Acuitas Health supports healthcare organizations interested in succeeding in value-based care by providing care management and analytics expertise. The organization faced challenges identifying individuals and groups who could benefit from their services, hindering program growth. To enhance efficiency, Acuitas deployed the Health Catalyst® Patient Intake and Care Coordination applications alongside the Health Catalyst Data Operating System (DOS™). This approach allowed Acuitas to achieve rapid results, successfully implementing the tools and generating value in under 60 days.
Data-driven decisions and analytics are critical for organizations and physician practices transitioning to value-based care, although many organizations struggle with measuring the effectiveness of these population health initiatives.
Acuitas Health works with healthcare organizations interested in succeeding in value-based payment arrangements and provides the necessary expertise and resources in care management and analytics to successfully deliver high-value healthcare. Its integrated care management teams have substantial skill and experience, yet found it challenging to identify which individuals and groups could benefit from the services the care management team could provide. As a result, the care management program could not be effectively scaled, limiting efficiency and continued program growth.
To obtain sophisticated, actionable analytics and automate processes, Acuitas deployed the Health Catalyst® Patient Intake and Care Coordination applications concurrent with beginning the implementation of the Health Catalyst Data Operating System (DOS™) platform. Acuitas meets the needs of its customers through a sprint to value—going faster than the typical time to value. The concurrent implementation approach used in this roll out set the pace for that sprint to value. In less than 60 days, the organization successfully implemented these tools and began receiving value.
An increasing number of provider groups are taking on risk for the total cost of care, and using care management programs to target high-risk, high-cost patients. The most successful care management programs use customized approaches to local contexts and caseloads, use qualitative and quantitative methods to identify patients, and consider care coordination as a key role. They also build trusting relationships with patients and primary care providers, match team composition and interventions to patient needs, and use technology, data, and analytics to enable effective care management.1
While data-driven decisions and analytics are critical for organizations and physician practices attempting to thrive under value-based care, many organizations struggle with measuring the effectiveness of their population health initiatives.2
Acuitas Health is a population health services company that empowers physicians to make the transition to a value-based care delivery system. Practicing medicine in a model where physicians are financially rewarded for improving the quality, while reducing the cost, of care they deliver to patients, allows for the introduction of innovative care models that improve outcomes. Its rich complement of care management staff provides medical care management for patients with multiple complex medical problems, behavioral health needs, and psycho-social challenges.
To be successful in its mission to empower physicians making the transition to a value-based care delivery system and preserve the independent practice of medicine, Acuitas needed to ensure it was engaging the right patients and investing the proper resources to improve patient outcomes, drive down costs, and increase value.
Identifying the right patients and engaging them to achieve the greatest improvement in outcomes are among the biggest challenges in value-based healthcare, population health, and care management. Even with Acuitas’ integrated care management team’s substantial skill and experience, it was difficult to identify the patients in need of what this team could provide.
Data was available within the EMR but could not be readily accessed to inform risk stratification, nor could it be effectively used to make decisions regarding care team assignments or evaluate the return on investment. As a result, the care management program could not be effectively scaled, limiting efficiency and continued program growth.
Acuitas needed a solution that would enable it to combine its years of value-based healthcare expertise and proven processes to streamline and accelerate the population health management and value-based capabilities of its physician partners. Time to value was of the essence here. Acuitas meets the needs of its customers through a sprint to value—going faster than the typical time to value.
To accelerate the population health management and value-based capabilities of its physician partners, and to effectively and efficiently scale its care management program, Acuitas needed sophisticated analytics that could automate related tasks in real-time, supporting the care management team in proactively engaging patients. Acuitas opted for a fast-track approach, supporting its sprint to value, and quickly deployed two Health Catalyst applications: Patient Intake and Care Coordination concurrent with its implementation of the Health Catalyst Data Operating System (DOS) platform. This approach not only dramatically shortened the time to value, it also provided the opportunity for teams to evaluate the data that currently goes into the EMR, and the rationale behind the data collection, enabling teams to eliminate waste, gain efficiencies, and optimize their workflow.
