Diabetes is a prevalent chronic illness among children in developed countries, and Texas Children’s Hospital aimed to enhance population health management for patients with diabetes, focusing initially on reducing diabetic ketoacidosis (DKA) incidents. The hospital formed a Diabetes Care Process Team (CPT) to standardize care and address variations in treatment and costs associated with DKA. By fostering collaboration, utilizing data for decision-making, and implementing effective interventions, the CPT has successfully improved health outcomes for patients with diabetes across all care settings.
Diabetes is one of the most common chronic illness for children living in developed countries. Texas Children’s Hospital in Houston is the nation’s largest pediatric hospital and ranked as one of the top four Best Children’s Hospitals by U.S. News & World Report. Hospital leaders wanted to take a more data-driven approach to population health management for patients with diabetes. They started by pursuing outcomes improvements related to diabetic ketoacidosis (DKA) since data from the EDW revealed that 64 percent of diabetes patients discharged had this life-threatening condition and there was measurable variation in costs and care for patients with DKA.
To reduce the variation, they formed a Diabetes Care Process Team (CPT). After the CPT achieved their initial goal of improving care for patients admitted to the hospital with DKA, they set out to implement larger improvements that would benefit the entire population of diabetes patients.
By empowering CPT members, leveraging data to drive decisions, and implementing new interventions effectively, the Diabetes CPT members have improved population health for patients with diabetes across all settings of care.
In 2012, 29.1 million Americans, or 9.3 percent of the population had diabetes. What’s even more troubling is that more than 200,000 of these Americans are under the age of 20.1 Diabetes is the most common life-threatening, chronic illness for children living in developed countries.2 Texas Children’s Hospital is a leader in the research and treatment of children with diabetes. The organization evaluates more than 2,500 cases annually with the goal of helping children, adolescents, and young adults to manage their illness effectively—and live long, healthy, and active lives.
Leaders at Texas Children’s wanted to take a data-driven approach to improving care for diabetes patients. However, they quickly recognized that EHR data alone would not be enough to inform their efforts. To access more clinical, financial, and operational data in real-time, Texas Children’s implemented the Health Catalyst Analytics Platform built using the Late-Binding™ Data Warehouse architecture (EDW). With this robust data now at their fingertips, the team used the Key Process Analysis application to determine that there was a measurable degree of unnecessary variability in care and costs associated with these patients, including increased length of stay (LOS) and readmissions.
Leaders at Texas Children’s wanted to take action to improve outcomes for patients with DKA, as well as the broader population of patients with diabetes. The improvement strategy encompassed four key initiatives:
Leaders at Texas Children’s decided to form a Diabetes CPT. CPTs are typically established for care processes that have a large population of patients, high degree of variation in care, measurable gaps in consistency and quality, and, importantly, organizational readiness to take on improvement efforts. However, forming the team was just the first step. The Diabetes CPT still needed experienced leadership, with a proven track record for using technology and clinical standards to facilitate data-driven process improvements. Dr. Rona Sonabend, Assistant Professor of Pediatrics, Pediatric Endocrinology & Metabolism, and Rhonda Wolfe RN, BSN, MBA, Assistant Director at Texas Children’s were the strongest candidates to lead the team.
Dr. Sonabend and Rhonda Wolfe, agreed to co-lead the diabetes CPTs, and understood that their teams would first solve the initial problems identified, and would then need to take on other challenges, continuing to improve care for patients with diabetes. The DKA improvement was a natural starting place but the teams wanted to ensure that the Diabetes CPT could expand their improvement efforts for the entire population of patients with diabetes, not just those admitted to the hospital for DKA. Understanding that the team desired to continue to grow and improve, the Diabetes CPT began its work—and within 1.5 years, opened a new Diabetic Care Unit for inpatients with DKA. Ultimately, the Diabetes CPT achieved every goal that had been identified—successfully decreasing length of stay, reducing variability, improving hospital throughput, and decreasing the readmission rate, all while improving patient satisfaction. The team’s early success in its DKA initiative served as the model for future improvements in care delivery for all diabetes patients.
To continue the forward momentum from the work on DKA, the Diabetes CPT identified core areas of focus to improve the care and outcomes for the diabetic patient population. In turn, this culminated in a comprehensive strategy for improvement, and five new CPTs designed to be co-led by a medical lead and an operational lead (see Figure 1) which report up through the Diabetes CPT.
