The year 2020 marks a decade since the passage of the Affordable Care Act in 2010 and healthcare’s first transitional steps from volume to value. The 10-year progress report is mixed. On one hand, CMS’s emphasis on quality and cost is driving an upward trend for patients and providers, with substantial improvement in readmissions; on the other hand, organizations still need to simplify and consolidate value-based programs for more widespread positive impact. As the industry enters into another decade of value, it’s time for health systems to consider the impacts of these programs so far and make sure they have the processes and tools in place to succeed in an increasingly value-driven industry.
In 2020, 10 years after the Affordable Care Act (ACA) passed and became in law (March 2010), CMS and healthcare organizations are still evolving and adapting policies and strategies to optimize outcomes and performance under value-based care (VBC). The most publicized areas of the ACA involved increased coverage for the uninsured and those with pre-existing conditions. The ACA also started CMS efforts to design and implement value-based programs—devised to encourage providers to improve quality by granting incentives for meeting regulatory measures or penalties for falling short.
CMS defines VBC as paying for healthcare services in a manner that directly links performance on cost, quality, and the patient’s experience of care. According to CMS, as of 2020, there are 31 programs defined as value-based; CMS sponsors 11 of these, and the Center for Medicare and Medicaid Innovation (CMMI) defines 20.
Three programs impacting health systems under VBC include the following:
In general, each program covers acute-care hospitals with exclusions for specialty hospitals, such as children’s, critical access, cancer, psychiatric, rehabilitation, and long-term care hospitals. Because these programs use selected measures first specified under the Hospital Inpatient Quality Reporting (IQR) Program, implemented in 2003, organizations were already reporting these measures, making them a natural basis for penalties and bonuses under VBC programs.
CMS reports and calculates yearly measures from a prior time period (generally, one to three years early). For example, the agency based the 2020 results for mortality on data from July 2015 to June 2018. CMS then shares the measures, definitions, and time periods with health systems for review and correction and makes the measures available on the public website Hospital Compare.
The agency then adjusts the hospital Medicare Severity-Diagnosis Related Group (MS-DRG) operating payment for the federal fiscal year to reflect the results of these measures. If the readmission measures show a need for improvement, the hospital may receive a penalty of 0 to 3 percent—an amount deducted from the MS-DRG payment. Medicare designed the program around readmissions because inpatient hospital spend reflects the largest share of Medicare overall spend.
Generally, CMS also scores hospitals in relation to each other, with the measures moving (recalibrated) as hospitals improve their performance. With this process, approximately the same number of hospitals will always receive an annual penalty. Under HACRP, for example, 25 percent of hospitals will receive a penalty each year. One exception is VBP, which scores on both improvement and achievement.
The following chart (Figure 1) is a summary of hospital value-based programs:
The above structure converts to a maximum penalty in 2020, equating to a 6 percent decrease on the MS-DRG operating payment for all three programs. In 2020, approximately 400 hospitals, or 12 percent of total eligible hospitals, received a penalty in all three programs, with penalties for those 400 hospitals totaling close to $400 million.
A 2015 Health Affairs study showed a bias against teaching hospitals and hospitals with greater than 400 beds, with those hospitals showing a mean penalty of -0.9 and -0.8, respectively. These rates are close to double the average hospital payment adjustment of -0.5.
In 2020 the VBP Program distributed a bonus payment to 56 percent of the eligible hospitals, or 1,530 acute care hospitals, with a median bonus of .4 percent of MS-DRG payments. This equates to a median payment of $65,000. Ten hospitals received over $1 million for their performance. On the downside, 1,200 hospitals received a penalty (median of .3 percent or $88,000). VBP is a budget-neutral program supported through a 2 percent reduction to payment; these funds are redistributed to hospitals achieving the higher scores on the measures.
VBP scoring for 2020 comprises four domains, each weighted at 25 percent:
The HACRP also measures HAC scores in the safety domain. Therefore, hospitals with low scores on these measures can receive a penalty in both programs.