Acuitas supported its team members in adopting the Patient Intake and Care Coordination applications by providing ample playtime in a sandbox while simultaneously focusing on team formation, role clarification, and team development. Patient Intake is used to streamline the processes for patient entry into the program, and assignment of patients to a care manager. It consumes algorithm-generated patient lists following Acuitas’ refinement of those lists based on chart review.
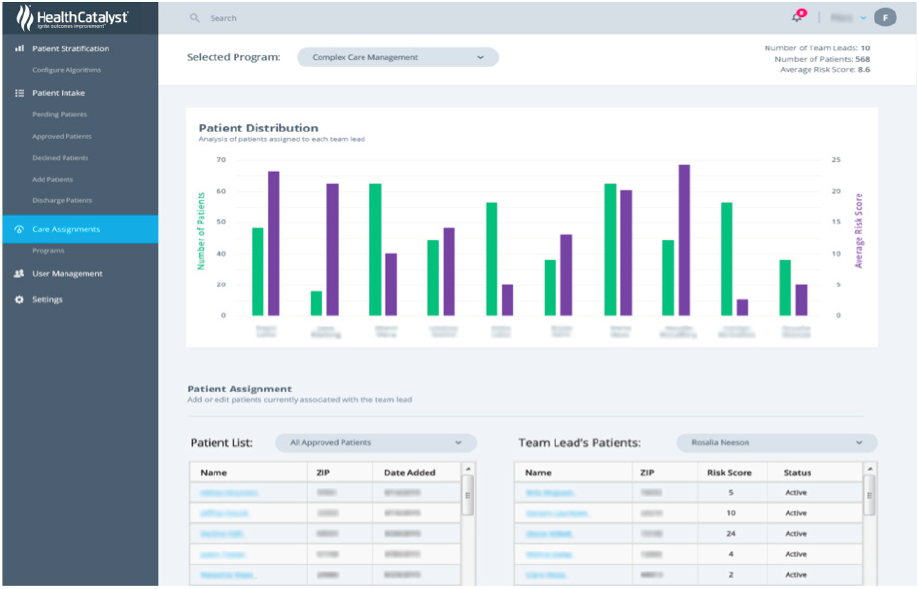
Following refinement of the patient lists, Acuitas assigns approved patients to the appropriate member of the integrated care management team using Patient Intake. The organization is then able to use the application to monitor patient distribution, ensuring equitable caseloads (see Figure 1).
Once patients are assigned, the integrated care management team employs Care Coordination, a web and mobile device application, to organize patient interventions.
Using Patient Intake and Care Coordination, integrated care management team members are able to capture data related to key processes such as:
Care Coordination allows integrated team members to monitor patients’ significant events, care plan activities, and appointments. The team is also able to easily communicate with other care team members associated with the patient and can manage new patient assessments and program enrollment (see Figure 2).

Acuitas, and its integrated care management program, use Patient Intake and Care Coordination to effectively monitor patient progress, in addition to payer statistics and geographic distribution of its enrolled patients.
In less than 60 days, Acuitas successfully implemented Patient Intake and Care Coordination concurrent with beginning the implementation of DOS, and the value is already visible. Acuitas is now able to:
“The care management solutions support us in improving patient outcomes and providing value to our physicians in an expedient way. At Acuitas Health, our purpose is to create the scale and space for providers of care to succeed in a value-driven environment with our integrated people, process and technology.”
– Keegan Bailey, MS, Strategy and Technology Leader, Acuitas Health
Acuitas plans to continuously expand its expertise, technology, and resources in practice intelligence, care management, and advanced analytics to support physicians in transitioning to value-based care. The organization will continue to integrate additional data sources and plans to use additional Health Catalyst Care Management Suite products, Patient Stratification and Care Team Insights, to help identify the individuals most likely to benefit from proactive care management and to evaluate the return on investment of its care management program (e.g., utilization, risk, costs, etc.).