Healthcare is shifting from fee-for-service to a value-based model focused on quality and cost-efficiency, driving growth in accountable care organizations (ACOs). In 2013, there were 606 ACOs in the U.S., with notable examples like Crystal Run Healthcare, recognized for pioneering efforts in population health management and collaboration.
Healthcare is transitioning from a transaction-based, fee-for-service payment model to a value-based model designed to deliver higher-quality, less wasteful care at the lowest possible cost. This new model emphasizes population health management and requires providers to take on risk and collaborate to an unprecedented extent.
The need for this level of collaboration has led to explosive growth in the number of accountable care organizations (ACOs). In 2013, there were a total of 606 public and private ACOs in the United States1 with 51 percent led by physicians and another 33 percent jointly led by physicians and hospitals.2
One pioneering, physician-led ACO is Crystal Run Healthcare in New York. This rapidly growing and forward-thinking organization has received national recognition as one of the first six ACOs to be accredited by the National Committee for Quality Assurance (NCQA), and one of the first 27 ACOs to be selected by CMS to participate in the Medicare Shared Savings Program.
Like the majority of ACOs, Crystal Run still receives most of its reimbursement—approximately 80 percent—under the fee-for-service model, but the organization is beginning to experience the long anticipated shift toward more value-based reimbursement. To ensure financial stability as they assume more risk, the ACO is implementing a strategy focused on rapid growth. Crystal Run already has more than 300 providers in 40 medical specialties with multiple practice locations. The ACO plans to grow to more than 1000 physicians, significantly expanding its geographic reach.
Crystal Run views its enterprise data warehouse (EDW crystal run) and applications as critical to the success of this strategy. This technology foundation enables sophisticated analysis necessary to position Crystal Run for continued success in an increasingly value-based reimbursement environment. In addition to population management, the ACO is leveraging the EDW and analytics to inform critical decisions about clinical excellence, operational optimization and growth targets and to identify new revenue sources such as government grants for treatment of Medicaid patients.
As Crystal Run leaders searched for technology to support their growth and population health management strategies, they knew they would need an analytics solution that would enable them to continuously improve in the following areas:
In addition to these general requirements, Crystal Run needed an analytics solution that could help address the day-to-day operational and clinical challenges that ACOs face. These challenges include:
Crystal Run’s growth has required and will continue to require the construction of new office buildings to support a growing patient base in expanded geographical locations. They were tasked with determining the best locations for these clinics and what provider mix was necessary to best serve patients. To tackle this question, they needed to understand where to locate the new sites and what types of providers they should staff to meet patients’ needs. The cost of large offices is not insignificant—often running into the tens of millions of dollars.
Like many healthcare providers, Crystal Run is anticipating increased participation in risk-based contracts involving bundled payments, shared savings and capitation. They need to understand what it costs to take care of a given patient population. Without this data, Crystal Run has little leverage, which means that payers will dictate the terms based on a risk score that is based on the average for the region. However, not all patient populations align with the regional average—and, in the case of Crystal Run, the bulk of the specialists in the community are in their network. Therefore, by selection bias, their patient populations are often inherently sicker and more complex than the general population. By having the data at the negotiating table, contract terms can be decided.
To ensure accurate reimbursement and assess physician productivity, Crystal Run needed to benchmark physicians’ performance based on their case mix and the risk profile of their patients. The ACO was particularly concerned about accounting for advanced procedures performed by sub-specialists that warrant a higher reimbursement rate.
As an ACO, Crystal Run’s mission involves improving population health and the patient experience while lowering costs. This requires physician engagement, a concerted focus on evidence-based practices and rigorous budget management.
Crystal Run decided that a healthcare-specific EDW was the best solution to help them meet these many challenges. The organization deployed the Late-BindingTM healthcare EDW platform from Health Catalyst, which they were able to get up and running in just 77 days. On top of this platform, they implemented foundational analytics applications to help them address the basic discovery measurements needed to effectively care for patients and manage access to patient care.
Here are some of the ways these foundational applications— including Key Process Analysis, Cohort Builder, Comorbidity Analyzer and Population Explorer—are helping the ACO address operational and clinical challenges:
The Population Explorer application (illustrated in Figures 1 and 2) visualizes the number of patients in each zip code area. It enables the ACO to view clinical data by county and by zip codes within each county (a given county can have as many as 100 zip codes). Importantly, the application also displays measurements for that population such as case counts, readmission rates, charges, revenue and length of stay. These metrics can be stratified by demographics and by clinical and financial information.


Using this application, Crystal Run was able to determine how many patients live near the proposed location for their new facility, understand what type of visits those patients were generating and in what specialty, and understand the potential volume of visits based on that information. They also explored risk and demographic information of patients living in the area.
Furthermore, when hiring new physicians, the ACO is now able to evaluate the patient volume for a given specialty in a county or zip code to help determine where the newly-hired specialists should practice or whether they should split their work week at different offices.
Summary dashboard provides insights into patient information, financials, demographics, visits and populations in one view, with filtering and drill-down capabilities to the patient and provider level.