The VBP score gives separate points for achievement and improvement: achievement uses a threshold and benchmark for hospital comparison, and organizations earn points awarded for improvement compared to a baseline, assuming they meet a threshold. Adding the higher score of achievement or improvement then generates a Total Performance Score (TPS).
Since its launch in 2012, VBP has made the following impacts:
In 2020 there were 3,129 hospitals in the VBP Program. Among these, 547, or 18 percent, received no penalty, and 2,583 hospitals got a penalty. Fifty-six hospitals received the maximum penalty of a 3 percent reduction of MS-DRG operating payments. The performance period was July 2015 to June 2018.
The HRRP reduces payments to hospitals when readmissions exceed an expected level. An excess readmission rate is calculated for a 30-day risk-adjusted unplanned readmission for the following conditions:
The HRRP doesn’t include the Hospital-Wide All-Cause Readmission (HWR) measure, and readmission measures for a hospital with fewer than 25 cases would not be included in the calculation.
CMS assigns hospitals to five peer groups based on the proportion of dual-eligible stays within the three-year performance period. The agency added this comparison in 2019 to account for more complex patients and the impact on readmissions. The reduction ranges from a maximin of 3 percent to no reduction in payment, with reduction applied to all MS-DRGs.
With the HRRP program, CMS is encouraging providers to increase communication and care coordination and be responsible for a patient’s post-discharge care.
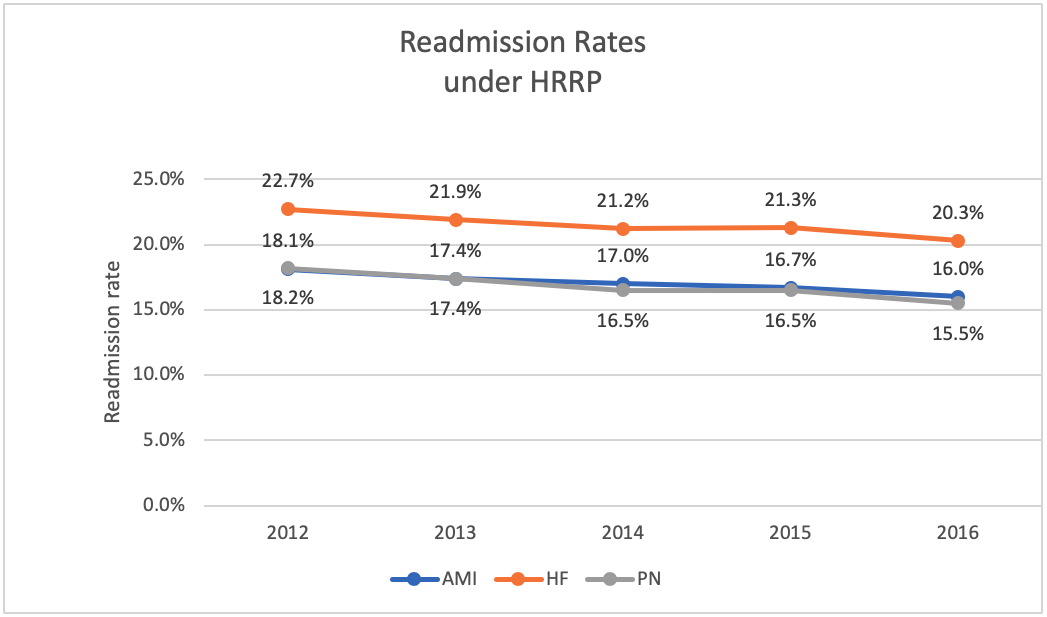
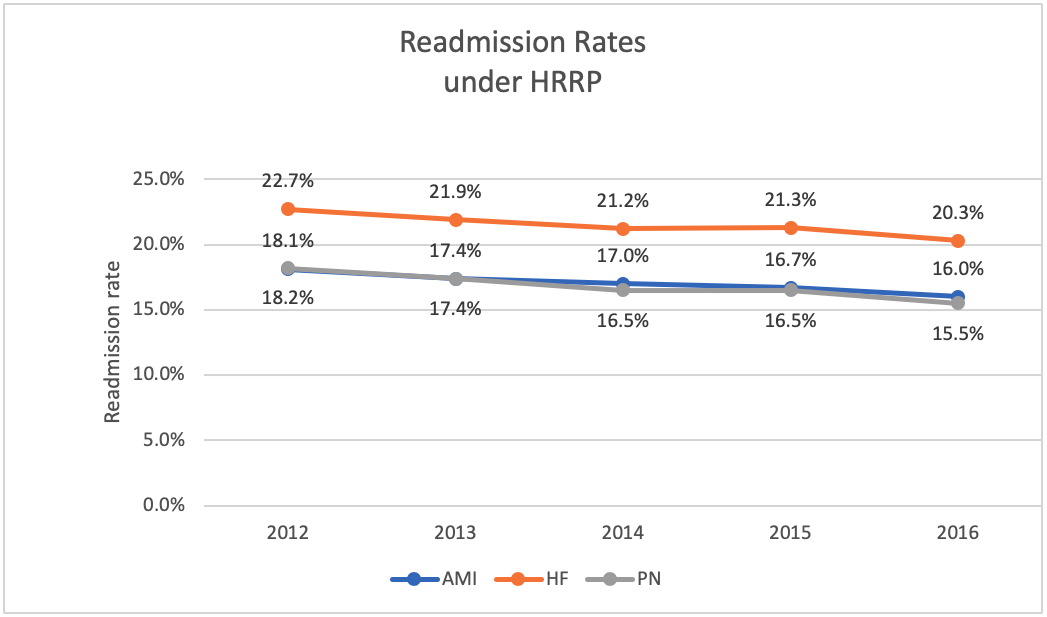
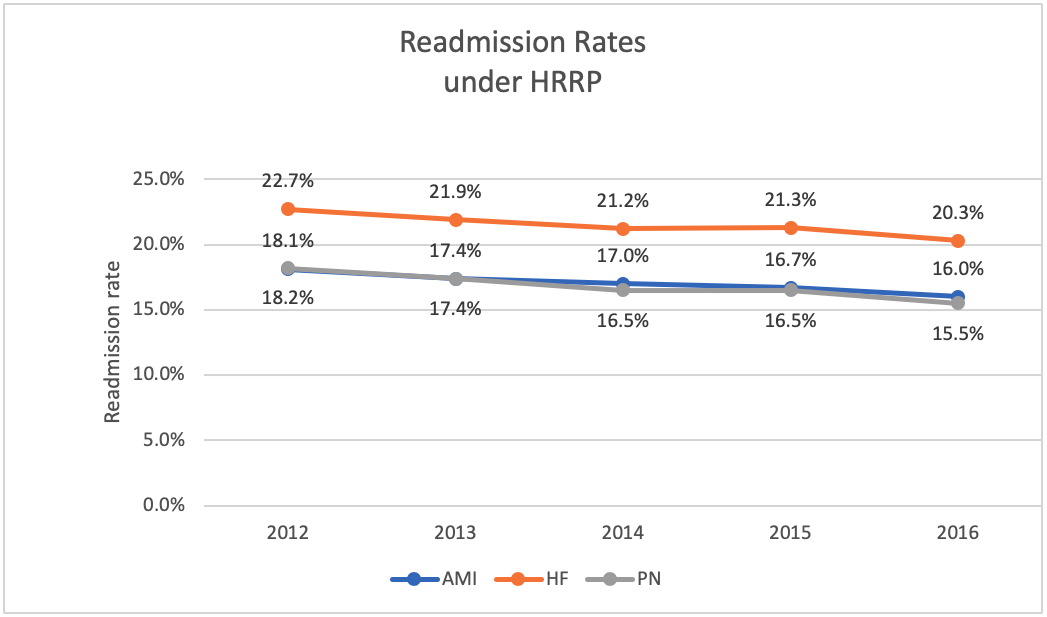
In a 2018 report, MedPAC stated the HRRP had been successful for beneficiaries and the Medicare program, with readmission rates declining after its implementation. Moreover, the decline did not materially increase outpatient observation or emergency department visits or adversely impact mortality. Rates declined from 2012 to 2016 by 3.6 percent for AMI, 3 percent for HF, and 2.3 percent for PN (Figure 2).
