The University of Kansas Hospital deployed an enterprise data warehouse to unify data for decision-making. Recognizing the need for trust in data, the organization implemented a data governance program with senior leadership support, established data definitions, assigned ownership, and created a multi-year roadmap to ensure a sustained focus on data quality and accessibility.
As healthcare transitions into an analytics-driven industry, data has become its most valuable asset—and one of the most challenging to manage. To support care delivery and other functions, health systems must integrate data from a complex array of internal applications including inpatient and ambulatory EHRs, laboratory information systems, pharmacy systems, and ERP systems. In a parallel need, these organizations must also pull data from affiliated providers’ EHR systems, payers, external laboratories, pharmacies and benchmarking sources. Good data governance practices are clearly essential for hospitals to ensure that all this data is well understood, trusted, accessible, and secure—particularly to validate the accuracy of dashboards, scorecards, and other analytic outputs in a data-driven setting. Further, establishing data governance practices now positions organizations for value-based care, another significant shift in the healthcare landscape in which timely access to trusted data is increasingly important.1
With an eye on creating such an environment, The University of Kansas Hospital has set an overarching goal to mature into an advanced analytics organization, capable of managing very large data sets and performing predictive analytics in pursuit of the best possible outcomes. To achieve these objectives, The University of Kansas Hospital required a “single source of truth” that users could rely on for quality data pulled from disparate sources and systems. While this could be accomplished in part with technology, they also needed to put in place a solid framework for data governance. In simplest terms, this is the management of data to keep it secure, available, usable and reliable, by a governing body that establishes procedures and execution plans.2
Certain data governance best practices have been identified that touch on a range of issues, from data stewardship to quality and availability.3 To put these and other best practices in place, such as active commitment and participation from senior leaders and tying data governance to a real world clinical or operational endeavor to realize the necessary level of engagement, The University of Kansas Hospital subsequently formed a data governance committee.
The University of Kansas Hospital faced several common data challenges for healthcare organizations, beginning with the amount of time required to manually collect, acquire and validate data from so many sources. This left staff with less time to actually study the data for improvement opportunities. As internal and external needs for information grew, the more expensive and inefficient this process became. It also became more difficult to get the right data in the hands of the right decision-makers. The Hospital needed a more efficient alternative, however, than just adding more full-time employees to manage this growing volume of data.
Data quality issues also regularly surfaced, illustrating the need for extensive clean-up of the different data sources. Non-standard data terms and definitions were among the most frequent problems, in addition to data that was inaccurate or missing altogether. Conflicting data was another challenge, such as the different values for length of stay that board members came across in two different reports. These and other discrepancies were often driven by the timing of when the information was produced, or differing data type definitions in different source systems.
The end result was that users didn’t fully trust the data. To overcome this distrust, The University of Kansas Hospital wanted to implement standard terms and definitions, and put in place better data management processes and practices. They also wanted to make data more accessible to clinical and operational end-users. Finally, they wanted to create a single source of truth for information that could take into account the many different people involved in data gathering and analysis and their varying degrees of training and experience.
To address the distrust in data, The University of Kansas Hospital implemented a data governance committee, sanctioned by senior leadership and provisioned with executive authority to govern all business intelligence, data and information assets. To keep up with its growing data reporting needs, rather than continuously adding full-time employees, The University of Kansas Hospital opted instead to invest in a modern analytics infrastructure. The chief features of such a solution significantly aid in the transformation to a data-driven culture.
To automate data collecting and reporting, the Hospital deployed a late-binding enterprise data warehouse and analytics applications from Health Catalyst.
From the outset, this committee made it clear that its purpose wasn’t to own data, but to facilitate its use for effective decision-making. To that end, the committee pursues four primary goals for data:
Information governance. This involves bringing clinical, administrative, and technology partners together to jointly design and optimize information assets in alignment with the organization’s strategies and goals. It also includes the declaration of sources of truth, systems of record, roles and responsibilities, information delivery standards and certified enterprise reports/dashboards. Data security and access decisions are within the scope of this governance.
Quality. Successful decision making is enabled by data that is complete, timely, accurate and consistent. The Committee assures data quality through standardization, process engineering and the creation and monitoring of data quality metrics.
Usability. Usability includes easy-to-use applications that promote data interaction and informed decision making, as well as creating a common data language for understanding organizational performance. Tools to create such usability include data dictionaries, training, a metadata repository, and access to trusted data sets as close to real-time as possible.
Availability. The Committee strives to implement the appropriate analytical infrastructure that makes data accessible to clinical and operational users when they need it, defined by their respective clinical and operational needs.
