Health systems continue to prioritize reducing hospital readmissions as part of their value-based payment and population health strategies. But organizations that aren’t fully integrating analytics into their readmission reduction workflows struggle to meet improvement goals. By embedding predictive models across the continuum of care, versus isolated them in episodes of care, health systems can leverage analytics for meaningful improvement.
Organizations that integrate predictive models into readmissions reduction workflows have achieved as much as a 40 percent reduction in risk-adjusted readmissions indexes. Effective analytics integration strategies use a multidisciplinary development approach to meet the needs of a patient’s entire care team and deliver common tools for all involved in the patient’s healthcare journey.
 Download
Download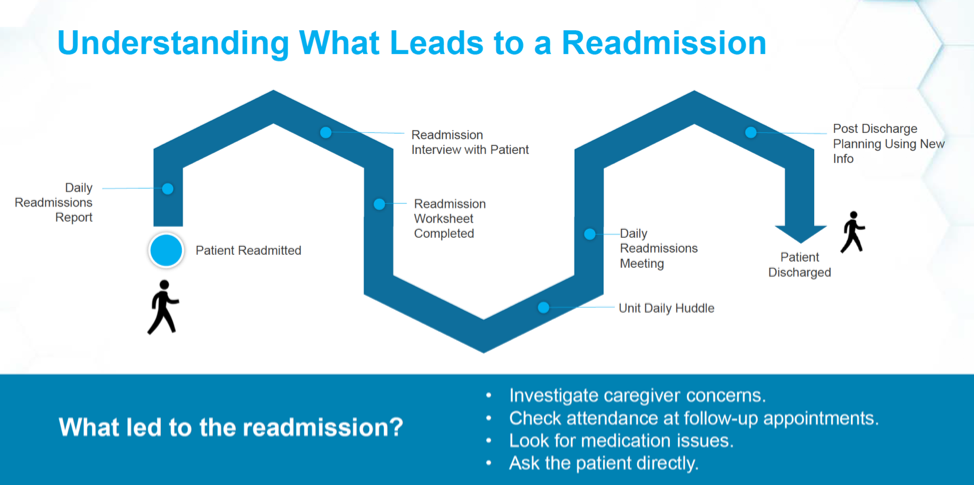
This report is based on a 2018 Healthcare Analytics Summit presentation given by Rhiannon Harms, Executive Director, Strategic Analytics, UnityPoint Health, and Ben Cleveland, Data Scientist, UnityPoint Health, entitled, “Leveraging Predictive Models to Reduce Readmissions.”
To meaningfully reduce readmissions and meet value-based care goals, health systems must implement analytics in their real systemwide workflows. In many organizations, predictive models are isolated along the continuum of care, where they’re applied to certain silos but not integrated across workflows. By fully integrating analytics models into its workflows, such as a readmissions reduction strategy, and supporting their adoption, a health system can realize meaningful improvement.
Fully integrated analytics deliver real results: A hospital in a regional health system that used an integrated analytics approach improved its risk-adjusted readmissions indexes by 40 percent over three years. The facility surpassed internal system targets in performance and became a top performer in the health system.
This report describes how healthcare organizations, like the example above, can build and adopt predictive models for reducing readmissions and fully integrate these strategies into workflows. Integrated analytics is multidisciplinary effort, requiring input for all individuals connected to the patient’s care (e.g., primary care providers, nurses, care managers, and home health and skilled nursing facility teams), that delivers a common tool for all care teams.
With integrated analytics tools and methods, health systems can achieve four chief goals around reducing hospital readmissions:
Before a healthcare organization builds an applicable predictive model for readmissions risk, it needs a comprehensive picture of the patient readmissions journey. Critical factors in understanding a patient’s return to the hospital include caregiver concerns, whether the patients attended follow-up appointments, medication issues, and patient-reported concerns (e.g., asking patients directly, “Why do you think you’re back?”).
To understand readmissions, the strategy must use patient data from readmission to discharge, including critical touchpoints in the process (Figure 1):
Having a predictive model alone won’t automatically help health systems reduce readmissions. To best leverage an analytics solution, health systems need to know where in the patient’s readmission journey to implement it, as well as have the ability to cut the data to show appropriate views for different teams (e.g., service line or diagnoses group views).
