Allina Health is leveraging data and analytics to enhance clinical value, reduce costs, and improve patient outcomes. Through a systemwide process focused on identifying, measuring, and improving clinical value, the health system has uncovered nearly $33 million in potential cost savings and confirmed over $10 million in savings. This collaborative approach has also elevated discussions around cost concerns, leading to the development of standardized processes and a reduction in unwarranted clinical variation.
Today’s healthcare industry, in which a lack of insight into clinical variation has contributed to increased expenses, has significant opportunities to use data and analytics to improve outcomes and reduce costs. As part of its ongoing commitment to improve clinical value, Allina Health has employed a systemwide process to identify, measure, and improve clinical value. The health system has been able to quantify the value of clinical change work to improve outcomes, while reducing costs and increasing revenue for reinvestment in care.
Unwarranted clinical variation is responsible for 42 percent of wasted healthcare spending in the U.S. The bulk of variation at hospitals comes from just 16 percent of physicians.1 Most healthcare documentation is within an EHR, leading to a growth of clinical analytics, techniques for analyzing large quantities of data, and new insights from that analysis—a phenomenon known as big data. As a result, the industry has unprecedented opportunities to use big data in clinical opportunity analysis to reduce the costs of healthcare.2
A not-for-profit health system, Allina Health is dedicated to the prevention and treatment of illness, and enhancing the greater health of individuals, families, and communities throughout Minnesota and western Wisconsin.
Healthcare organizations must closely monitor margins to remain financially viable. Allina Health leadership recognized the need to focus more precisely on finding ways to fund its mission. As a large health system with limited resources, Allina Health was challenged to identify improvement opportunities to impact outcomes and reduce costs. Allina Health recognized that a lack of insight into clinical variation contributed to increased costs. Additionally, previous attempts to identify opportunities for improvement were not specific enough to target clear cost categories with the greatest variation.
As part of its ongoing commitment to improve clinical value, Allina Health employs clinical opportunity analysis—a systemwide process to identify, measure, and improve clinical value by quantifying the value of clinical change work to improve outcomes, while reducing costs and increasing revenue for enhancing patient care.
Clinical opportunity analysis identifies actionable opportunities to reduce cost. The Health Catalyst® Analytics Platform, including the Late-Binding™ Data Warehouse and broad suite of analytics applications, is a critical component of the Clinical Value Program used to identify opportunities.
Allina Health uses two pathways to initially explore potential opportunities:
Allina Health identifies and further refines potential opportunities with the following measures:
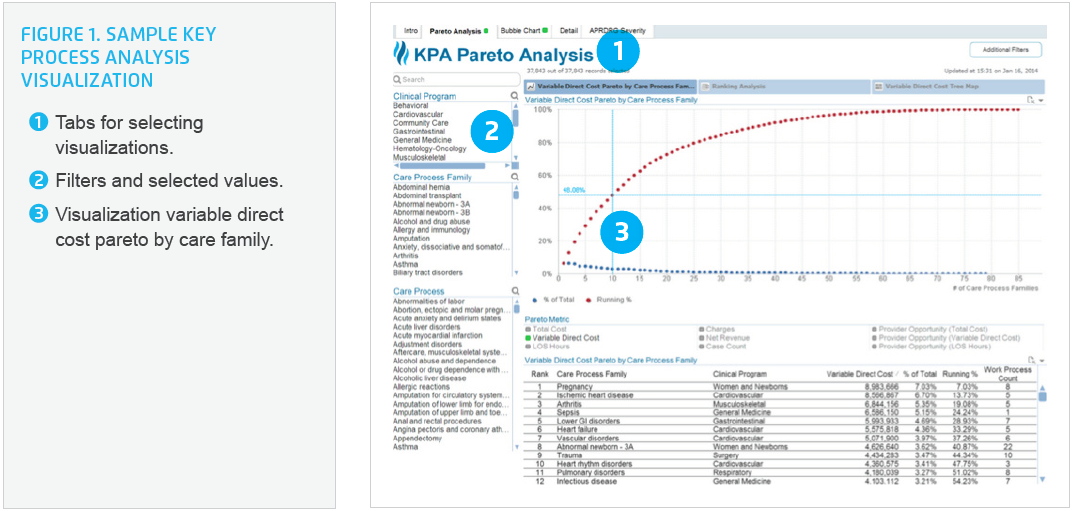
On a quarterly basis, Allina Health’s data analysts use the rich data within the analytics platform to identify undesirable variation in high-cost, high-volume clinical care processes. Leaders of the improving Clinical Value Program meet with the analytics team to select and assign areas of focus. The areas of focus could include service lines, facilities, types of services and events, literature reviews, or other identified areas of special interest. The analytics team then reviews, critiques, develops, and finalizes the opportunity analysis, and presents it to the Clinical Value Program team and clinical leaders.
The analytics team provides clinicians with suggestions on areas to dig into deeper, defines a methodology, and identifies where additional input from clinical expertise is needed. By involving clinicians and clinical leaders, Allina Health ensures correct clinical decisions, allowing it to address unwarranted variation.
Focusing the analysis on cost category levels, such as supplies, labs, pharmacy, radiology, therapy, room costs, and operating room costs, enables Allina Health to explicitly target areas of greatest clinical variation. Initially, the opportunity identification process focused primarily on inpatient cost variation. Allina Health has since expanded the opportunity analysis process to explore other revenue generating opportunities and cost savings areas, such as referrals, care coordination, and reducing total cost of care.
Allina Health reduces care variations by reducing outliers or shifting the mean:
For each opportunity, data analysts identify variation by developing an understanding of similarities or differences between populations. To understand true variation, rather than the perception of variation when comparing groups that are too dissimilar, Allina Health drills down to as homogenous of a clinical population as possible. To present a full picture of the variation and opportunity, analysts share their analyses visually—via bubble graphs and box plots—with Clinical Value Program members and clinical leaders. These graphs are used together to help guide improvement opportunity identification, and are presented in a consistent manner with each opportunity analysis.
The Clinical Value Program and clinical leaders use the information to develop quarterly plans for improvement projects targeting improved outcomes and decreased costs. The identified opportunities may or may not be acted upon right away. Items that are not immediately acted upon are retained in service line portfolios and are moved to the forefront when resources become available to focus attention on the opportunity.
Using a collaborative, data-driven approach to improve clinical value, Allina Health has achieved the following results:
“Providing our clinicians actionable data analyses has helped engage them in identifying opportunities for improvement.”
– Sarah Jenson MS, PMP, Lead Clinical Data Analyst, Allina Health
Allina Health plans to continue to use a data-driven, multidisciplinary team effort to strengthen the utilization of the opportunity analysis process, embedding it into routine business operations.