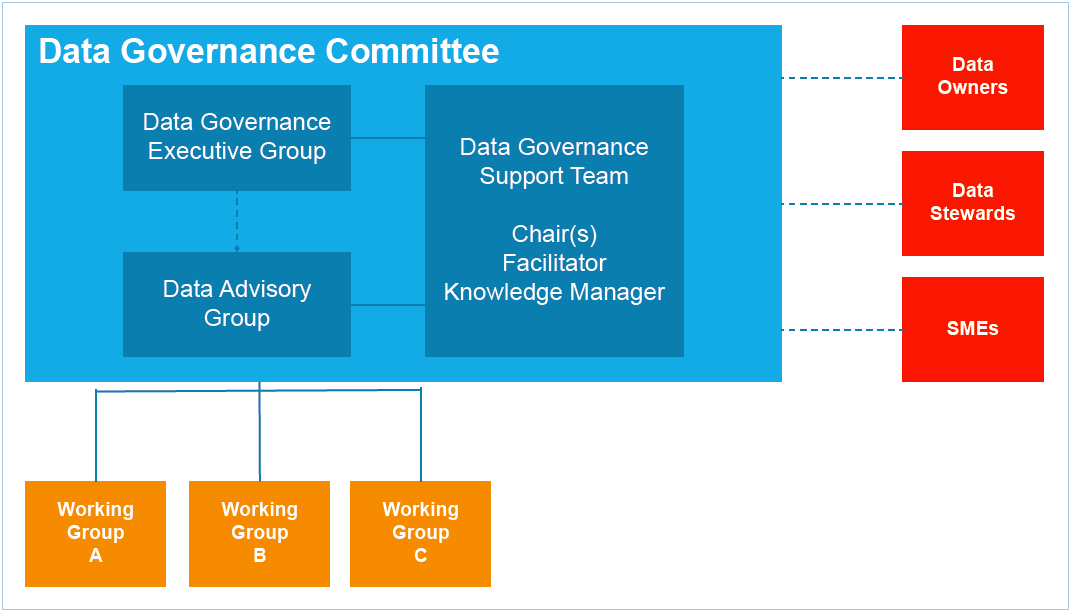
As illustrated in Figure 1, this committee is segmented into different groups with specific responsibilities. Overseeing vision and strategy for improvement efforts is the Data Governance Executive Group, while the Data Advisory Group functions at a more tactical level and addresses data quality issues, work priorities and the creation of working groups. Working groups are composed of subject matter experts in the domain the group is formed to study. Other key committee members include the Data Governance Support Team, made up of technology, process improvement and clinical experts.
To avoid the mistakes that can lead to an unsuccessful data governance program, The University of Kansas Hospital devised and implemented a number of best practices to build a solid data governance structure that would serve the hospital for years to come.
With a solution comprised of intelligent technology and prudent best practices, The University of Kansas Hospital achieved its primary goals while further transforming into an analytics-driven culture.
70+ standardized enterprise data definition approvals planned for completion in first year. The organization approved seven definitions in the first quarter to more than 66 in the second quarter— averaging four decisions per months, and growing. End-users are assuming ownership of the data and accepting responsibility to manage data quality. A number of data quality issues have been fixed and improved data quality. In turn, trust in the data has grown among end-users.
Systemwide executive and clinical engagement in data governance. Due in no small part to an executive team that has been visibly and strongly supportive of the Data Governance Committee, and provided it with the necessary resources, two important events have happened. First, the committee has assumed overall responsibility for managing the availability, usability, integrity, and security of the organization’s data. Second, key clinical and operational leaders are becoming more engaged in the analytics and improvement efforts, with participation rates increasing to 60 percent in bi-monthly governance meetings.
Creation of a multi-year business intelligence/data governance roadmap. The University of Kansas Hospital is moving from a fragmented business intelligence environment to the more cohesive enterprise perspective ideal for managing large data sets and using predictive analytics to create the best outcomes. In support of this journey, they have developed a business intelligence roadmap (illustrated in Figure 2) against which they track their progress. The Data Governance Committee is focused on making progress on several fronts including:

"Data is critical to making informed decisions. A data governance structure makes sure that the data is accurate and that we are all telling the same story."
– Chris Harper, Director Business Architecture & Analytics
The University of Kansas Hospital sees data governance as a critical component of a successful data-driven culture. As such, focus will remain on building the most successful data governance program possible. The Hospital plans to build a data governance dashboard, for example, to track and manage governance metrics. Future metrics under consideration include the number of data owners identified, the number of processes documented, the number of dollars saved (or expenses avoided) and usage of the enterprise data warehouse (such as efficiencies gained, reduction in usage of non-enterprise data solutions, and measuring the value of applications to assure customers are using the business intelligence solutions that have been developed).
A sustained focus on data quality and accessibility to facilitate trust and usage is also ongoing. Elements include:
With such a commitment to data integrity and usability in place, The University of Kansas Hospital is well-positioned not only to perform analytics in the pursuit of improved outcomes, but to lead the way.