The U.S. healthcare system is costly yet underperforms compared to other nations. To improve efficiency and preventive care, Mission Health created the Mission Health Partners ACO for 40,000 patients, using an analytics application to automate data collection, resulting in improved performance across all 33 ACO quality metrics.
The United States healthcare system is the most expensive in the world, but data consistently shows the U.S. underperforming relative to other countries on most dimensions of performance. The Centers for Medicare & Medicaid Services’ (CMS’s) accountable care organization (ACO) model is aimed at addressing that issue by offering financial incentives for providers to improve the health of populations and reduce costs through greater efficiencies and a focus on preventive care.
Mission Health, North Carolina’s sixth-largest health system, recognized that the goals of ACOs were in alignment with its mission and formed a Medicare Shared Savings Program (MSSP) ACO called Mission Health Partners (MHP), which is responsible for 40,000 patient lives.
MHP knew that its manual approach to data collection and reporting would not be sufficient for the required ACO quality metrics. By leveraging a previously implemented enterprise data warehouse platform and implementing an ACO MSSP analytics application, MHP was able to automate the processes of data-gathering and analysis and align the data with ACO quality reporting measures.
The U.S. healthcare system is the most expensive in the world, but data consistently shows the U.S. underperforming relative to other developed countries on most dimensions of performance including overall life expectancy. In an attempt to decrease the cost of care while improving the health of Americans, CMS launched multiple demonstration projects, several of which were variations of a new model of providing care called an Accountable Care Organization (ACO).
ACOs are groups of doctors, hospitals, and other healthcare providers who come together voluntarily to provide high-quality care while reducing unnecessary costs for their Medicare fee-for-service patients. One model, the Medicare Shared Savings Program (MSSP) ACO, facilitates coordination and cooperation among providers to improve the quality of care by focusing on quality performance. Traditional healthcare fee-for-service models reimburse providers only when a patient is sick. MSSP ACOs offer financial incentives for providers based on performance on specific quality metrics.
Like many health systems across the country, Mission Health, North Carolina’s sixth-largest health system—with five hospitals, numerous outpatient and surgery centers, and more than 1,000 employed physicians—decided in recent years that the time was right to embrace the ACO model. Recognizing the alignment between the goals of ACOs and its mission to provide world-class care to patients and their families when they need it most, Mission formed a Medicare Shared Savings Program (MSSP) ACO called Mission Health Partners (MHP) in 2014, which is now accountable for the cost of care for more than 40,000 Medicare patients.
To participate in MHP, providers must agree to follow specific standards of care set by the ACO. These standards promote more coordinated and better care for patients, especially those with chronic illness. As an MSSP ACO, MHP is eligible for financial incentives from CMS for meeting specified goals related to performance on MSSP quality metrics. Before any ACO can share in any savings generated, it must demonstrate that it met the quality performance standard for that year.1 In 2015, CMS required ACOs to report on 33 quality measures spanning four quality domains: Patient/Caregiver Experience, Care Coordination/Patient Safety, Preventive Health, and At-Risk Population.2 In order for MHP to successfully monitor, achieve, and report these quality measures, it needed to establish a solid infrastructure, including an innovative approach to real-time analytics.
MHP leaders knew that in order for the ACO to achieve successful outcomes, ACO metrics performance data needed to be accessible and visible, and barriers to improving ACO metrics needed to be identified and addressed. The ACO was essentially starting with a blank slate when it came to timely access to reliable, objective measures of physician quality. Before the creation of MHP, Mission relied on Physician Quality Reporting System (PQRS) reports to measure provider quality, but the performance data was delayed, only available periodically on a static report, and considered grossly inaccurate by physicians due to problems with physician attribution and data integrity. In addition, while Mission had a system of physician incentives for employed physicians based on quality metrics, the metrics were not necessarily aligned with performance on the ACO measures.
When MHP initially formed, accessing data tied to the 33 ACO metrics was limited, and obtaining any information required significant manual effort. In addition, changes in metrics specifications or clinical practice changes, which occur fairly often, would often go unrecognized. When and if they were identified, the data extraction process would need to be adjusted and the report rebuilt before the performance metric would be accurate again.
Besides needing this information for Medicare patients to report to CMS for MHP, Mission needed reliable performance information about all patients, by provider, group practice, and payer to strategically set physician incentives for all of its employed physicians, and to more effectively negotiate at-risk contracts with third-party payers. In order to meet all of these information requirements, an analytics solution was needed that could pull data together for, as well as differentiate between, independent and employed providers and practices, and ACO and non-ACO providers and practices. This task was further complicated by the multiple different data sources used by employed and independent practices.
While improving any quality metric is inherently complex and presents multiple challenges, improving performance within the diverse clinic environments that make up an ACO is even more difficult. For MHP, clinic workflows, which were not standard across the ACO, rarely incorporated key components of the 33 ACO metrics such as screenings for fall risk and depression. Not only were these screenings and tools inconsistent across physician practices, but all practices struggled with documenting the screening results. The complexity of information and the lack of integration of the data systems, particularly between employed and independent practices, made consistent process development challenging even when there was agreement on what needed to be done.
In addition, providers and clinic staff lacked knowledge and awareness about ACO quality measures and how to address them—a challenge further complicated by a lack of timely data to help drive change. The manually compiled reports were static and only ran monthly, which made it nearly impossible for a practitioner to identify patients affected by a measure and intervene in a timely manner to provide recommended care. The providers’ ACO performance data were months behind, which made it difficult to identify and focus efforts on problem areas to improve performance. Individual providers and group practices had difficulty judging how well they were doing because they couldn’t see their results in relationship to their peers or national benchmarks.
When Mission leaders decided to form an MSSP ACO, they knew they would need to quickly implement an analytics solution that could provide ready access to the data needed for MHP to report the 33 ACO quality metrics to CMS. The solution also needed to address Mission’s needs for managing the performance on quality metrics for all employed physicians.
Providing Access and Visibility to ACO Metrics Performance Data Mission had previously implemented an enterprise data warehouse platform (EDW) from Health Catalyst that aggregates clinical, financial, operational, and other data sources. The EDW served as the basis for automating the previously manual processes of data gathering and report creation for ACO metrics, with the addition of the ACO MSSP Measure analytics application (see Figure 1).
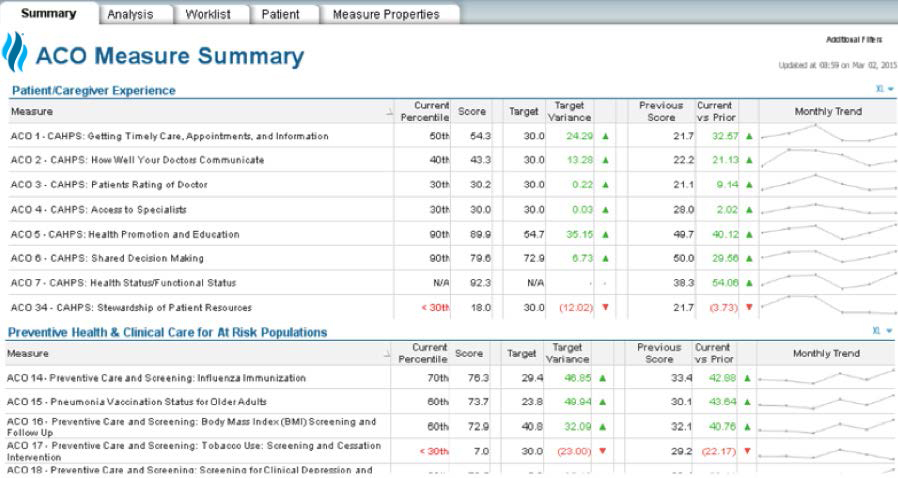
This application enables a much more complete, accessible, and interactive source of information that is reliably built to align with the data specifications for the ACO quality measures, eliminating the need for manual data-gathering. Changes in metrics specifications or clinical practice changes that affect the data sources for metric calculations, which were previously a major obstacle, can now be identified and quickly addressed due to the increased visibility of the data and the electronic nature of the data extraction process. The application also provides visibility and access to performance on the ACO measures for all of the health system’s patients regardless of payer, thus providing the reporting flexibility needed to support Mission as well as MHP.
The consistency, visibility, and accessibility of the performance data through the application are a distinct improvement over the previous attempts to use PQRS reports or the internal manual reports as a source of quality metrics. Physicians are much more accepting of the data due to greater consistency and improved accuracy. The data provided by the application are now the primary driver for physician quality incentives not only for physicians who are part of the ACO, but for all employed physicians. The transparency of the information allows physicians to see where they stand compared to their peers. This has driven change by engendering healthy competition and has led to overall quality improvements.
The application provides a number of benefits, including the ability to filter data by payer, physician, and practice, which provides key strategic information about performance on quality metrics that can be used to inform negotiations for risk-based contracts with third-party payers. When building the application, it became clear that
MHP’s ambulatory and employed physician groups had a clearer path between the data in the electronic medical record (EMR) and the ACO metrics than MHP’s independent practices did. Because of the more reliable data connection available to employed providers, the utility of the application and the expectations of their use of it are more robust than for the independent practices in the ACO. The goal for the employed group was real-time visualization of quality performance data across the employed group network and patient lists with actionable data to drive improved performance.
Due to the lack of direct access to raw data for the independent practices, a separate dashboard was created that is dependent on less robust information such as meaningful use reports that are uploaded into the EDW. Adding another layer to the challenge, the EMR reporting capabilities and clinical accuracy are very poor for the independent practices, leading to less consistency, reliability, and actionable information than that experienced by the employed physicians on the health system’s standard platform. Therefore, the goals for the independent practices are more modest, focused on encouraging them to review the data for peer-to-peer comparisons to drive quality improvements.
MHP’s practice managers and clinical leaders (typically the RN supervisors in each practice) are responsible for monitoring the performance of their practices based on data from the application and key metrics. Performance issues can be identified in near real-time, allowing for immediate process changes that can have a positive impact right way, rather than waiting for delayed feedback they used to get from their previous reporting methods.
One of the most powerful benefits realized from the improved access to information provided by the application has been the ability to obtain provider- or practice-specific patient lists behind the measures that identify which patients are in need of a particular test or screening or that require interventions based on specific clinical indicators. This capability gives practices actionable information they can use to prioritize patient care and improve quality measure performance. The data allows managers to monitor the impact of improvement efforts and identify weak spots in operations. Issues such as workflow problems or technical barriers to completing screenings can now be easily identified and addressed.
MHP and Mission took several steps to engage and support providers and clinic staff as they learned the importance of the quality measures. When new processes were developed, education and tools were provided to the providers and their clinic staff through an internal website that included toolkits, podcasts, order sets, protocols, and algorithms. Clinical teams also had access to a smartphone app with the metrics definitions and scorecards in PDF format. In addition, higher performing providers were encouraged to share best practices and were available for consultations. Leaders also communicated frequently via newsletters, emails, and reports at regularly scheduled meetings.
When the application came out, the metrics revealed that one physician was in the 20th percentile for falls screening of eligible patients, one of the ACO quality measures. He began having his medical assistant (MA) do fall screenings over the phone, and the physician went from the 20th percentile to now over the 90th percentile in fall screening, simply by changing the workflow and leveraging support personnel and the patient list provided via the application in a real-time fashion. That is something the practice did not have the capability of doing effectively before the data were available from the application.
Learning from the provider’s experience, the ACO leadership shared this story with their members and recommended standardizing workflows to empower MAs to initiate the screening process for the preventative care measures. In the recommended workflow for all of the screenings, the MA owns the recommendations for screenings, and has the initial conversation with the patient. The MA may recommend mammograms, colonoscopies, etc., based on standing orders; whenever possible, screening tools are standardized and built into the EMR. MAs are educated on how to perform and use the screening tools and the action that should be taken for positive screenings, and providers receive training on what interventions to initiate for patients with a positive screening.
Some of the screenings were more difficult to effectively implement than others. Improving colorectal screening rates required additional innovative interventions. Although screening colonoscopies are recommended for people older than 55 years, many patients choose not to undergo them. For those patients, MAs were instructed to offer simpler alternative testing such as the fecal immunochemical test (FIT) or the fecal occult blood test (gFOBT), which could be performed at home and mailed in. For ease of ordering, these screening alternatives were added to the order set. In addition, MHP created a workflow enhancement that automatically “checked” a box to satisfy the ACO quality measure when the results of the mailed-in
tests were documented by the lab.
MHP needed a similar multi-step approach to drive depression screening rates, one of the newer ACO requirements. The Patient Health Questionnaire (PHQ2) depression screening tool was selected as the standard and built into the EMR. The screenings brought some unexpected results that required creative solutions.
As a result of increased depression screening, the need for additional patient interventions was uncovered and more patients needed follow up by providers. Mission worked to build capacity for the providers to respond to positive depression screenings by implementing “curbside” consults with psychiatrists, where a provider may submit a case electronically for review and recommendations. Mission also developed additional protocols for referrals and follow up based on the screening results.
MHP’s experience demonstrates how an MSSP ACO can be successful in improving performance with visible, actionable data coupled with a focus on providing the best quality care for patients.
This focused approach has resulted in subsequent improvement in all 33 of the 2015 ACO metrics. Specifically, key outcomes have included:
The ability to monitor near real-time performance on quality metrics also has allowed MHP to identify when performance is below thresholds for payer incentives tied to quality performance measures. In just one example, with a financial incentive of over $1 million dependent on whether MHP met its metrics, the ACO was able to institute daily data updates to monitor progress toward goal on a real-time basis. Due in large part to that ready access to near real-time data to closely monitor its progress, MHP successfully earned the seven-figure financial incentive from a third-party payer.
In addition, the automation of Mission’s cumbersome manual processes resulted in improved efficiencies for both the health system and MHP:
“For each number in a dashboard, there’s a patient list behind that. With the analytics application, it’s about two clicks to access the patient information behind the numbers in a report. It’s all there in one place now, and it’s standardized across the system.”
– Rex McWilliams, CIO, Mountain Area Health, Education Center (MAHEC)
MHP leaders have found that where tight workflows are in place, and an ACO quality measure is not provider dependent, it is easier to be successful in meeting the measure. They will continue to look for opportunities to leverage the contributions of support staff such as the role MAs have played in increasing preventive screening rates. Leaders say they believe that the higher rate of important preventive screenings is leading to earlier interventions for conditions that could improve patients’ health in significant ways, resulting in better outcomes and better care for patients. They will be monitoring outcomes data to determine if this assertion is proven correct over time.
Leaders have recognized that ACO performance metrics are inherently more challenging to impact than process metrics due to their complexity. They will be sharing best practices and their internal successes to help other practitioners do better. Mission continues to tackle and work through these barriers by optimizing its EMR system, tightening workflows, and managing manual extraction in the few cases where it is still needed. Leaders also plan to continue to drive improvements in measures and outcomes; develop more protocols to support best practices; consider telemedicine to expand provider capacity; and analyze the impact of metrics on mortality and readmissions.