CMS applies a flat 1 percent payment reduction to hospitals that rank in the worst performing 25 percentiles of all hospitals under the HACRP. The agency designed the program to improve patient safety and lower the number of HACs. CMS estimates the program saves $350 million annually.
CMS calculates the patient-safety score using the following measures with PSI 90 in Domain 1 as one measure and each healthcare-associated infection (HAI) as a separate measure in Domain 2, for a total of six measures:
The following CMS Patient Safety Indicator (PSI) 90 measures for discharges from July 2016 through June 2018 measures count as one measure in the HAC program:
The Centers for Disease Control and Prevention (CDC) National Healthcare Safety Network (NHSN) HAI measures for discharges January 2017 to December 2018 each receives a score and counts as one measure (for a total of five):
In 2020 785 hospitals received a penalty under HACRP, with an average penalty of $350,000. The American Hospital Association (AHA) has commented on this program and the inherent bias in the formulas. An AHA study shows the penalties disproportionately impact teaching and large urban hospitals. There is not an adequate method to risk adjust the data.
The Agency for Healthcare Research and Quality (AHRQ) shows the rate of HACs declining. From 2010 through preliminary 2017 data, the average annual reduction in the overall rate of HACs was approximately 4.5 percent. The 2014 rate started at 99 HACs per 1,000 hospital discharges and is estimated at 86 HACs per 1,000 discharges for 2017. Based on these reductions compared with 2014, the AHRQ estimates a total of 910,000 fewer HACs in 2017. These HAC reductions link to savings estimates of approximately $7.7 billion in costs and approximately 20,500 fewer HAC-related inpatient deaths.
A 2019 study found improvements in rates of conditions pre-HACR from 133.4 per 1,000 discharges to post-program of 122.2 per 1,000 discharges. This study concluded the CMS program did not improve patient safety beyond existing trends because greater improvement was observed in non-targeted measures (which are not part of the CMS HACRP). CMS states HACRP has yielded 2.1 million fewer incidents of harm and $28 billions of savings.
Both commercial payers and Medicaid lag behind Medicare in the spread of VBP. Several commercial payers have adopted programs to move to VBP, and Medicaid will vary by state, but momentum toward the value scale has accelerated:
Medicare is a large payer, representing generally over 35 percent of a health system’s gross revenue, based on California’s Office of Statewide Health Planning and Development hospital data. To keep the payments from decreasing, organizations need to manage and improve their quality metrics. Leading organizations are preparing for an increasing percentage of value-based arrangements in the future.
The following examples show systems moving to the new model of value:
Health systems can prepare for increasing value-based programs by taking the following steps:
Hospitals have learned from the Medicare value-based programs since 2010, with the emphasis on quality and cost proving to be a positive trend for the healthcare industry. Significant readmission improvements are benefiting health systems and patients, but organizations still need to improve and refine programs overall with an eye to simplification and consolidation. The industry also needs bring all stakeholders together to actively participate in healthcare improvement and question whether the current measures represent value to providers, payers, and patients.
In a March 2020 blog post, healthcare policy analyst Paul Keckley, PhD, summarized the current state of the U.S. system, explaining: “The transition from volume to value is inevitable but the road from here to there is bumpy.” With both inevitability and obstacles projected, healthcare organizations have the opportunity now to reevaluate and adapt larger changes to their programs and leverage predictive tools in preparation for the next decade of VBC.
Would you like to learn more about this topic? Here are some articles we suggest: