Social determinants of health (SDOH) data captures impacts on patient health beyond the healthcare delivery system. Traditional health data (e.g., from healthcare encounters) only tells a portion of the patient and population health story. To understand the full spectrum of health impacts (e.g., from environment to relationship and employment status), organizations need data from their patient’s daily lives. The urgency for SDOH data is particularly strong today, as value-based payment increasingly presses health systems to raise quality and lower cost. Without fuller insight into patient health (what happens beyond healthcare encounters) organizations can’t align with community services to help patients meet needs of daily living—prerequisites for maintaining good health.
Standardizing SDOH data into healthcare workflows, however, requires an informed strategy. Health systems will benefit by following a standardization protocol that includes relevant and comprehensive domains, engages patients, enables broader understanding of patient health, integrates with organizational EHRs, and is easy for clinicians to follow.
 Download
Download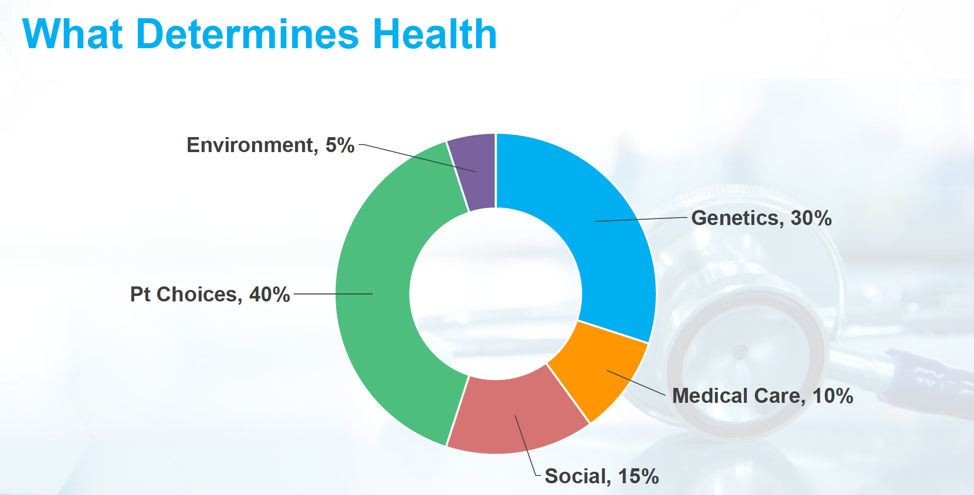
This report is based on a 2018 Healthcare Analytics Summit (HAS 18) presentation given by Andrew Hamilton, RN, BSN, MS, Chief Informatics Officer and Deputy Director of AllianceChicago, entitled, “Standardizing the Collection of Social and Economic Risk Data.”
As value-based payment (VBP) puts more pressure on health systems to reach quality targets and lower the cost of care, healthcare leaders are increasingly interested in strategies to better understand health and wellness in their populations. Strategies that leverage social determinants of health (SDOH) data are gaining attention for their ability to paint a comprehensive picture of health and address social and economic risk by connecting patients in need with the appropriated community services.
The World Health Organization defines SDOH as, “the conditions in which people are born, live, work, and age.” It adds that money, power, and resources at the global, national, and local levels shape these conditions and that SDOH significantly impact health inequities.
This report outlines the importance of SDOH in healthcare today and offers an example of a protocol for health systems to standardize SDOH in their workflows.
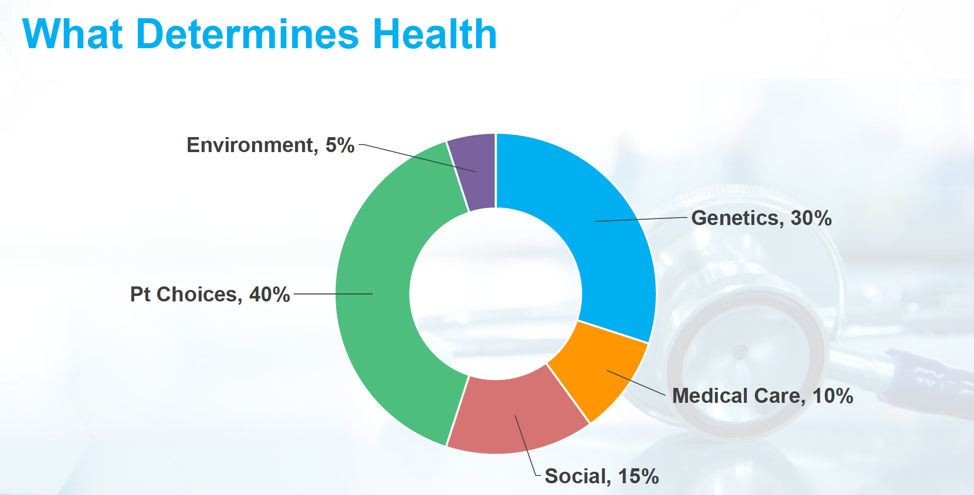
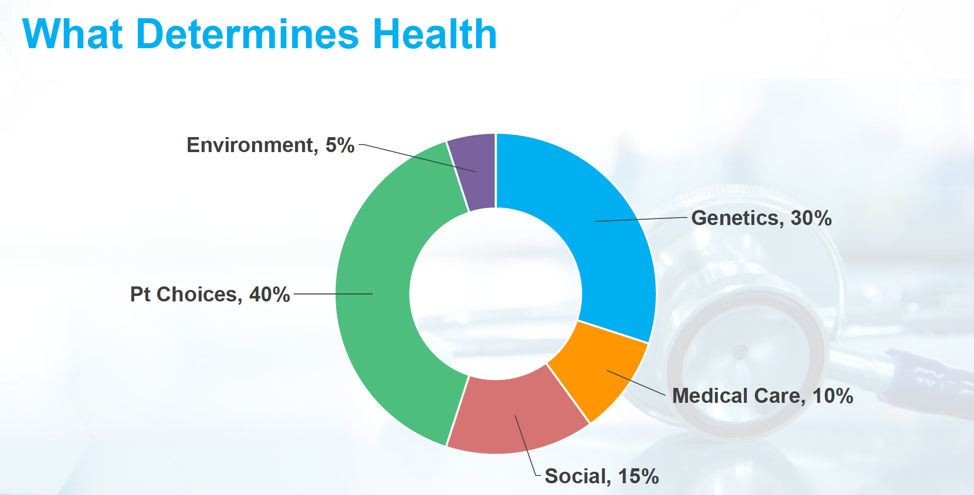
By capturing data on daily patient life (including socioeconomic and employment status, environment, etc.), SDOH data gives richer insights into factors impacting health than traditional healthcare encounters do—an especially important consideration with complex and underserved populations. Other data sources, such as genetics and healthcare delivery, can shed some light on quality and patient experience, but because patient choices are the biggest driver of health outcomes, true understanding demands a broader view. SDOH data captures patient choices and genuine experiences at a level traditional health data sources (which exist primarily within the four walls of healthcare) cannot. Figure 1 shows a breakdown of actual health determinants, with patient choices weighing in highest and just above genetics (30 versus 40 percent).
Data elements for SDOH cover a range of daily life beyond the healthcare delivery system:
