed decisions. For example, if a total knee replacement costs the hospital $15,000, the hospital understands that if they do not collect any revenue, they will incur $15,000. Understanding the costs means having more controlled mechanisms in place to prevent losing revenue, especially for high-dollar procedures like knee replacements.
Bad debt is a growing concern for health systems because it increasingly reduces topline revenue. With better controls and processes in place, health systems can identify bad debt and create strategies to mitigate it or, in some cases, eliminate it. And, with new regulations requiring public availability and higher levels of transparency of a health system’s chargemaster, shoppable services, and all services, effectively managing bad debt is even more critical for financial success.
As well as delivering the right care, a health system is also responsible for giving each patient every financial resource possible so that the cost of care doesn’t stand in the way of receiving care and achieving optimal health. Better bad debt management allows health systems to enjoy the long-term benefits of fiscal responsibility, such as growing services, hiring more providers, building better facilities, and, most importantly, focusing on providing the highest quality of care.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.
Click Here to Download the Slides
https://www.slideshare.net/slideshow/embed_code/key/FCGXv5vTIoqyTM