Crystal Run is using the Cohort Builder and the Comorbidity Analyzer applications (Figure 3) to ensure that conversations with payers are more data-driven and accurate. With this application, the ACO can demonstrate the health complexity and risk associated with a given cohort of patients (such as diabetics) insured by each payer.
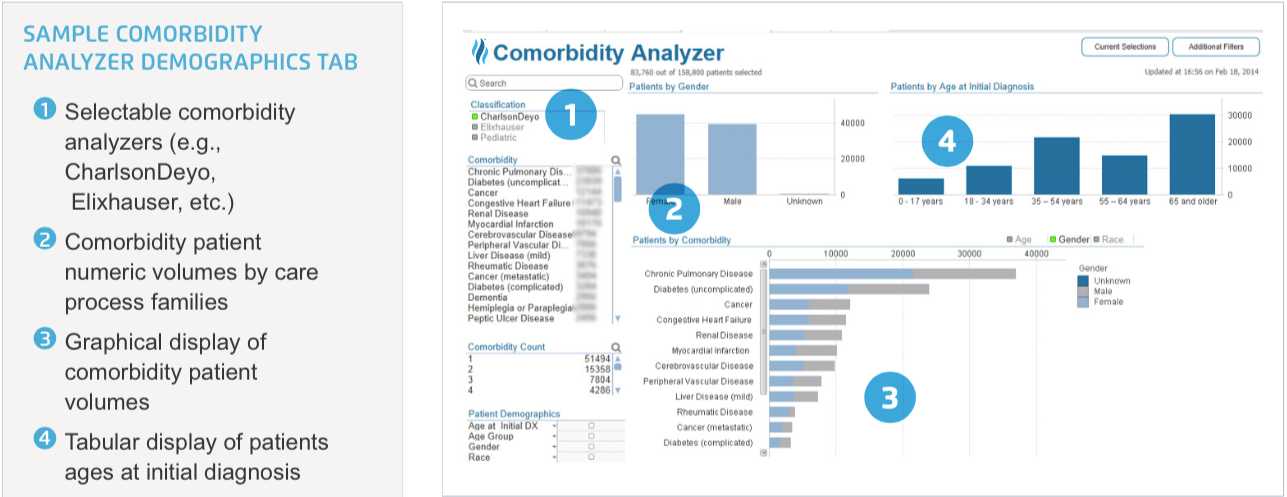
Both the payer and Crystal Run are pursuing the same objective of delivering higher quality care at a lower cost. Crystal Run now has leverage to justify a higher per-patient-per-month care management fee to enable investment in the care infrastructure—for example, to hire more care managers to help coordinate better care—which enables the group to deliver more effectively on that joint objective.
Crystal Run wants to ensure that the organization’s compensation framework is properly aligned with the actual patient care that a physician delivers on a day-to-day basis. This requires an accurate accounting of the volume and risk of sub-specialty work. The ACO is using the Health Catalyst foundational analytical applications to help answer these important questions. These analytical applications can easily identify patient populations with specific characteristics including demographics, diagnosis, lab, medications, procedures performed, etc. For example, a breast surgeon who also does general surgery can be more accurately bench marked based on the volume of breast surgery she performs as compared to general surgery and also on the risk profile of the patients she serves. Aligning physician compensation with their actual work effort in this way not only ensures that personnel costs are properly matched to the clinical costs; it also helps physicians feel fairly compensated and improves their satisfaction and retention.
Crystal Run is using the EDW and analytics applications to tackle a variety of population health management issues.
Quality Improvement and Physician Engagement
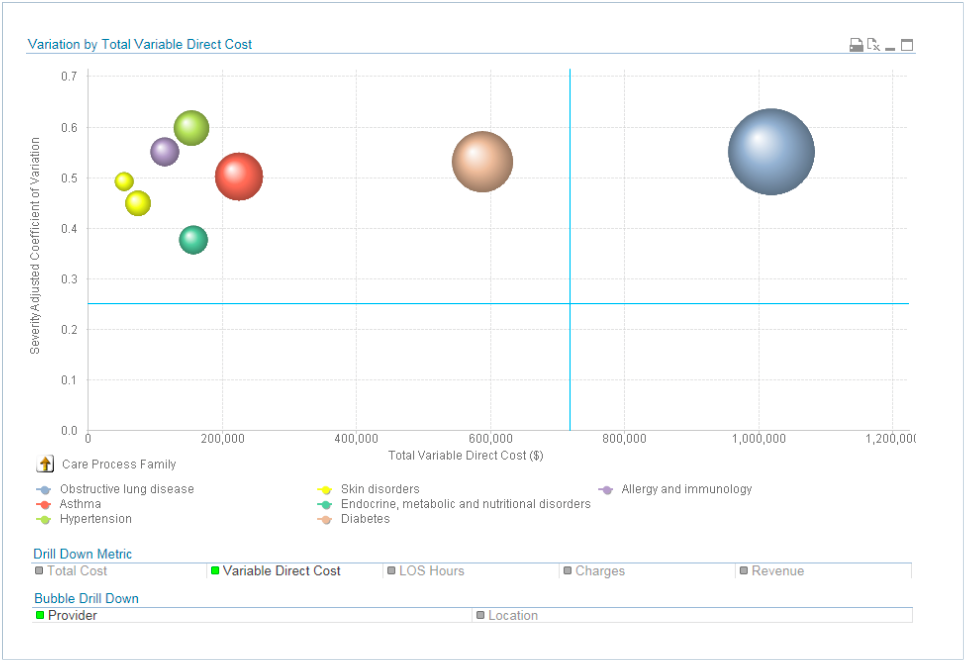
The ACO uses the Health Catalyst Key Process Analysis (KPA) application (Figure 4) as an important component of its initiative to reduce inappropriate clinical variation. Their objective is to remove inappropriate variation from specific clinical processes in order to ensure patient care aligns with best practices. Using the KPA application, Crystal Run easily identifies clinical areas that display high variation. The application enables them to quickly visualize variation rates stratified by physician and adjusted by risk to pinpoint the biggest opportunities for improvement. This process enables the organization to prioritize variation reduction initiatives.
Increased revenues through population health management leadership
Crystal Run leveraged the Population Explorer and Cohort Builder applications to justify an exception they hope will qualify them for the Centers for Medicare and Medicaid Services’ Innovation DSRIP (Delivery System Reform Incentive Payment) grant. New York State had received a waiver from the federal government to decrease Medicaid spend and use that money to reinvent the system and deliver more efficient care for Medicaid beneficiaries. The waiver allows the state to reinvest $8 billion into community-level collaborations that focus on system reform.3
The focus of the grant was on regional ACO formation for Medicaid and uninsured patients; however, as a private practice, Crystal Run was ineligible to apply for the grant. Although Crystal Run as a practice did not exceed the 35 percent threshold for Medicaid and uninsured visits, by using Population Explorer and Cohort Builder—individual specialties and individual providers were found to surpass this threshold—allowing Crystal Run to apply for a waiver to be included in the funding for the grant program.
This data, organized by county and region, was submitted to CMS to demonstrate that an eligibility exception should be made for Crystal Run, potentially providing the ACO with additional revenues which can be used to deliver improved population health management for its community.
Improving the accuracy of the annual budgeting process
Crystal Run is using the EDW to inform a seasonally adjusted budget. In 2014, Crystal Run experienced a profound negative financial effect from snow days that impeded the ability of patients to come in for care—roughly 16,000 patient visits did not occur. The resulting disruption to business continuity and financial downslide necessitated a more proactive and accurate seasonal budgeting strategy and physician productivity plan.
With the EDW, Crystal Run analyzed the data to determine the number of patients who would be seen per year in the absence of snow. Using this as their annual forecast, they designed an individualized budget for each physician, designed to help the physician make his own decisions about how to manage anticipated missed visits during the snow season, ensure patients receive the care they need and stay on budget for the year. This more accurate, seasonally adjusted budget and productivity plan—driven by data—helps ensure that patients who need care will be seen during the months of severe weather and allows physicians to better balance their professional and personal lives.
Crystal Run estimated the amount of time it would have taken using legacy analytics solutions to conduct some of the ACO’s clinical and operational analyses discussed above. The Health Catalyst solution demonstrated significant time savings compared to that estimation:
The Cohort Builder and Comorbidity Analyzer application are driving a more effective way of negotiating with payers on risk-based contracts. Analytics delivers transparency around the financial risk associated with the ACO’s patients—including comorbidities and risk profiles. Crystal Run is now able to bring new information to the table to drive more data-focused and accurate conversations, which enables them to capitalize on each shared-savings and risk contract and to negotiate appropriate per member per month rates.
Crystal Run is now able to better prioritize its clinical variation initiatives. Now, at quarterly multi-specialty meetings, the priority areas identified with the KPA application are discussed with providers serving a specific domain, such as diabetes care. These physicians then are given ownership in the development of best practices and are accountable for making changes in their individual practice to better align with evidence-based medicine. Ultimately, this alignment on best practices will result in less variation in care and lower costs.
“It is not just the delivery of care, but how to arrange for care delivery that we have to consider if we want to succeed as an ACO. We are doing a lot of ‘what if’ analysis now that we could not do before: Which patients go to a certain office? Are they sicker in one area as opposed to another? Answers to these questions help us arrange care to meet our population’s needs. We are becoming a medical logistics organization, and advanced analytics makes it possible.”
– Greg Spencer, MD Chief Medical Information Officer
With its goal to move as quickly as possible to value-based care, Crystal Run has applied to the state of New York for a health maintenance organization (HMO) license, which will enable the ACO to become a health plan (the “Crystal Run Health Plan”). Creation of this health plan will allow Crystal Run to be fully accountable for their care over long periods of time. Crystal Run anticipates launching the health plan in January, 2015.4 To manage the plan’s population effectively, drive quality improvement and lower costs, the ACO will continue to rely on the EDW to conduct robust operational analytics and gain critical clinical insights.