Figure 2, a framework for health equity, shows both the “upstream” SDOH, or social-ecological, and the “downstream” medical data models. The goal of standardizing SDOH data is to help health systems leverage both sides of this diagram, ensuring incentivized and sustainable services addressing SDOH as well as integrated community partnerships.

Health systems can achieve four central goals by standardizing SDOH data within the EHR:
To meet these goals, health systems need an SDOH strategy that will leverage data for risk stratification as well as connect patients with appropriate community services. Doing so requires data interoperability, common sets of values, and the capability to harness SDOH data for analytic purposes.
Healthcare organizations can benefit from following a protocol for adopting SDOH into their workflows. For example, the Protocol for Responding to and Assessing Patients’ Assets, Risks and Experiences (PRAPARE) is a standardized patient risk assessment protocol that aims to engage patients in assessing and addressing SDOH. As described by Hamilton during his HAS 18 presentation, PRAPARE is a national effort and collaboration between multiple organizations to help health systems and other providers collect and apply the data they need to better understand their patients’ social and economic risks, with the goal to transform care to meet patient and population needs.
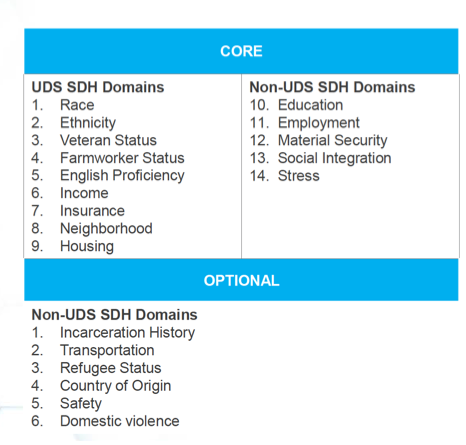
PRAPARE addresses 15 questions to assess 14 core SDOH domains. The Uniform Data System (UDS) for federal health center reporting already addresses nine of these domains. PRAPARE also has five non-UDS domains, taken from Meaningful Use Stage 3, and six optional domains (Figure 3).
An effective standardized patient risk assessment protocols for SDOH must collect data at an individual level and use that data at a population health level to inform care coordination efforts. The data must be accessible to clinicians at the point of care and at a national level to inform local, state, and national delivery redesign. As such, these protocols must meet key criteria:
Organizations looking for an effective standardized patient risk assessment protocol for SDOH will enjoy more effective outcomes if they choose a protocol with an implementation and action toolkit. The PRAPARE toolkit, for example, covers vital steps:
During two years of pilot studies (2015 and 2017), PRAPARE has met important performance targets:
Standardization protocols for SDOH data are a necessary place to start to integrate more patient social and economic data into healthcare delivery. As the industry moves toward greater health equity, key questions remain about the role of SDOH data moving forward. The next steps will need to identify the best ways to capture SDOH data (particularly for patients who have not engaged with the healthcare system) and use the data to inform the patient’s care plan. Additional understanding will include the correlation between specific SDOH and health outcomes and which business models will support sustainable and effective programs around SDOH.
Social and economic patient data will continue to play a critical role in healthcare as VBP further presses organizations to raise quality and lower costs. Health systems can best standardize SDOH data in their workflows with a protocol that includes relevant and comprehensive domains, engages patients, enables broader understanding of patient health, integrates with organizational EHRs, and is easy for clinicians to follow.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.
Click Here to Download the Slides
https://www.slideshare.net/slideshow/embed_code/key/3dN0FkVMT4yjgp