The University of Kansas Health System faced a 25 percent denial rate, higher than the best practice of five percent. To improve financial and clinical outcomes, it engaged more effectively with clinical partners. The organization redesigned its processes by identifying early revenue cycle issues and fostering collaboration between clinicians and finance. Within eight months, these efforts led to impressive savings and significant improvements in its revenue cycle management.
CMS denies nearly 26 percent of all claims, of which up to 40 percent are never resubmitted. The bane of many healthcare systems is the inability to identify and correct the root causes of these denials, which can end up costing a single system tens of millions of dollars. Yet almost two-thirds of denials are recoverable and 90 percent are preventable. Despite previous initiatives, The University of Kansas Health System’s denial rate (25 percent) was higher than best practice (five percent), and leadership realized that, to provide its patients with world-class financial and clinical outcomes, it would need to engage differently with its clinical partners.
To effectively reduce revenue cycle and implement effective change, The University of Kansas Health System needed to proactively identify issues that occurred early in the revenue cycle process. To rethink its denials process, it simultaneously increased organizational commitment, refined its improvement task force structure, developed new data capabilities to inform the work, and built collaborative partnerships between clinicians and the finance team.
As a result of its renewed efforts, process re-design, stakeholder engagement, and improved analytics, The University of Kansas Health System achieved impressive savings in just eight months.
Insurance claim denials are a significant financial liability for many health systems. CMS denies nearly 26 percent of all claims and 40 percent of those are never resubmitted, even though two-thirds are recoverable and 90 percent are preventable.1 Health systems struggle with claims denial management, including the inability to identify and correct the root causes, which can cost tens of millions of dollars.
Any large healthcare organization’s revenue cycle is filled with variation and complexity. Policies and procedures differ from payer to payer, technology and communication systems vary from patient to patient, and the complexities of separate hospital and professional revenue cycles in the same system can lead to defects and waste.
This was true with The University of Kansas Health System, which faced a 25 percent denial rate compared to the national best practice of five percent. The University of Kansas Health System is a large academic medical system with more than 80 locations in two states, 999 licensed beds, over 700 employed physicians, and 10,000 employees.
The University of Kansas Health System always had a vision of leading the nation in caring, healing, teaching, and discovering. But this vision was impaired by an unsustainable level of denied claims, leading to millions of dollars wasted annually. It understood that avoiding initial denials would reduce re-work and improve cash flow, but previous efforts proved too broad and required excessive effort from stakeholders. The University of Kansas Health System knew that in order to affect positive change in reducing denials that it would need to focus their effort, and do so in several areas:
Bottom line, The University of Kansas Health System needed to get upstream of its challenges with claims denial management, and needed a comprehensive improvement plan, informed by data, that engaged clinical, operational, and financial staff in improving the problem.
The University of Kansas Health System designed a comprehensive denials initiative, with a long-term goal to lower denial rates to the best practice industry standard of five percent. It simultaneously upped organizational commitment, improved its improvement task force structure, developed new data capabilities to inform the work, and built collaborative partnerships between clinicians and the finance team.
First, leadership set the stage for organizational commitment and success by endorsing and promoting the denials reduction initiative. The CEO, CFO, and COO provided visible executive support, and designated an executive champion, who conveyed the vision and the “why” for the work.
To engage clinical and operational leaders, executives articulated the vision and issues in a way that resonated with clinicians, illustrating how revenue cycle impacts patient experience. Clinicians understood that avoiding claims denials and getting billing right the first time would have a positive impact, and was the caring and right thing to do for their patients.
The revenue cycle improvement plan was built with an eye on sustainability and flexibility, and framed progress as a series of initiatives to drive sustainable change. The University of Kansas Health System recognized that focusing on specific problem areas identified in the data would lead to better outcomes than trying to “boil the ocean.”
Leadership stopped focusing on one-time tasks, and developed a culture of continuous improvement by conducting ongoing assessment, research, and continuous cycles of Plan, Do, Check, Act (PDCA), aligning lean improvement events to address specific areas of denials. This robust approach identified root causes and developed effective interventions to address inefficient processes, workflows, and manual entry.
The University of Kansas Health System realized that to maintain momentum and to sustainably reduce denials and write-offs, it needed a dedicated denials analysis team. It hired and trained a small, talented team to focus on denial trends and root cause analysis. The team was responsible for reporting, quantifying opportunities over time, identifying trends, and assessing improvement opportunities. In addition to its revenue cycle expertise, the team also had the skills to facilitate and develop partnerships with stakeholders.
Set with a dedicated denials team, The University of Kansas Health System needed meaningful data to move forward. Initially, it developed Excel-based solutions to replace inadequate stock reports from its EHR, creating visualizations that gave new insights into the data.