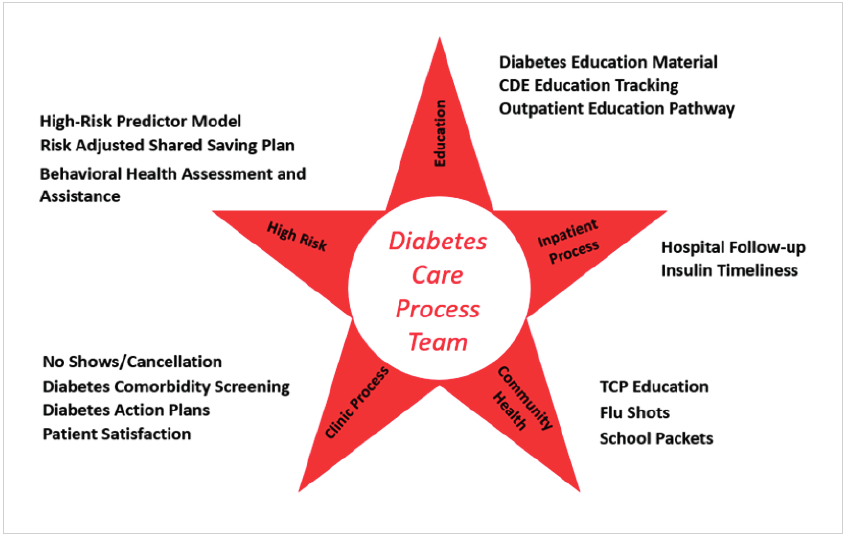
The new teams were designed to improve population health, reaching the entire population of patients with diabetes, including care providers in all settings. The interdisciplinary teams include everyone involved in patient care from parents and patients to those inside the hospital like physicians, nurses, and ancillary staff, and to those supporting patients outside of the hospital like school nurses and community based providers.
To be successful, the additional CPTs need to have strong leaders whose professional and personal passions are tightly aligned with the teams’ goals. That larger sense of purpose helps physicians and operational leaders to navigate the challenges of achieving and sustaining improvements. CPT leaders receive ongoing, in-depth training and development to ensure that they have the knowledge and skills to effectively implement quality improvement activities. Physicians who are new to quality improvement are also mentored by more experienced physicians.
CPT leaders also contribute to the work of the improvement teams. Rather than just running meetings and delegating assignments, team leads participate in tasks such as data validation, while still fulfilling their clinical and operational responsibilities. There is no hierarchy within the teams. All members contribute their ideas, share their expertise, and have equal representation which keeps them fully engaged and invested in outcomes improvement. Similarly, all team members regularly offer feedback, either appreciating other’s contributions or identifying areas for growth.
The five Diabetes CPTs meet independently every two weeks. During these meetings, the teams develop and refine their outcomes goals, generate ideas for Plan-Do-Study-Act (PDSA) cycles, and evaluate the effectiveness of their work. Every six weeks, the co-leads of the Diabetes CPTs meet to present their work, clarify questions, and align on goals. These conversations are critical to finding linkages with other teams and gaining consensus on proposed improvement plans. Team leaders not only celebrate each other’s big wins but also provide corrective feedback when necessary. This regular cadence of cross-team meetings fosters relationships and collaboration, helps to prioritize resources, and maximizes team efforts to benefit patients.
Texas Children’s uses a Modified Delphi process for the development of balanced score cards for each department that are aligned with the Institute of Medicine domains of healthcare quality (see Figure 2).

Each Diabetes CPT is responsible for establishing measurable improvement goals that align with the balanced scorecard. Each team also has a specific work plan to support those goals and the overall mission. The teams use data from the EDW to evaluate current performance and explore opportunities for improvement. By focusing on the data, and knowing that it’s a single source of truth, the teams are able to focus their discussions on what the data is telling them about their performance. After identifying the improvement opportunities, team members determine their priorities and focus on actionable activities. If a proposed change is necessary but cannot be completed for many months, team members place the item on hold and select something they can move forward on now.
To facilitate data-driven outcomes improvement, each team develops improvement goals that include the specific outcome goal (aim), balance measures, and timeframe for when the goal is expected to be achieved. The teams review national performance benchmarks while establishing goals, allowing them to evaluate how Texas Children’s performance compares to children’s hospitals across the country. Often, the team members discover that the organization’s performance is already higher than the benchmark. However, they also understand that the benchmark performance may not be adequate and frequently set goals that exceed national benchmarks. The CPT has the advantage of having a diabetes specific analytics application which is built on the EDW and capable of integrating information from multiple data sources. By integrating improvement goals into the Pediatric Diabetes Application, teams can quickly visualize and monitor progress towards these goals at every meeting.
Each goal must have an active PDSA improvement plan and defined interventions. The team is dedicated to achieving the desired improvements and heavily focused on activities that will improve patient outcomes. PDSA activities are also tracked in the Pediatric Diabetes Application so that the CPTs can evaluate the effectiveness of their interventions in relation to their goals (see Figure 3). Tracking both the outcome goals and the associated PDSA activities in one application helps teams to understand which interventions are effective and should be continued, as well as which interventions are not delivering results so should be discontinued.