The analytics team delivers essential capabilities to make predictive models actionable:
The health system from the example in the introduction used several readmission risk reduction tools to achieve its 40 percent improvement in risk-adjusted readmission indexes over three years:
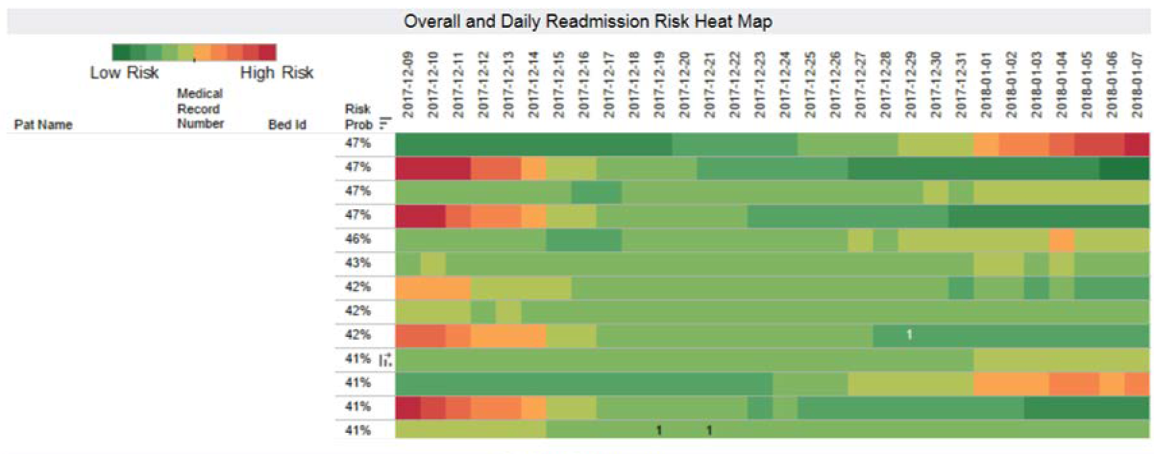
Figure 2 shows an inpatient readmission risk dashboard, which displays readmissions risk for all patients in the hospital with a color (from a low in green to a high in red) to indicate daily risk. Care teams can use this specific risk insight to plan appropriate strategies and interventions for each patient.
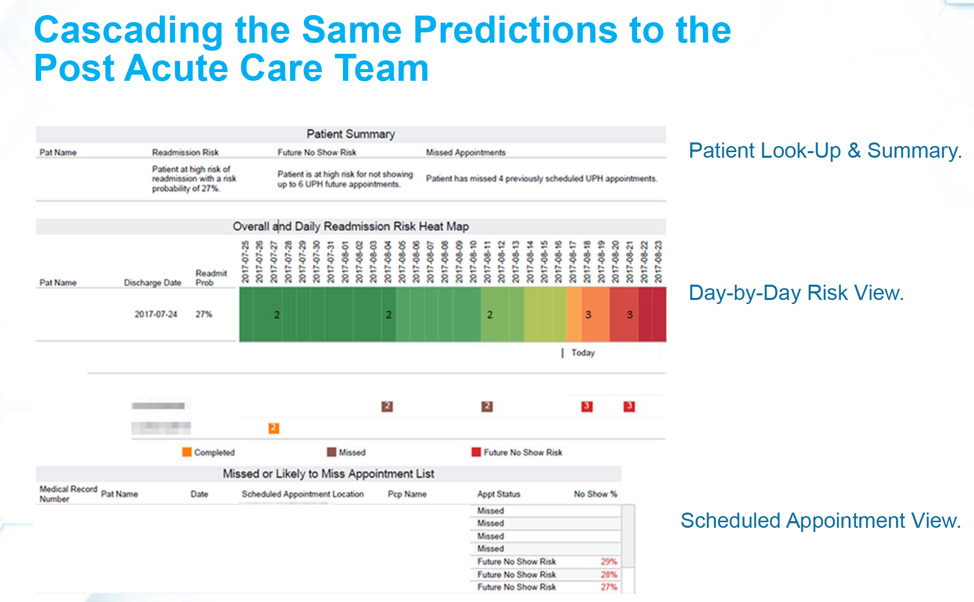
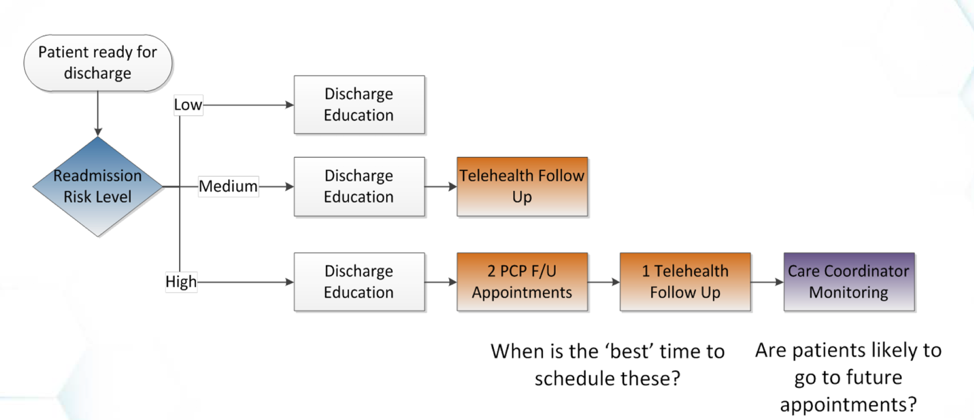
The post-acute care team dashboard (Figure 3) moves patient risk data to a discharge dashboard that overlays follow-up appointments on top of risk. The overlay highlights vulnerable points in the patient journey. Care teams can determine risk levels and make an appropriate plan (e.g., little intervention for low-risk patients or multiple follow-up appointments for high-risk patients) and determine the best time to schedule follow ups and the likelihood that the patient will make these appointments.
