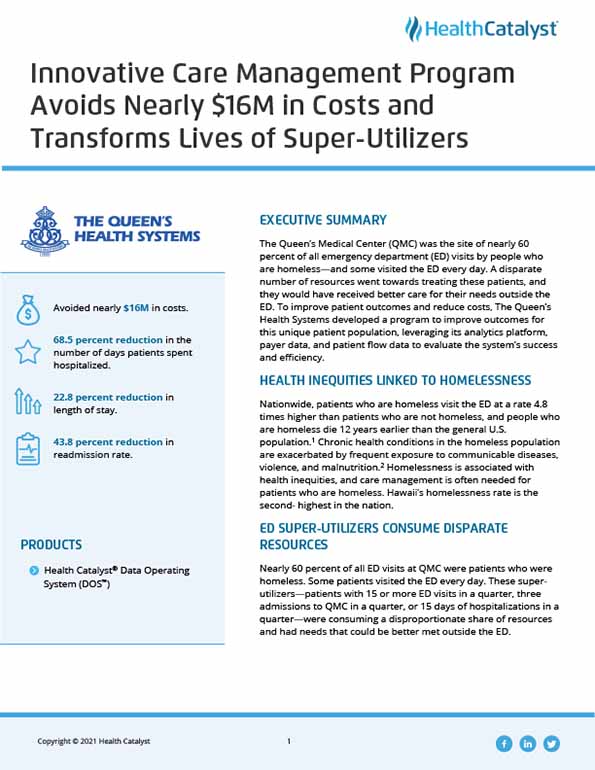
The Queen’s Medical Center (QMC) was the site of nearly 60 percent of all emergency department (ED) visits by people who are homeless—and some visited the ED every day. A disparate number of resources went towards treating these patients, and they would have received better care for their needs outside the ED. To improve patient outcomes and reduce costs, The Queen’s Health Systems developed a program to improve outcomes for this unique patient population, leveraging its analytics platform, payer data, and patient flow data to evaluate the system’s success and efficiency.
Nationwide, patients who are homeless visit the ED at a rate 4.8 times higher than patients who are not homeless, and people who are homeless die 12 years earlier than the general U.S. population.1 Chronic health conditions in the homeless population are exacerbated by frequent exposure to communicable diseases, violence, and malnutrition.2 Homelessness is associated with health inequities, and care management is often needed for patients who are homeless. Hawaii’s homelessness rate is the second-highest in the nation.
Nearly 60 percent of all ED visits at QMC were patients who were homeless. Some patients visited the ED every day. These super-utilizers—patients with 15 or more ED visits in a quarter, three admissions to QMC in a quarter, or 15 days of hospitalizations in a quarter—were consuming a disproportionate share of resources and had needs that could be better met outside the ED.
QHS had enrolled these patients into its programs for high utilizers but had not achieved the positive impact on patient outcomes, costs, and patient experience that it desired. The organization needed a new care management strategy that would allow it to respond to the needs of this unique patient population more effectively.
QHS developed the Queen’s Care Coalition, an innovative care management program, to address the needs of super-utilizers. In addition to utilization criteria, QHS screens patients for social determinants impacting health outcomes, including employment, food insecurity, housing instability, poverty, incarceration, and violence. When QHS finds patients with multiple factors influencing their health and wellbeing, it enrolls the patients in the care management program.
Community health workers (CHWs) first meet with these high-need, high-cost patients while they are in the ED or admitted to the hospital. After establishing trusting relationships, CHWs provide intensive, post-discharge navigation for these patients for 30 to 90 days. The CHWs withhold judgment of the patients they partner with and take a strength-based, harm-reduction approach to improving the patients’ health.
The CHWs meet patients face-to-face one to three times a week. Meetings can take place in parks, on sidewalks, and in homeless encampments—wherever the patient may be. CHWs work with patients to meet the goals and needs that are the most important to them. Patients are not required to stop using drugs to receive services and are not penalized or removed from the care management program for missing an appointment.
CHWs connect patients with medical and behavioral health services as well as services in the community to ensure patients receive the right care in the right place and prevent unintentional duplication of services. The CHWs schedule and attend medical, behavioral health, and benefit appointments with their patients; assist with financial and non-financial benefit applications; connect patients to low-barrier housing/shelters; and provide skills training to foster independence. When the patient is ready, CHWs perform a warm handoff to community partners. The CHWs check back in with patients for six months, reengaging with the patient if additional services are needed.
QHS leverages the Health Catalyst® Data Operating System (DOS™) platform for data and analytics. Housing status data for Queen’s Care Coalition patients is entered into the Instant Data Entry Application (IDEA), ensuring the data is readily available for analysis and reporting in DOS. The organization is able to use payer data, patient data, and patient flow data for ongoing program evaluation and data-informed decisions.
Queen’s Care Coalition is transforming lives while simultaneously decreasing utilization and costs. QHS achieved the following results:
One patient whose life was transformed by the Queen’s Care Coalition program had utilized the ED 16 times in three months with four hospitalizations. The patient had lived in a parking lot for 10 years and had a mental health diagnosis and history of substance abuse. He lacked connections to community resources and had refused mental health and substance abuse treatment. He was not consistently taking his prescribed medications.
QHS enrolled the patient in the Queen’s Care Coalition program. The patient’s CHW:
After three months, the patient graduated from the program. He remains housed, attends his medical appointments on his own, and takes all prescribed medications. He has not returned to the ED for more than two years.
"Queen’s Care Coalition has improved health equity and transformed lives. We have seen people who were homeless and routinely assaulted reshape their lives. They’re now living independently, going to their medical appointments, adopting pets—living full, healthier lives."
- Ashley Shearer, LCSW, CSAC, Manager, Queen’s Care Coalition
QHS plans to expand Queen’s Care Coalition and scale its program across the health system, expanding its reach and ability to transform more lives while also reducing healthcare costs.