An efficient accounting closing process delivers timely and accurate information to guide decisions and operational adjustments. Learn how UPMC implemented an analytics-driven cost management system, supporting a 50 percent reduction in the time needed to complete month-end close.
In healthcare, the timely delivery of patient-activity level cost metrics to clinical, financial, and operational leaders is critical and allows the organization to respond to internal and external shifts and challenges in a way that will positively impact financial performance without negatively impacting patient care and the patient experience. UPMC is a large integrated healthcare delivery system with 40 hospitals, as well as a robust network of clinics, cancer centers, outpatient centers, and a large network of employed and affiliated providers. As a highly complex healthcare delivery system, UPMC continuously strives to accelerate the timeliness of trusted business insights to inform operational and strategic decisions.
The general ledger (GL) accounting closing process is the routine preparation of accounts to produce financial statements. As a result of this process, health system revenue and expense transactions are summarized in the form of an income statement, which illustrates the income or loss for the period. The GL accounting closing process is an important precursor to the cost accounting closing process. The cost accounting close process relies on the GL, as well as various other data sources, to allocate revenues and expenses to patients and patient activities.
Trusted, timely, and actionable results require sophisticated data integrity monitoring and validation checks to ensure all GL revenues and expenses are accurately associated with clinical data from the EMR and other ancillary sources. Typically, software that serves as the “allocation engine” is required in conjunction with a database to handle complex assignment rules and large quantities of data. Given the scarcity of resources, many organizations face challenges with maintaining and managing complex assignment/ allocation rules and large quantities of data required to attribute costs at a meaningful level, in an appropriate amount of time.
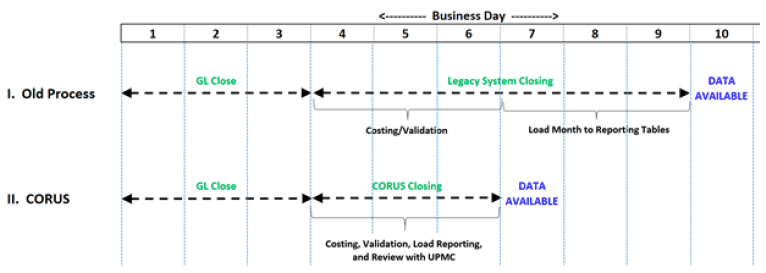
In order to accelerate and bolster the integrity of its cost accounting close process, UPMC partnered with Health Catalyst. This is the latest development in UPMC’s relationship with Health Catalyst, which includes an investment in the company. The cost accounting close process at UPMC took approximately six days and initialized immediately following the general ledger close. The cost accounting close process required six staff and over 60 manual steps to complete. Most of the time was spent on data processing, rather than validation and analysis; the health system determined that the manual effort needed to overcome the deficits of the suboptimal technical infrastructure and database supporting its current cost management system drove many of the delays built into its closing process.
After exploring the options to enhance and commercialize its cost management intellectual property, UPMC partnered with Health Catalyst to use the Health Catalyst® Data Operating System (DOS™) to co-develop and commercialize the PowerCosting™ application.
The new cost management system provided significant efficiency advantages:
With the ability to monitor each source system and inputs to the costing process daily, UPMC significantly improved its data integrity. Replacing multiple spreadsheets with five structured data source marts reduced, and almost eliminated, the need for manual intervention, which in turn reduced the time to generate reports that summarized cost metrics from a patient-activity level.
The new, analytics-driven cost management system supported a 50 percent reduction in the time needed to complete month-end close:
“The complexity and cumbersome maintenance of existing activity-based costing solutions have resulted in low adoption and limited success. We have spent years understanding and developing a standard methodology for calculating the costs of any patient service, and can now provide validated, data-driven, activity-based cost output within 3 days after the necessary source data is available. As reimbursement models change, hospitals and providers will need this level of routine intelligence to stay in business.”
- Bob Alexander, Director Implementation Services, Product Development
UPMC is preparing to deploy logic that’s built into the analytics application to support automated processes to check for data validity and further simplify maintenance. The health system will leverage these advantages to further streamline its closing process by resolving data quality issues more frequently during the month using ongoing feedback from financial and operational stakeholders.