Once denial information was visible, the team identified two root causes that led to problems early in the process. Seeing and understanding denials information allowed it to address these core issues right away:
The University of Kansas Health System leveraged the learnings gained from these Excel-based solutions to build a robust denials analytics application in its Healthcare Analytics Warehouse and Knowledgebase (HAWK), using the Health Catalyst® Analytics Platform, including the Late-Binding™ Data Warehouse.
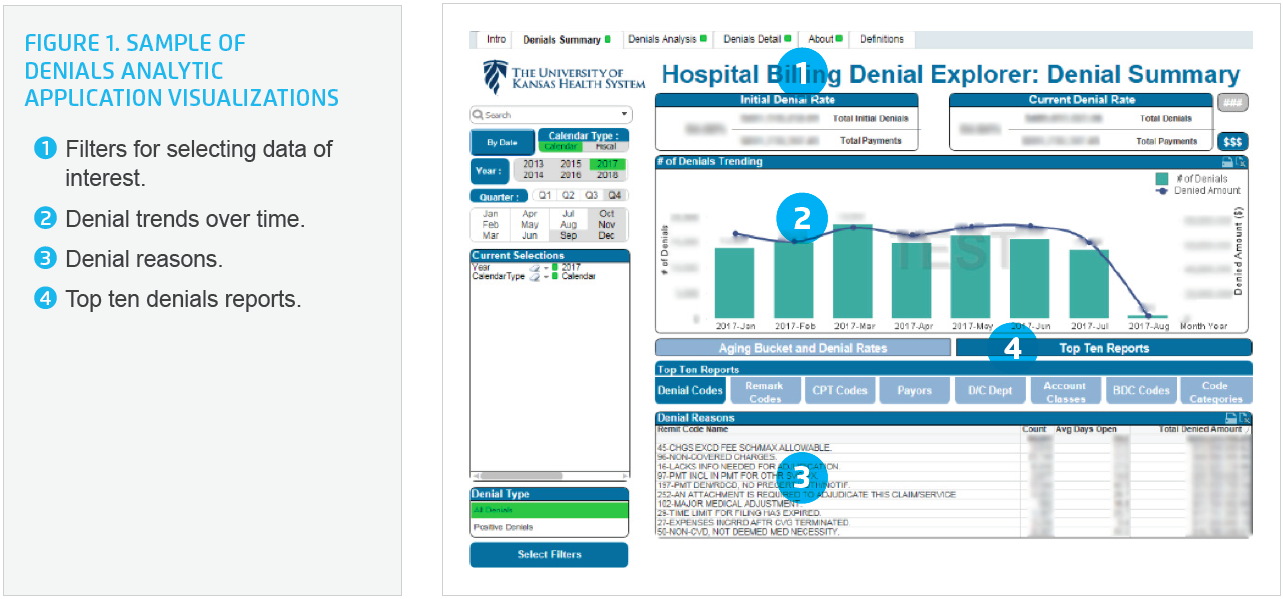
The analytics application exposed denials data in powerful ways, allowing the team to drill into, and explore, specific issues with ease. Using the analytics application, The University of Kansas Health System could visualize performance and obtain detailed information for denial trends over time, age of denials, and type of denial by denial code, CPT code, payer, department, and account class. With this actionable data in hand, it could standardize a core set of metrics (initial denial versus subsequent denials) that defined success in ways that everyone agreed to, and could understand.
Measurable results, visible in reliable, trusted analytics applications, enabled consensus and engagement, and led to the successful adoption of improvement initiatives.
In one example, data exposed issues with denials of treatments in the cancer center, where the organization assumed it had been doing well. The team explored the data with the clinic leader, created shared understanding of clinic processes, and identified possible underlying causes of denials. Operational expertise, coupled with actionable, visible data and analytics, helped drive successful and sustainable improvement efforts in the clinic. This kind of collaborative partnership led to operational leaders owning and driving improvement efforts, and the associated results.
As a result of its renewed efforts, process redesign, stakeholder engagement, and improved analytics, The University of Kansas Health System achieved impressive savings in just eight months:
“We were investing significant time to produce an incredible amount of data—but, when we shared it with our clinical and operational partners they were overwhelmed and the data was not meaningful to them. We needed to engage with our stakeholders differently.”
– Colette Lasack, MBA, Vice President, Revenue Cycle, The University of Kansas Health System
The University of Kansas Health System continues to hone and refine analytic tools for denials reporting. Ongoing refinement of the continuous quality improvement model for insurance denials will support enduring changes in payer denials. The team continues to engage additional operational leaders and departments to help tackle denials.