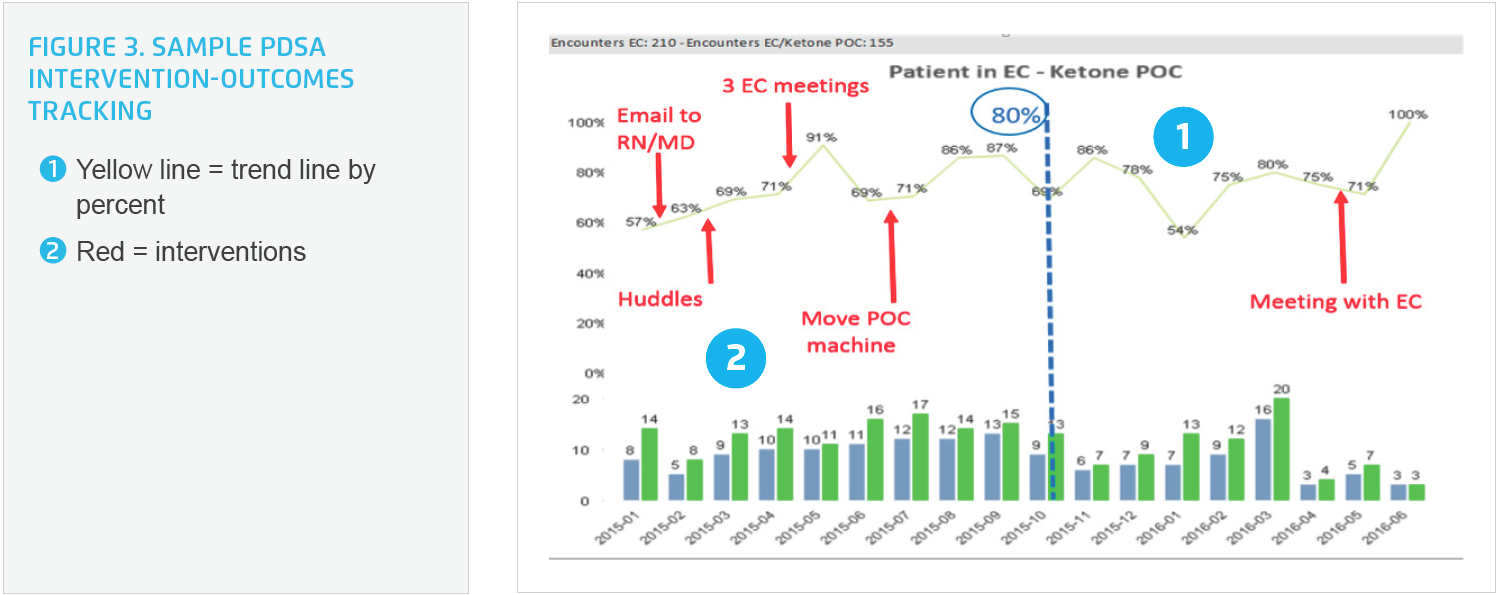
Most importantly, team members know that their work doesn’t stop once they achieve an outcome goal. They continue to monitor performance in the application to ensure that improvements are sustained. If performance slips, the team investigates why and then develops corrective action plans.
Effectively implementing changes and ensuring continued adoption is a pivotal component of successful quality improvement efforts. That’s why the CPT members move immediately into implementation once data demonstrates that a proposed intervention is effective and improves patient outcomes. They communicate the planned changes to key stakeholders, along with the data supporting the change and the expectation that teams adopt the changes in a timely manner. This commitment to data-driven action—both to identify and implement improvement opportunities—increases the speed and scale of improvements.
Team members also understand that while everyone wants to improve patient outcomes, change can be difficult. So, it’s vital to look for every opportunity to decrease the burden on end users by leveraging technology and automation. They design workflows to reduce, if not all together eliminate, the potential of not following the newly-established processes. Aligning evidenced based standards of care, decision support, automated alerts, and structured order sets with the existing workflow makes it easier for clinicians to do the right thing. As part of the ongoing improvement process, teams monitor the utilization of tools and how each component of the intervention impacts outcomes. If a step in the workflow or a tool does not lead to improvement, they re-evaluate options and may discontinue use of the tool.
Diabetes CPTs have improved population health for patients with diabetes across all settings of care, in multiple locations of care, and has successfully sustained these improvements. Below are a few of the most significant results with links to each of the individual CPT case studies for greater detail.
“Our patients already receive better care than they did five to ten years ago. We also know care will be different and better five to ten years from now. What’s most important is that we are no longer waiting for someone else to do this improvement work for us. We are diligent and focused about improving patient care from within the organization.”
– Rona Sonabend, MD, Assistant Professor of Pediatrics, Pediatric Endocrinology & Metabolism, Baylor College of Medicine
Dr. Sonabend and the Diabetes CPT members are confident that their data-driven quality improvement efforts have positively impacted outcomes for the entire population of diabetes patients. They are equally confident that outcomes will continue to improve because of their effective implementation of interventions and diligent monitoring of metrics on an ongoing basis. Having already achieved such impressive results, Dr. Sonabend and her teams have even bigger goals for the future, aspiring to transform the current model for care delivery and reimbursement system for chronic disease care. They believe that their demonstrated model for quality improvement should be used by others to enhance and improve care, and that these improvements should be financially-incentivized.