The triggers in Figure 4 show the different scenarios from the discharge risk assessment.
An analytics adoption strategy aims to meet three goals:
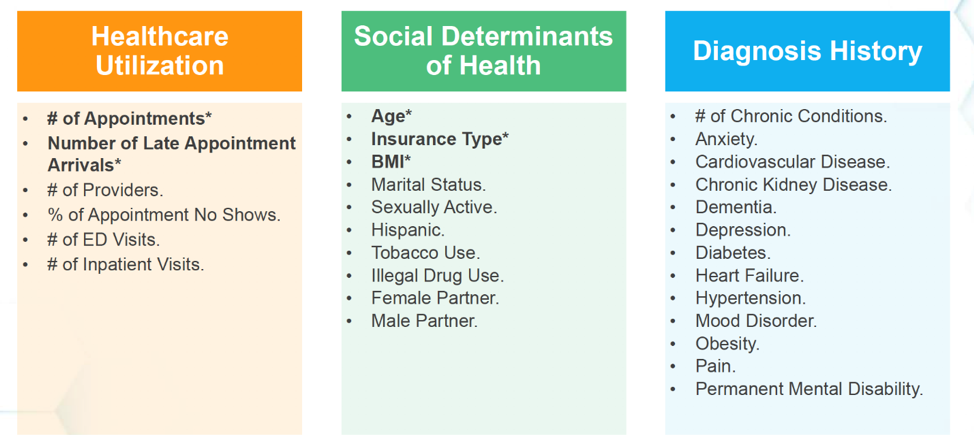
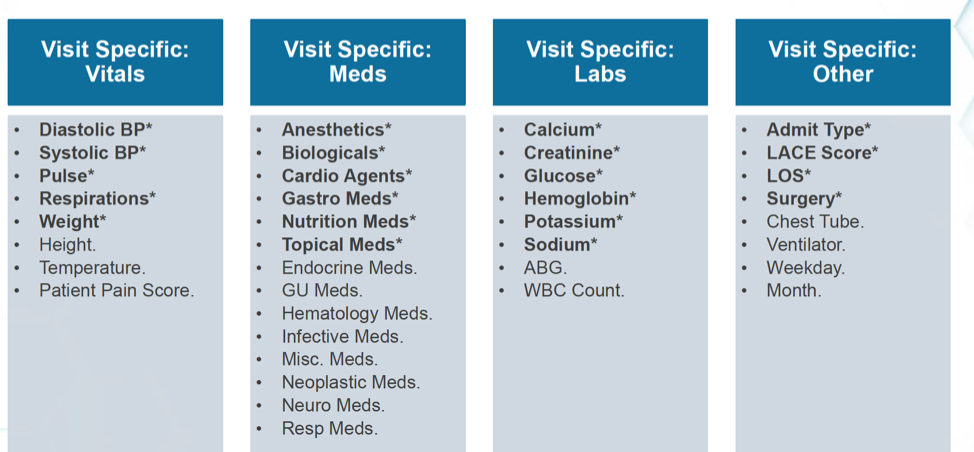
When reducing hospital readmissions, the strategy must span the domains of healthcare utilization, diagnosis history, and social determinants of health (Figure 5), as well as visit specifics, including vitals, labs, and medications (Figure 6).
Health systems can achieve significant reduction in readmissions by fully integrating predictive analytics strategies into their workflows. Applicable predictive models will consider the entire patient readmission journey, as well input from the whole care team and the patient; leverage the capabilities of the analytics team, and deliver accessible, easy-to-use tools with meaningful visualizations.
Would you like to learn more about this topic? Here are some articles we suggest: