Cost challenges in healthcare are threatening the future of many healthcare organizations and their ability to effectively care for patients. Read how UPMC took on these challenges by partnering activity-based costing and service line operations to gain insight into cost and clinical variation.
Healthcare costs continue to increase at a disproportionate rate relative to gross domestic product, and Americans are becoming increasingly aware that they aren’t getting their money’s worth. Lack of understanding about how much it costs to provide patient care, and lack of knowledge about how those costs compare to the outcomes achieved, lead to the cost increases. To build sustainability, healthcare organizations must identify and address waste in healthcare and reduce the total cost of care.
UPMC recognized that the common denominator to addressing threats to sustainability is to fully understand and effectively manage costs. It implemented activity-based costing (ABC) by utilizing PowerCosting™, an application that leverages Health Catalyst's analytics platform and best-of-breed, activity-based costing models to deliver accurate and actionable data. The application delivers detailed and actionable cost data across the analytics environment, and supports service line reporting, contract modeling, and clinical process improvement. UPMC has used this capability to effectively drive cost savings and improve clinical outcomes in many of its service lines, including Surgical Services, Women’s Health, Orthopedics, and Cardiovascular.
Through its analytics platform and best-of-breed, ABC models, UPMC is improving quality and safety, reducing costs, and increasing value across service lines.
Healthcare costs are climbing disproportionately to gross domestic product (GDP), and are predicted to account for 19.9 percent of GDP by 2025.1 This spending is exorbitant, and Americans are becoming increasingly aware that they aren’t getting their money’s worth. Healthcare outcomes lag those of other developed countries, while over $700 billion of healthcare spending is considered waste. Major factors contributing to increased healthcare costs are a lack of understanding about how much it costs to provide patient care, and a lack of knowledge about how those costs compare with the outcomes achieved.2
Meanwhile, the average hospital operating margin is 2.2 percent, ranging from 3.9 percent for hospitals with AA credit ratings, to -1.4 for hospitals with BBB ratings.3 Addressing margins this tight requires accurate data to effectively navigate the path between profit and loss.
For the American healthcare system to be sustainable, healthcare organizations must be able to identify and address waste in healthcare, and reduce the total cost of care. To create these internal efficiencies, hospitals must have timely and actionable data that can identify unnecessary variation in care routines and supply usage, and enable appropriate corrective action.
Healthcare reimbursement is being driven by growth in government programs, changes in employer plans, and growth of alternative payment models, requiring hospitals to shift their revenue strategies from volume to value, and improve patient outcomes at a lower cost. Exacerbating this challenge, payment system reforms will increasingly require providers to bear greater population-based financial risk.
Price transparency is critical in this new healthcare environment to effectively manage payer contracting, but to provide this information, hospitals need reliable and defensible data.
UPMC is a large integrated healthcare delivery system with over 30 hospitals accounting for more than 6,000 licensed beds and 310,000 inpatient admissions and observation cases, in addition to 4.2 million outpatient visits, more than 4,000 employed physicians, and a UPMC Health Plan with 3.2 million members.
UPMC was aware that a changing environment required it to take on more risk, moving from payment for volume to payment for value. This forward-thinking healthcare organization began to analyze the industry and implemented a strategic and effective way to position the organization for success while improving care for patients.
UPMC determined several underlying problems making the current U.S. healthcare system unsustainable:
UPMC recognized that the common denominator to addressing these threats to sustainability is the ability to fully understand and effectively manage costs—knowledge that is essential to eliminate waste and improve patient outcomes, both of which are made possible by eliminating unnecessary clinical variation. UPMC’s approach to success centered on expanding its analytics capability and implementing an advanced costing system that would provide insight into both cost and clinical outcomes.
UPMC determined that the traditional cost accounting methods used most often in healthcare—relative value units (RVU) and ratio of costs-to-charge (RCC)—did not provide the level of detail and accuracy necessary to inform decisions that would enable it to overcome industry threats to its sustainability.
Activity-based costing (ABC), used in manufacturing for decades, has been deemed impossible or not worth the effort in healthcare due to challenges with data integrity, integration, and access. UPMC overcame these technological challenges by using PowerCosting, which leverages Health Catalyst's analytics platform and best-of-breed ABC models to deliver easily accessible, reliable, integrated, accurate, and actionable data.
Several key differentiators define this advanced ABC system:
PowerCosting includes data from a variety of sources (EHR, patient accounting systems, general ledger, HR and payroll data, supply chain, pharmacy, etc.), which makes it possible to assign direct costs, such as medications, supplies, and labor costs to patients based on their actual utilization. UPMC allocates remaining expenses to patients using the best available driver, such as minutes in the operating room, time on the MRI machine, or scheduled minutes for a procedure.
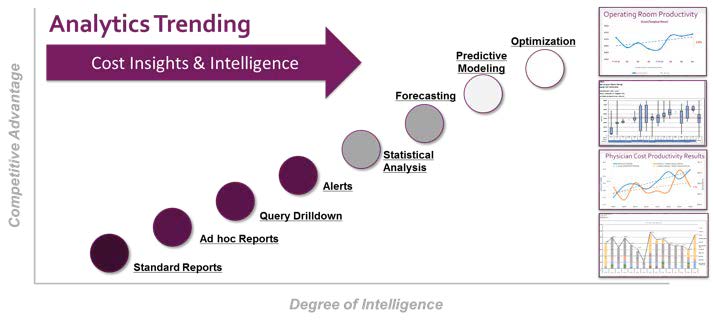
Detailed and actionable cost data across the analytics environment supports service line reporting, contract modeling, clinical process improvement, and more (see Figure 1), enabling UPMC to do the following:
UPMC has used analytics to effectively drive cost savings and improve clinical outcomes in many of its service lines, including Surgical Services, Women’s Health, Orthopedics, and Cardiovascular.
A good example of how UPMC leveraged analytics to successfully improve both clinical and financial performance is its approach to surgical services.
In the current healthcare environment of declining surgical volume and increasing cost, it has become imperative for any health system to gain solid, data-driven insight into its use of operating room (OR) resources. One of the largest areas of opportunity is the efficient deployment of OR labor, both anesthesia and hospital staff, in reacting to changing volumes. Using cost allocation methodologies developed with Health Catalyst, UPMC sought to understand the correlation of labor costs for anesthesia and hospital resources to surgical case time, which resulted in a transparent view of labor cost per OR hour across the system. By understanding the intersection and interaction of volume and cost, UPMC has been able to identify operational variation within and across facilities.
As a result, operational and physician leaders have regular insight into the changing cost and volume associated with each OR. Data is actively used to identify best practices related to OR utilization and staffing to deliver the same high-quality patient care, using fewer resources.
To improve the clinical outcomes of UPMC’s patients, perioperative and surgical services teams actively worked to implement the protocols related to the nationally recognized Enhanced Recovery After Surgery (ERAS) program. ERAS protocols are designed to reduce surgical stress and maintain post-operative physiological function, reduce rates of complications, facilitate faster recovery through early ambulation and feeding (thus reducing LOS), and improve patient/family satisfaction.
By prioritizing these clinically meaningful interventions for resource allocation supported by the insight provided by its analytics platform, UPMC was able to increase the utilization of clinically meaningful practices—while eliminating non-value-added practices—to improve both clinical and financial outcomes.
As fee-for-service reimbursement models transition to alternative payments, providers are increasingly held accountable to deliver high quality, value-based care. One such alternative payment model is the CJR program, which aims to provide coordinated, high quality, cost-efficient care during and after a hip or knee replacement surgery. To achieve these objectives, the model aligns quality, outcomes, and cost data to help support better and more efficient care pathways for patients.
When UPMC implemented the CJR model, it leveraged the combination of financial and clinical leadership provided by its Orthopedics Service Line structure, and the detailed information about cost and clinical variation from its analytics platform. Guided by this information, the combined efforts of quality, operations, physicians, and finance have driven improvement in multiple areas, including clinical practice change and supply utilization, ultimately providing better care at a lower cost with a greater degree of patient satisfaction.
Through use of the analytics platform and best-of-breed, ABC models, UPMC is increasing value by improving quality and safety, and reducing costs. UPMC now has accurate, actionable, defensible data that is helping the organization successfully change from volume to value.
Results from Surgical Services include:
The impact on orthopedics related to the CJR program has produced the following:
Enhanced transparency toward identifying practice variation for specific procedures has also improved performance in other service lines, such as:
Additionally, enhanced validation of source data has simplified ongoing maintenance, and the automated and improved cost allocation algorithms have helped shorten the closing process, simultaneously saving time and improving data integrity.
"This ABC system can be implemented in 6-12 months, and the ROI is exponential."
- Rob DeMichiei, Executive Vice President and Chief Financial Officer, UPMC
UPMC will continue to leverage its cost accounting system to inform and improve operations of its clinical service lines and general operations. Using this information to improve contracting will enable UPMC to continue providing excellent patient care and improving patient outcomes.


In surgical services:
In orthopedics related to the Comprehensive Care Joint Replacement (CJR) program: