Guy's and St Thomas' NHS Foundation Trust faced coding challenges due to the need to review 380,000 episodes annually. To improve efficiency, the organisation combined and standardised data from various systems, leveraging technology to automate data gathering and enhance diagnostic coding for patients, easing the burden on clinical coders.
Responsible for coding approximately 380,000 episodes annually, clinical coders at Guy’s and St Thomas’ NHS Foundation Trust review documentation across several systems. The overwhelming amount of data, burdensome manual review processes, and limited coding resources made reviewing all data unfeasible. The consequence? Difficulty in assuring coding accuracy with a challenge to maintain appropriate payment for services rendered.
To address its coding challenges, Guy’s and St Thomas’ chose to leverage the Health Catalyst® Data Operating System (DOSTM) platform. DOS combines and standardises data across disparate source systems to provide actionable insights in a single technology platform. With improved access to accurate data, the organisation identified several opportunities where the data platform could be used to streamline and enhance the coders’ work—including automating the discovery of patients whose diagnostic coding could be improved.
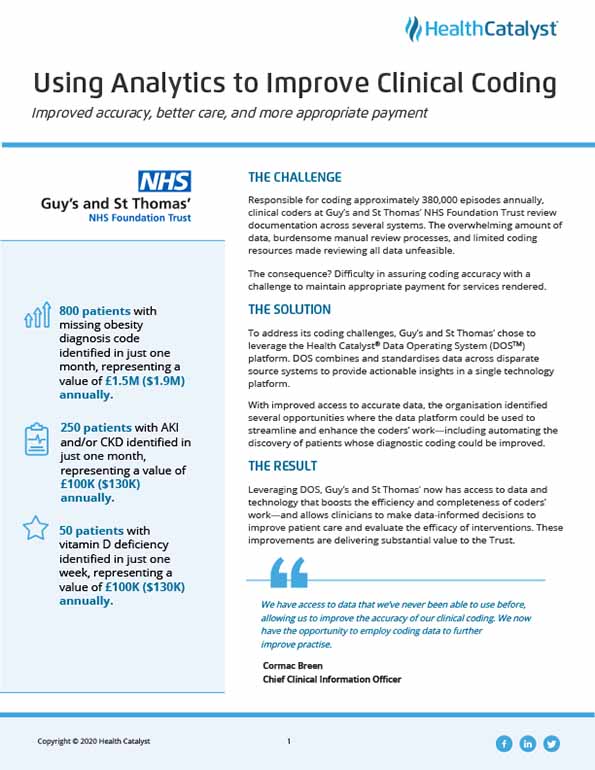
Leveraging DOS, Guy’s and St Thomas’ now has access to data and technology that boosts the efficiency and completeness of coders’ work—and allows clinicians to make data-informed decisions to improve patient care and evaluate the efficacy of interventions. These improvements are delivering substantial value to the Trust.
Precise clinical coding improves diagnostic recording and accuracy of clinical documentation, helping to ensure patients are treated more effectively. Suboptimal clinical coding can negatively impact payment, limiting the money available for patient care.1
Guy’s and St Thomas’ clinical coders process approximately 380,000 inpatient episodes per year, reviewing documentation in up to six unique sources to improve diagnostic recording and accuracy. Coders manually review data across these systems, including handwritten notes, computerised records, healthcare provider correspondence, clinical worksheets, nursing care pathways, diagnostic test reports, and discharge letters and forms.
The volume of sources, coupled with burdensome manual review processes and limited coding resources, limited coders’ ability to review every source for each patient, resulting in a gap in coding accuracy and potentially jeopardising appropriate payment for services rendered.
Guy’s and St Thomas’ needed a solution that would allow it to enhance the quality of medical records and the accuracy of its coding without increasing the number of coders or the documentation burden.
To enhance its coding process, Guy’s and St Thomas’ chose to leverage the Health Catalyst® Data Operating System (DOS™) platform. DOS combines and standardises data across source systems to provide actionable insights in a single technology platform, enabling the meaningful use of data.
With improved access to data, the organisation identified several opportunities where the data platform could be used to streamline and enhance the coders’ work—including automating the discovery of patients whose diagnostic coding could be improved. Guy’s and St Thomas’ prioritised potential use cases, selecting circumstances with clear clinical criteria that could be easily identified. This prompted the organisation to leverage the data platform to extract data and identify patients with missing diagnostic codes for obesity, vitamin D deficiency, and acute kidney injury (AKI)/chronic kidney disease (CKD).
To identify each group of patients, Guy’s and St Thomas’ worked with clinicians to design and approve the decision-making logic. For patients who are obese, the data platform extracts BMI documentation, locating patients with a BMI greater than 30. The BMIs are then matched to various episodes of care. The logic identifies if the patient is missing the diagnostic code for obesity, generating a list of patients for coders who then apply the diagnostic code.
Guy’s and St Thomas’ developed a similar workflow for vitamin D deficiency. The data platform gathers lab results using the decision-making logic approved by clinicians to identify patients with vitamin D deficiency. Coders are provided a list of patients with vitamin D deficiency criteria that do not have the associated diagnostic code, prompting bulk assignment of that code.
A larger number of criteria are used to identify patients with AKI and CKD. After collaborating with clinicians to identify the criteria that would result in the accurate identification of the patients, the team elected to use glomerular filtration rate, creatinine, and albumin to identify patients who may have AKI or CKD but who have not yet been coded with kidney disease. A tentative diagnosis of AKI or CKD is then sent to the clinical team for validation. Once validated, the coders assign the AKI or CKD diagnostic code.
Guy’s and St Thomas’ now have access to data and technology that augments coders’ work, automating data gathering to better identify patients whose diagnostic codes could be improved. Clinicians can now make data-informed decisions to improve patient care and evaluate the effectiveness of interventions on patient outcomes. These improvements are delivering substantial value to the Trust. Results include:
“We have access to data that we’ve never been able to use before, allowing us to improve the accuracy of our clinical coding. We now have the opportunity to employ coding data to further improve practice.”
– Cormac Breen, Chief Clinical Information Officer
Guy’s and St Thomas’ will continue to identify opportunities to augment clinical coding, improving diagnostic accuracy. The organisation plans to leverage technology to auto-populate diagnostic codes, further improving efficiency and accuracy.